Kamagra gibt es auch als Kautabletten, die sich schneller auflösen als normale Pillen. Manche Patienten empfinden das als angenehmer. Wer sich informieren will, findet Hinweise unter kamagra kautabletten.
Ojo_feb_09.indd
[Downloaded free from http://www.ojoonline.org on Saturday, February 28, 2009]
Original Article
Collagen cross-linking with riboflavin and ultraviolet-A light
in keratoconus: One-year results
Maria Clara Arbelaez, Maria Bernardita Sekito, Camila Vidal, Sanak Roy Choudhury
Muscat Eye Laser Center, Muscat, Oman
Background: The aim of this study is to evaluate the
pachymetry, posterior and anterior elevations from
safety and effectiveness of riboflavin-ultraviolet type
Pentacam and corneal aberrations at 6 months and 1
A (UV-A) light rays induced cross-linking of corneal
collagen in improving visual acuity and in stabilizing the progression of keratoconic eyes. The method of
Results: Comparative analysis of the pre-operative and
corneal cross-linking using riboflavin and UV-A light
1 year post-operative evaluation showed a mean gain of
is technically simple and less invasive than all other
4.15 lines of UCVA (
P = 0.001) and 1.65 lines of BCVA
therapies proposed for keratoconus. It is the only
(
P = 0.002). The reduction in the average keratometry
treatment that treats not only the refractive effects of
reading was 1.36 D (
P = 0.0004) and 1.4 D (
P = 0.001)
the condition but the underlying pathophysiology.
at the apex. Manifest refraction sphere showed a mean reduction of 1.26 D (
P = 0.033) and 1.25 D (0.0003) for
Materials and Methods: In this prospective, manifest cylinder. Topo-aberrometric analysis showed nonrandomized clinical study, 20 eyes of 19 patients
improvement in corneal symmetry.
with keratoconus were treated by combined riboflavin
Conclusion: Cross-linking was safe and an effective
UV-A collagen cross linking. The eyes were saturated
therapeutical option for progressive keratoconus.
with riboflavin solution and were subjected for 30 min under UV-A light with a dose parameter of 3 mW/cm2.
Keywords: Corneal scarring, cross-linking, irregular
Safety and effectiveness of the treatment was assessed by
measuring the uncorrected visual acuity, best corrected visual acuity, manifest cylinder/sphere, keratometry,
Oman Journal of Ophthalmology, 2009; 2(1):33-38
intermarriage with a second- or third-degree relative is a common practice.
Keratoconus is a progressive, noninflammatory, bilateral (but usually asymmetrical) disease of the cornea, Spectacles and contact lenses are the usual treatment characterized by paraxial stromal thinning that leads
modalities in the early stages of keratoconus. As the
to corneal surface distortion.[1] The thinning and the
disease advances, severe corneal astigmatism and stromal
protrusion in keratoconus induces irregular astigmatism,
opacities develop to the point where contact lenses can no
myopia and scarring resulting in visual loss and mild to
longer provide useful vision and penetrating keratoplasty
marked impairment in the quality of vision. Among the risk
(PKP) becomes necessary to restore visual function.
factors of this condition is genetics, usually inherited in an
Penetrating keratoplasty is the most commonly performed
autosomal dominant fashion.[2] This could partly explain
surgical procedure for keratoconus, but is associated with
why keratoconus is a relatively common corneal disease
complications including graft rejection.[3] It is estimated
entity in the gulf countries particularly in Oman where
that eventually 21% of the keratoconus patients require
Copyright: 2009 Soliman Mahdy MAE. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Correspondence:
Maria Clara Arbelaez, Muscat Eye Laser Center, P.O. Box 938 PC 117 Muscat, Oman. E-mail:
[email protected],
DOI: 10.4103/0974-620X.48420.
Oman Journal of Ophthalmology, Vol. 2, No. 1, 2009
[Downloaded free from http://www.ojoonline.org on Saturday, February 28, 2009]
Arbelaez
et al.: Collagen cross-linking in keratoconus
surgical intervention (PKP) to restore corneal anatomy and
The surgical procedure consisted of topical anesthesia (instillation of oxybuprocaine 0.4% eye drops) and then
In selected cases wherein the cornea is still transparent and
manual epithelial abrasion of 6–8 mm using 17% ETOH for
in relatively young patients who are reluctant to pursue PKP,
20–40 s. This was done to ensure penetration of riboflavin
less invasive surgical interventions may be resorted to and
in the stroma and that a high level of UV-A absorption
these are lamellar keratoplasty (LKP)[5-7] and intrastromal
was achieved. Riboflavin solution was repeatedly placed
corneal ring segments (Intacs). LKP has the advantages of
every 3 min for 30 min to allow sufficient saturation in
being extraocular, reversible if tissue complications occur
the stroma. This was inspected by slit lamp examination
and has the ability to replace only selected areas of diseased
as fluorescence within the anterior chamber. Then the
corneal tissue with healthy donor tissue.[8] Intacs, which
cornea was irradiated with UV-A light at 365 nm with a
were initially used to correct low myopia, have been shown
dose parameter of 3 mW/cm2 for 30 min (UV-X device).
to improve vision in keratoconus[9,10] and post-LASIK
During the treatment, riboflavin solution was applied every
5 min to saturate the cornea and drops of BSS every 2 min to moisten the cornea. After the treatment, the cornea was
Results of the currently available treatments for keratoconus
irrigated with 20-ml BSS solution and an antibiotic drop
(rigid contact lens, LKP and Intacs) are viable and are
was instilled. Contact lens was placed after the treatment.
considered logical addition to the stepwise treatment of keratoconus for the improvement of vision. However,
there is a new procedure that addresses primarily the
Antibiotic eye drops (ofloxacin) and Pranoprofen
pathophysiology of keratoconus and this is riboflavin UV-A
0.1% E/D were applied for one week until complete
rays induced cross-linking. Cross-linking of the cornea is
re-epithelializationwas achieved. After the cornea has
a procedure that can increase the ties or chemical bonds
completely healed, the contact lens is removed. Efemoline
between the fibers of the corneal collagen by means of a
eye drops and artificial tears were applied for approximately
highly localized photo-polymerization using UV-A light and
a photosensitizer riboflavin drops. [13,14] Riboflavin (Vitamin B2) has a dual function of acting as a photosensitizer for
Outcome measures and statistical analysis
the production of oxygen free radicals, which induce
Follow-up examination was done at 3, 6, and 12 months
physical cross linking of collagen, and it gives a "shielding
post-treatment. At each examination, uncorrected visual
effect" by absorbing the UV-A irradiation (90%), thereby
acuity, best corrected visual acuity, refraction, keratometry,
preventing damage to deeper ocular structures. UV-A light
corneal topography, pachymetry and corneal aberrations
of 370 nm wavelength at 3 mW/cm2 allows approximately
were recorded. SPSS statistical software was used for
95% of the UV light to be absorbed into the cornea; thus
statistical analysis.
there is no risk for damage to the lens and retina. Collagen cross-linking is the only treatment that deals with not only
the refractive effects of the condition but the underlying pathophysiology. The aim of this study is to evaluate the
Twenty keratoconic eyes of 19 patients were included in
safety and effectiveness of riboflavin UV-A light-induced
the study. All patients completed 1 year and presented with
cross-linking of corneal collagen in improving visual acuity
moderate to severe keratoconus. Fourteen patients were
and in stabilizing the progression of keratoconic eyes.
men and 5 were women. The mean age was 24.4 years (range: 18–44 years).
Materials and Methods
Table 1 shows the pre-operative and postoperative findings
This prospective longitudinal study comprised patients with
in all patients. The surgery and the postoperative period
signs of progressive keratoconus defined as an increase in
were unremarkable in all patients. The epithelium re-
maximum K readings in several consecutive measurements
epithelialized one week after the treatment. In the early
over a period of 3 to 6 months, changes in refraction, patient
post-operative period, all eyes had minimal anterior stromal
reports of deteriorating visual acuity and contact lens
corneal haze which resolved approximately 3 months post-
intolerance. All of the patients had bilateral keratoconus
operatively. After 6 months from the treatment, patients
without sub-epithelial scarring, were older than 18 years
were given the option to wear contact lenses or to undergo
old, with a corneal thickness of at least 400 µm. The eye
intrastromal corneal ring surgery if necessary.
with the more advanced stage of keratoconus was treated. The institutional ethics committee approved the study, and
Visual acuity
all patients were asked to sign an informed consent.
Visual acuity was measured using the decimal equivalent
Oman Journal of Ophthalmology, Vol. 2, No. 1, 2009
[Downloaded free from http://www.ojoonline.org on Saturday, February 28, 2009]
Arbelaez
et al.: Collagen cross-linking in keratoconus
Table 1: Comparison between mean preoperative, six months and one year postoperative data
Parameter
Pre-operative Mean ± SD
Post-op 6 months Mean ± SD
Post-op 1 year Mean ± SD
1.18 (20/320) ± 0.69
0.63 (20/80) ± 0.32
0.55 (20/70) ± 0.32
0.40 (20/50) ± 0.43
0.24 (20/30) ± 0.19
0.22 (20/30) ± 0.17
Manifest refraction sphere (D)
Manifest refraction cylinder (D)
UCVA-uncorrected visual acuity; BCVA- best corrected visual acuity; D = diopters; In logMAR values (Snellen acuity). SD = standard deviation
and transformed into logarithm of the minimum angle
manifest refraction sphere at 1 year as compared with the
of resolution (logMAR) for further statistical analysis
pre-operative evaluation. The mean value of the manifest
as recommended by Holladay.[15] Visual acuity data is
refraction cylinder was utilized as a measure of the change
expressed as logMAR ± standard deviation (Snellen value).
in the refractive astigmatism. The cylinder values at 1-year
Table 1 provides the uncorrected visual acuity (UCVA) for
examination were statistically significantly less than the
all patients at the pre-operative, 3 months and 6 months
pre-operative measurements (
P = 0.0003).One year after
examination and Figure 1 shows the change in UCVA
the cross-linking treatment, manifest sphere decreased by
between the postoperative and one-year examinations. Two
a mean of –2.75 D in 13 eyes (65%), and no improvement
eyes maintained the preoperative UCVA; seven eyes gained
in 7 eyes (35%). Manifest cylinder decreased by a mean of
one to two lines, and five eyes gained three to five lines and
–1.68 D in 15 eyes (75%) and no change in 5 eyes (25%).
six eyes gained more than five lines. There was a mean gain of 4.15 lines of UCVA from preoperative to the last follow-
The K value at the apex decreased by a mean of 1.40 D from pre-operative to 1-year evaluation,
P = 0.01.The K average
The best corrected visual acuity (BCVA) data from the
decreased by a mean of 1.36 D from pre-operative to 1-year
study eyes at the pre-operative and 3 and 6 months post-
evaluation,
P=0.004. Table 1 and Figure 3 describes the
operative examinations are shown in Table 1. There was a
change in K average and K value at the apex from pre-
statistically significant (
P = 0.002) improvement in BCVA
operative value to 1 year.
between the pre-operative and 1-year evaluations. The change in BCVA lines gained or lost at 1 year compared
with the pre-operative baseline is presented in Figure 2.
Pachymetry measurements (measured by the Pentacam)
Of the 20 eyes evaluated at 1 year, 12 of 20 eyes (60%)
at the thinnest location and at the apex were measured
experienced at least a gained of 1–5 lines of BCVA. Eight of
pre-operatively, 3-months, 6-months and 1-year post-
the 20 eyes (40%) experienced no change in BCVA.
operatively. At 3-months post-operative examination, there was a significant reduction in pachymetry both at the
thinnest location (
P = 0.0007) and at the apex (
P = 0.0002).
Table 1 shows the improvement in manifest refraction
Pachymetry at the thinnest location reduced from 452.25
±
sphere at the pre-operative, 6-month and 1-year evaluations.
29.58 µm pre-operatively to 430.4
± 44.38 µm at 3 months
There was a statistically significant (
P = 0.033) change in
(4.83% reduction). At the apex, there was also a significant
1-2 lines gained n = 7
3-5 lines gained n = 5
>5 lines gained n = 6
1-2 lines gained n = 7
3-5 lines gained n = 5
>5 lines gained n = 6
UCVA = uncorrected visual acuity
BCVA = Best corrected visual acuity
Figure 1: Change in UCVA from preoperative status to status 1 year following cross-
Figure 2: Change in BCVA from preoperative status to status 1 year following cross-
Oman Journal of Ophthalmology, Vol. 2, No. 1, 2009

[Downloaded free from http://www.ojoonline.org on Saturday, February 28, 2009]
Arbelaez et al.: Collagen cross-linking in keratoconus
Pachymetry (thinnest location, um)
Pachymetry (apex, um)
Figure 4: Changes in pachymetry measurements (µm) at the thinnest location and at
the apex
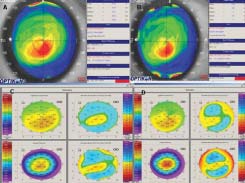
Figure 3: Corneal topography of a patient who had cross-linking in the right eye. A:
Preoperative UCVA: –0.70 (20/100), BCVA: –0.10 (20/25), K max at the apex = 47.78.
B: 1 year after cross-linking, UCVA: –0.20 (20/30), BCVA: –0.10 (20/25), K max at the
apex = 45.86, K average = 44.64. C: Pentacam pre-operative, anterior elevation = +17
were measured pre-operatively, 6-months and at 1-year post-
µm, posterior elevation = +27 µm. D: 1 year after cross-linking, reduction in anterior
treatment by the Oculus Pentacam. There was a significant
elevation = +4 µm and posterior elevation = +17 µm.
reduction in anterior elevation both at the thinnest location and at the apex at 6 months post-treatment. At the thinnest location, the anterior elevation decreased significantly, P
= 0.015, from 31.25 ±17.06 D pre-operatively to 26.35 ±
16.63 D at 6 months post-treatment. No significant change
was noted at 1 year post-treatment. At the apex, the anterior
elevation decreased significantly,
P = 0.025, from 21.05 ±
15.55 pre-operatively to 17.0 ± 15.37 D at 6 months post-
treatment. No significant change was noted at 1 year post-
SPHERICAL ABERRATION
Student's t test for paired data did not find any significant
difference in the posterior eleavation at the thinnest location
and at the apex from pre-operative value, at 6 months and
at 1 year post-treatment. Table 2 and Figure 3 present the changes in anterior and posterior elevation at the thinnest location and at the apex over time.
Figure 5: Corneal wavefront analysis with 4-mm pupil; blue arrows indicate (paired t
tests) signifi cant difference with preoperative data
decline from 463.96 ± 27.28 µm pre-operatively to 439.25
± 42.80 µm at 3 months (5.32% reduction). One-year
The goal for the corneal collagen cross-linking treatment
evaluation showed the pachymetry to increase gradually to
is to delay or halt the progression of keratoconus and to
455 ± 37.98 at the thinnest location and 463.95 ± 37.36
defer the need for a corneal transplant. The results of this
at the apex. Figure 4 shows the changes in pachymetry
study were encouraging as far as safety and effectiveness
measurement at the thinnest location and at the apex in
are concerned. No side effects were noted except for the
subjective complaints of patients, namely, visual symptoms like fluctuating vision and double images. Although no
Corneal wavefront surface aberrometry
survey was used in the study, patients anecdotally reported
Corneal wavefront surface aberommetry showed a significant
improvement in visual symptoms over time.
reduction in absolute RMS (P = 0.041) and absolute coma (P = 0.026) at 1 year with respect to the pre-operative value
Refractive results in this study were approximately similar to
[Figure 5]. Spherical and other high-order aberrations did
other studies published.[16,17,18] There was a 1.25-D reduction
not show any significant change.
in the manifest sphere and cylinder as confirmed by the reduction in the keratometry readings. This reduction in
Anterior and posterior elevation
refractive error is also associated with a significant increase
Anterior elevation at the thinnest location and at the apex
in UCVA (4 Snellen lines).
Oman Journal of Ophthalmology, Vol. 2, No. 1, 2009
[Downloaded free from http://www.ojoonline.org on Saturday, February 28, 2009]
Arbelaez et al.: Collagen cross-linking in keratoconus
Table 2: Anterior surface and posterior surface elevation change at the thinnest location and at
the apex from pre-operative, 6 months and one year post evaluation as measured by the 0cuius
Pentacam
Anterior elevation, thinnest location (D)
Anterior elevation, apex (D)
Posterior elevation, thinnest location (D)
Posterior elevation, apex (D)
Corneal wavefront surface aberrometric analysis reflected a
corneal collagen cross linking has the potential to become a
significant reduction in RMS and comatic aberrations. This
standard therapy for progressive keratoconus in the future.
could partly explain the improvement in the BCVA in 60%
Particularly in Oman, this treatment could benefit a lot
of the patients.
of people due to the fact that there are very few centers that are capable of performing corneal transplant and the
In a study made by Wollensak et al,[19] it was shown that
environment is not suitable for contact lens wear. However,
apoptotic cell death occurs after exposure to UV-A light.
as with all new treatment modalities, controversies and
The massive, transient cellular damage or keratocyte
questions remain unanswered. Long-term results are
apoptosis is assumed to be an initiator of the corneal wound
necessary to evaluate the duration of the stiffening effect,
healing response and the start of the complex wound
indications and contraindications must be investigated,
healing cascade.[20] In the present study, a 5% reduction in
hence, the need for long term longitudinal studies.
pachymetry was observed in all patients at 3 months. After which, a steady increase was noted. This finding could
correspond to the apoptosis that occurs after the treatment (2 to 3 months) and the repopulation that occurs thereafter
Rabinowitz YS. Keratoconus. Surv Ophthalmol 1998;42:297-319.
(6 months). Based on this finding, the authors strongly
Rabinowittz YS. The genetics of keratoconus. Opthalmol Clin North Am
suggest that when the cross-linking treatment is combined
Thompson RW Jr, Price MO, Bowers PJ, Price FW Jr. Long term graft
with an additional treatment such as Intacs or LASEK, a
survival after penetrating keratoplasty. Ophthalmology 2003;110:1396-
healing interval of approximately 2 to 3 months should be
respected to avoid complications caused by the additional
Waller SG, Steinert RF, Wagoner MD. Long-term results of epikeratoplasty
damage of the added procedure.
for keratoplasty for keratoconus. Cornea 1995;14:84-8
Tan BU, Purcell TL, Torres LF, Schanzlin DJ. New surgical approaches
In the present study, a significant reduction in the anterior
to the management of keratoconus and post-lasik ectasia Trans Am Ophthalmol Soc 2006;104:212-20.
elevation was noted but the reduction in posterior
Bilgihan K, Ozdek SC, Sari A, Hasanreisoglu B. Microkeratome-assisted
elevation was not statistically significant. The studies in
lamellar keratoplasty for keratoconus: Stromal sandwich. J Cataract
animal experiments[21,22] and in humans[23,24] may provide
Refract Surg 2003;29:1267-72.
an insight to this finding. These studies have shown
Shimazaki J, Shimmura S, Ishioka M, Tsubota K. Randomized clinical trial
that treatment of the cornea with riboflavin and UV-A
of deep lamellar keratoplasty vs penetrating keratoplasty. Am J Ophthalmol 2002;134:159-65.
significantly stiffened the cornea only in the anterior 300
8. Alio JL, Shah S, Barraquer C, Bilgihan K, Anwar M, Melles GR.
µm. This depth dependent stiffening effect may explain
New techniques in lamellar keratoplasty. Curr Opin Ophthalmol
significant flattening in the anterior cornea as revealed by
the reduction in the anterior elevation.
Kanellopoulos AJ, Pe LH, Perry HD, Donnenfeld ED. ModiÞ ed intracorneal ring segment implantations (INTACS) for the management of moderate to advanced keratoconus: EfÞ cacy and complications. Cornea 2006;25:29-
It has been shown that collagen cross-linking increases the
biomechanical rigidity of the cornea by 4.5 times.[21] By
10. Joseph Colin, MD, European clinical evaluation: Use of intacs for the
increasing the biomechanical stability of the cornea using
treatment of keratoconus, J Cataract Refract Surg 2006;32:747-55.
the riboflavin and UV-A-induced collagen cross-linking,
11. Pokroy R, Levinger S, Hirsh A. Single Intacs segment for post-LASIK
it is possible to stop the progression of keratoconus. The
keratectasia. J Cataract Refract Surg 2004;30:1685-95.
12. Boxer Wachler BS, Christie JP, Chandra NS, Chou B, Korn T, Nepomuceno
improvement in vision, reduction in the refractive effect,
R. Intacs for keratoconus. Ophthalmology 2003;110:1031-40.
reduction in keratometry readings, improvement in the
13. Wollensak G. Crosslinking treatment of progressive keratoconus: New
topographic and surface aberrometric analysis are all
hope. Curr Opin Ophthalmol 2006;17:357-60
evidences that the treatment can arrest the progression of
14. Wollensak G, Spoerl E, Seiler T. Riboß avin/ultraviolet-A-induced
keratoconus. No analysis of the fellow eye was done in this
collagen crosslinking for the treatment of keratoconus. Am J Ophthamol
study; such analysis is indicated in the future.
15. Holladay JT. Visual acuity measurements. J Cataract Refract Surg
Given the effectiveness, simplicity, safety and cost 16. Caporossi A, Baiocchi S, Mazzotta C, Traversi C, Caporossi T. Parasurgical effectiveness (this is a one-time treatment) of this modality,
therapy for keratoconus by riboß avin-ultraviolet type A rays induced cross-
Oman Journal of Ophthalmology, Vol. 2, No. 1, 2009
[Downloaded free from http://www.ojoonline.org on Saturday, February 28, 2009]
Arbelaez et al.: Collagen cross-linking in keratoconus
linking of corneal collagen: Preliminary refractive results in an Italian study.
and porcine corneas after riboß avin-ultraviolet-A-induced cross-linking. J
J Cataract Refract Surg 2006;32:837-45.
Cataract Refract Surg 2003;29:1780-5.
17. Mazzotta C, Traversi C, Baiocchi S, Sergio P, Caporossi T, Caporossi A.
22. Wollensak G, Spoerl E. Collagen crosslinking of humanand porcine sclera.
Conservative treatment of keratoconus by riboß avin-UV-A-induced cross-
J Cataract Refract Surg 2004;30:689-95.
linking of corneal collagen: Qualitative investigation. Eur J Ophthalmol
23. Mazzotta C, Balestrazzi A, Traversi C, Baiocchi S, Caporossi T, Tommasi
C, et al. Treatment of progressive keratoconus by riboß avin-UV-Ainduced
18. Chan CCK, Charma M, Boxler Wachler BS. Effect of inferior-segment
cross-linking of corneal collagen: Ultrastructural analysis by Heidelberg
Intacs with and without C3R on keratoconus. J Cataract Refract Surg
Retinal Tomograph II in vivo confocal microscopy in humans. Cornea
19. Wollensak G, Spoerl E, Reber F, Seiler T. Keratocyte cytotoxicity of
24. Seiler T, Hafezi F. Corneal cross-linking-inducedstromal demarcation line.
riboß avin/UV-A treatment in vitro. Eye 2004;18:718-22.
20. Wollensak G, Iomdina E, Herbst H, Wound healing in the rabbit after corneal
collagen cross linking with riboß avin and UV-A. Cornea 2007;26:600-5.
Source of Support: Nil, Conflict of Interest: None
21. Wollensak G, Spoerl E, Seiler T. Stress-strain measurements of human
Accreditation of Oman Journal of Ophthalmology
CME Credits
The Directorate General of Education and Training, Ministry of Health, Muscat, Oman has announced the award of Category 2 CME credits to local authors and reviewers of the Oman Journal of Ophthalmology.
3 credits per publication
2 credits per publication
Third Author and beyond
1 credit per publication
1 credit per paper
Oman Journal of Ophthalmology, Vol. 2, No. 1, 2009
Source: http://www.c-dat.co/muscateye/about/publications/files/04_OmanJOphth%20Collagen%20cross-linking%20Vol%201%202009.pdf
Inlacin® Therapy in Patients with Type-2 Diabetes Mellitus (The Prospective Surabaya-Inlacin® Study) Askandar Tjokroprawiro Sri Murtiwi Surabaya Diabetes and Nutrition Center – Dr. Soetomo Teaching Hospital Faculty of Medicine Airlangga University, Surabaya Prospective study on DLBS3233 (Inlacin®) which is called Surabaya-Inlacin® Study (SIS) has been per-
BETH TIKVAH C H A I L I G H T S PURIM 5776 MARCH 2016 FROM OUR RABBI There is a Jewish expression that says- "With the arrival of the comes to replace another one, until the other one comes back Jewish month of Adar, our happiness is greatly increased!" to replace the new one. And so on, and so on! The reference to "greatly increased happiness" is a reference to The story is told of a new rabbi officiating at his first religiousthe holiday of Purim celebrated on the 14th of Adar.