Kamagra gibt es auch als Kautabletten, die sich schneller auflösen als normale Pillen. Manche Patienten empfinden das als angenehmer. Wer sich informieren will, findet Hinweise unter kamagra kautabletten.
Primary sclerosing cholangitis
THE NEW ENGLAND JOURNAL OF MEDICINE
Nevertheless, in addition to medical therapy, a varietyof endoscopic, radiologic, and surgical procedures have
been used to relieve the mechanical obstruction of thebile ducts that the disease produces. The availability ofliver transplantation has also greatly improved pa-tients' prospects for long-term survival.
PRIMARY SCLEROSING CHOLANGITIS
OUNG-MEE LEE, M.D.,
AND MARSHALL M. KAPLAN, M.D.
Thickening and induration of the common bile duct,
seen at laparotomy, are characteristic of primary scle-
PRIMARY sclerosing cholangitis, a chronic chole- rosing cholangitis.32 In early stages of the disease, the
static liver disease of unknown cause, is character-
liver may appear grossly normal. However, as the con-
ized by ongoing inflammation, destruction, and fibro-
dition progresses, the liver becomes coarsely nodular
sis of intrahepatic and extrahepatic bile ducts.1-4 Over
and stained with bile.
time, bile ducts become irregularly narrowed and oblit-
Four histologic stages of primary sclerosing cholan-
erated, and small intrahepatic ducts disappear. Focal
gitis have been identified.32 Stage 1 represents the ini-
bile-duct dilatation proximal to areas of stricture pro-
tial lesion; the other stages presumably develop with
duces a characteristic beaded appearance on cholan-
time and the progression of the disease. Stage 1 is char-
giography.5,6 Primary sclerosing cholangitis, although
acterized by the degeneration of epithelial cells in the
only about 1 percent as common as alcoholic liver
bile duct and by infiltration of the bile duct by lympho-
disease,7,8 is the fourth leading indication for liver
cytes and, occasionally, neutrophils. There is inflamma-
transplantation in adults in the United States.9 The dis-
tion, scarring, and enlargement of the portal triads
ease progresses silently, but relentlessly, in most pa-
and, at times, portal edema. At stage 1, however, these
tients and leads to cirrhosis, portal hypertension, and
findings are not present outside the portal triads (Fig.
liver failure.10,11
1A and 1B). In some cases, there may be proliferation
Seventy percent of patients with primary sclerosing
of bile ducts in the portal triads, vacuolation of ductu-
cholangitis are men, and the mean age at diagnosis is
lar epithelial cells, and the formation of onionskin le-
39 years.12 The disease typically occurs in patients with
sions, concentric layers of connective tissue surround-
inflammatory bowel disease, but it may also occur alone
ing bile ducts (Fig. 1C and 1D).33 Primary sclerosing
or in association with retroperitoneal or mediastinal fi-
cholangitis typically involves less inflammation in the
brosis.13 Of the approximately 75 percent of patients
portal triads than other chronic cholestatic liver diseas-
with primary sclerosing cholangitis who have inflam-
es, such as primary biliary cirrhosis. In stage 2, the le-
matory bowel disease, about 87 percent have ulcerative
sion is more widespread. The fibrosis and inflammation
colitis and 13 percent Crohn's disease.14-21 Seen anoth-
infiltrate the periportal parenchyma, where they even-
er way, 2.5 to 7.5 percent of patients who present with
tually destroy periportal hepatocytes in piecemeal ne-
ulcerative colitis have, or will have, primary sclerosing
crosis. Portal triads are often enlarged. Bile ductopenia
cholangitis.22-24 The true frequency of primary scleros-
is a prominent feature; concentric periductal fibrosis is
ing cholangitis in patients with ulcerative colitis may
less obvious. As the disease progresses to stage 3, por-
actually be higher. Some patients who, in fact, have pri-
tal-to-portal fibrous septa form. Bile ducts disappear
mary sclerosing cholangitis may not undergo cholangi-
or undergo severe degenerative changes. Cholestasis
ography because they are asymptomatic and the results
may be prominent, primarily in periportal and para-
of their biochemical tests of liver function are only min-
septal hepatocytes. Stage 4, the end stage, is charac-
imally abnormal. The prevalence of ulcerative colitis in
terized by frank cirrhosis; the histologic features dif-
the United States is estimated to range from 40 to 225
fer little from those seen in other forms of that disease.
per 100,000.25,26 On the basis of this figure, the preva-
In primary sclerosing cholangitis, however, there may
lence of primary sclerosing cholangitis would be ap-
also be changes associated with large-duct obstruction:
proximately 1 to 6 cases per 100,000.
the proliferation and dilatation of interlobular bile
At the present time, there is no effective treatment
ducts and increased numbers of periportal neutrophils
for the disease.4 Preliminary data on drugs such as
ursodiol27-29 and methotrexate30,31 show improved re-
It is noteworthy that the pathognomonic sign of
sults in biochemical tests of liver function, particularly
primary sclerosing cholangitis — the onionskin le-
decreases in serum alkaline phosphatase levels, as well
sions — is rarely seen on percutaneous biopsy of the
as occasional improvement in symptoms. However,
liver. It is more common to find only a paucity of nor-
there are no data to show that these drugs can favor-
mal bile ducts and nonspecific fibrosis and inflamma-
ably alter the course of primary sclerosing cholangitis.
tion in the portal triads. The diagnosis is thereforeusually made by cholangiography. Histologic exami-nation of the liver is used for confirmation and to de-
From the Division of Gastroenterology, New England Medical Center, 750
termine the stage of disease. Since the progress and
Washington St., Boston, MA 02111, where reprint requests should be addressedto Dr. Kaplan.
extent of the disease seen in biopsy tissue may vary,
The New England Journal of Medicine
Downloaded from nejm.org on April 22, 2013. For personal use only. No other uses without permission.
Copyright 1995 Massachusetts Medical Society. All rights reserved.
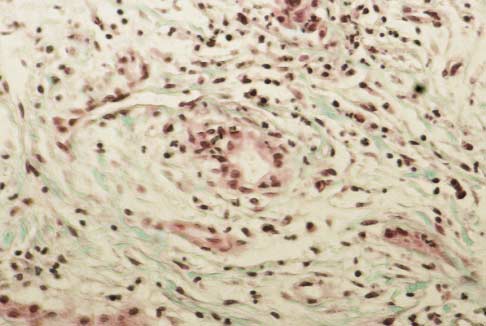
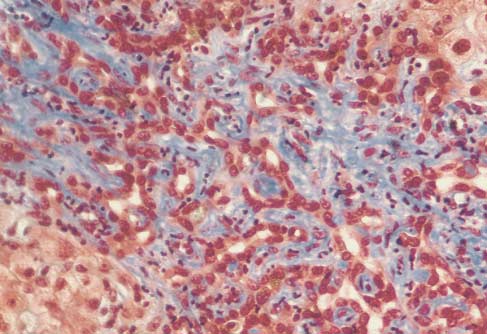
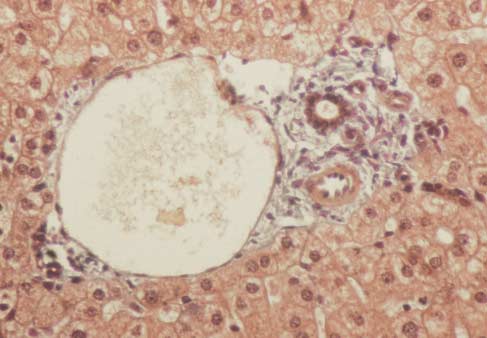
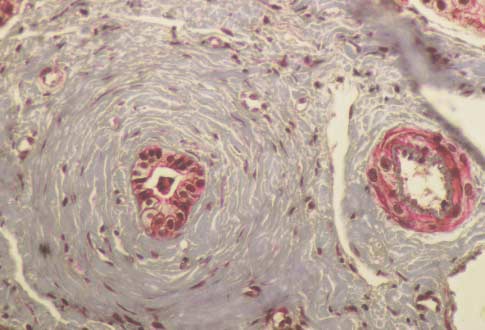
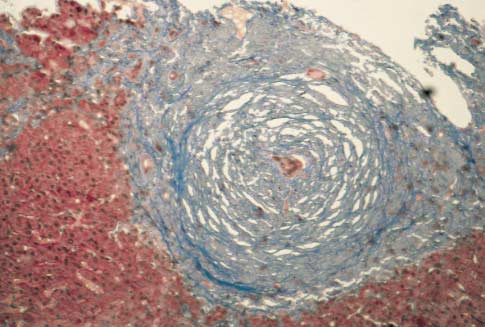
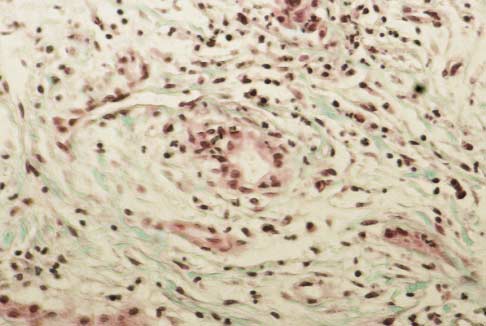
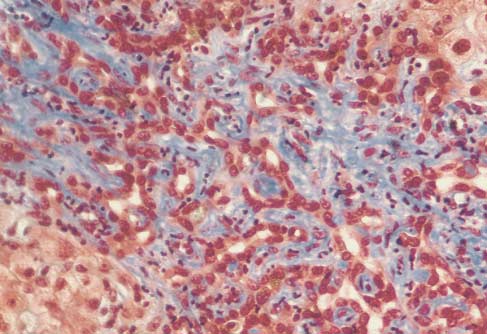
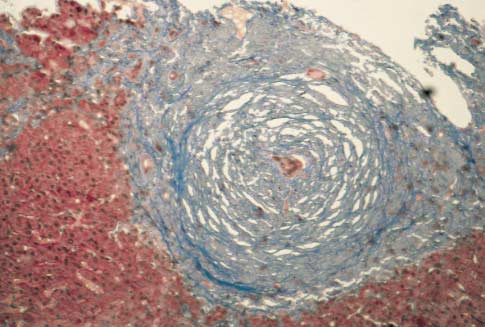
Figure 1. Lesions in Primary Sclerosing Cholangitis.
Panel A shows acute bile-duct injury in a patient with early stage1 disease. The bile duct at the center is infiltrated with neutro-phils and lymphocytes. Epithelial cells are damaged. There areloosely arrayed concentric rings of connective tissue, separatedby clear zones of edema and inflammatory cells that surroundthe damaged bile duct. Panel B shows a stage 1 lesion. A bileduct contains vacuolated, degenerating epithelial cells and is in-filtrated by lymphocytes. The duct is surrounded by concentricrings of connective tissue with scant lymphocytic infiltrate. An ar-teriole is visible on the right. Panel C shows a stage 2 lesion. Anecrotic bile duct is at the center of an enlarged, scarred portaltriad. Note the onionskin appearance of the concentric rings ofconnective tissue. The inflammation and scar tissue extend intothe periportal parenchyma. Panel D shows another type of stage2 lesion, an enlarged portal triad with proliferating bile-duct tis-sue and neutrophils. These lesions are not specific to primary
sclerosing cholangitis and may be seen in many types of chroniccholestasis. Panel E shows a normal portal tract, which containsa branch of the portal vein, an interlobular bile duct, and small
arterioles. (Masson trichrome, �190.)
accurate histologic staging requires the examinationof a sufficiently large specimen.
The cause of primary sclerosing cholangitis is un-
known. However, a number of factors have been pro-posed that might cause recurring damage to the bileducts and lead to development of the disease. These in-clude chronic portal bacteremia, toxic bile acid metab-olites produced by enteric flora, toxins produced direct-ly by enteric bacteria, chronic viral infections, ischemic
vascular damage, and genetic abnormalities of immu-noregulation.
The close association between primary sclerosing
cholangitis and ulcerative colitis led researchers tothe hypothesis that chronic portal bacteremia mightcause chronic biliary tract infection, inflammation,portal fibrosis, and ultimately, primary sclerosing cho-langitis.34-36 One study reported portal bacteremia insome patients with ulcerative colitis who had had co-lonic surgery.35 However, further research did not con-firm the observation. In these later studies, patientswith primary sclerosing cholangitis did not have evi-dence of portal-vein phlebitis, a typical feature of por-tal bacteremia.37-39
Other researchers have suggested that primary scle-
rosing cholangitis is the result of toxic bile acid me-
The New England Journal of Medicine
Downloaded from nejm.org on April 22, 2013. For personal use only. No other uses without permission.
Copyright 1995 Massachusetts Medical Society. All rights reserved.
THE NEW ENGLAND JOURNAL OF MEDICINE
tabolites generated by the gut flora.40 Lithocholic
eases such as Graves' disease, systemic lupus erythema-
acid, formed from chenodeoxycholic acid by bacterial
tosus, and myasthenia gravis.62 HLA-DRw52a is found
7-a-dehydroxylation in the colon, is hepatotoxic in ani-
in a high proportion of patients with primary sclerosing
mals.41 However, no major abnormalities in the compo-
cholangitis, but not in all, as was initially reported.63,64
sition and concentration of bile acids have been found
In patients with HLA-DR4, the course of primary scle-
in the bile and portal blood of patients with either pri-
rosing cholangitis tends to be accelerated.61
mary sclerosing cholangitis or chronic inflammatory
Patients with primary sclerosing cholangitis have
bowel disease.42 Moreover, lithocholic acid is rapidly
signs of abnormal immunoregulation, including infiltra-
sulfated and rendered nontoxic in human tissue. This
tion and destruction of bile ducts by lymphocytes,38 hy-
metabolic process has not been found to occur in ani-
pergammaglobulinemia with a disproportionate increase
mals, in which lithocholic acid can induce liver dis-
in serum IgM,65 perinuclear antineutrophil cytoplasmic
antibodies,66 anticolon epithelial autoantibodies,67 cir-
Research on animals suggests a third possible cause
culating immune complexes,68 increased metabolism of
of primary sclerosing cholangitis: bacterial products
complement component C3,69 and activation of the com-
acting as toxic proinflammatory agents. N-formyl
plement system by the classic pathway.70 Primary scle-
L-methionine L-leucine L-tyrosine is a peptide produced
rosing cholangitis is associated with other disorders of
by enteric flora. When this peptide, labeled with io-
immunoregulation, including inflammatory bowel dis-
dine-125, was introduced into the colons of rats with
ease,21 thyroiditis, and type I diabetes.62
experimentally induced colitis, it was absorbed, under-
The cellular immune system appears to play a part
went enterohepatic circulation, and appeared unde-
in primary sclerosing cholangitis. The total number of
graded in bile.46 Histologic changes in the livers of the
circulating T cells is decreased, whereas T cells are in-
rats resembled those in primary sclerosing cholangitis,
creased in the portal tracts.71-73 The ratio of CD4 to
including periportal inflammation with neutrophils
CD8 lymphocytes in the circulation is increased, as are
and eosinophils clustered around bile ducts. The injec-
the number and percentage of B cells.71 There is inhi-
tion of killed, nonpathogenic Escherichia coli into the
bition of leukocyte migration in the presence of biliary
portal veins of rabbits produced portal-vein fibrosis.47
antigens74 and enhanced autoreactivity of portal T lym-
Similar hepatic lesions developed in rats with experi-
phocytes.75 Finally, the aberrant expression of class II
mentally created blind loops in the jejunum after poly-
antigens on bile-duct epithelial cells suggests that bile-
mers prepared from the cell walls of intestinal bacteria
duct epithelial cells act as autoantigens to host lym-
were injected into the animals' portal veins.48
phocytes.76,77 It is unknown whether these immunologic
The natural history of primary sclerosing cholangi-
abnormalities are primary events or are due to the un-
tis, however, argues against a major pathogenetic role
derlying disease, although the ligation of bile ducts in
for portal bacteremia or bacterial metabolites. Antibi-
rats causes an aberrant expression of class II antigens
otic treatment, for example, is not effective against the
on bile-duct cells.78
disease.49 There is also no correlation between the se-verity of ulcerative colitis and that of primary scleros-
ing cholangitis.21 Primary sclerosing cholangitis may
The current criteria used to diagnose primary scle-
develop years before the onset of colitis or years after
rosing cholangitis are based on characteristic changes
patients have had total colectomies.50
in the intrahepatic and extrahepatic biliary tree seen
Chronic viral infections and ischemic damage to bile
with endoscopic retrograde cholangiopancreatography
ducts have also been implicated as causative factors in
or transhepatic cholangiography. Before the diagnosis
primary sclerosing cholangitis.51,52 Cholangitis caused
of primary sclerosing cholangitis is established, disor-
by cytomegalovirus in patients with acquired immu-
ders that cause secondary sclerosing cholangitis must
nodeficiency has a cholangiographic similarity to pri-
be ruled out. These include chronic bacterial cholangi-
mary sclerosing cholangitis.53 However, there are no
tis in patients with bile-duct stricture or choledocholithi-
data that suggest any relation in immunocompetent pa-
asis, ischemic bile-duct damage due to treatment with
tients.54,55 Likewise, no pathological data suggest that
floxuridine,52 infectious cholangiopathy associated with
ischemic damage to bile ducts is a cause of primary
the acquired immunodeficiency syndrome,53 previous
sclerosing cholangitis. Ischemia had been proposed
biliary surgery, congenital biliary-tree abnormalities,
because intraarterial injections of the chemotherapeu-
and bile-duct neoplasms. The presence of these disor-
tic agent floxuridine resulted in a clinical syndrome
ders is typically ruled out by the use of patient histo-
similar to that seen in primary sclerosing cholangitis.52
ries, blood-test results, characteristic cholangiographic
Intraarterial floxuridine has been shown to cause nar-
or ultrasound findings, or pathological findings from
rowing and obliteration of the arteries supplying the
bile-duct scraping and biopsies.
Laboratory tests in patients with primary sclerosing
Genetic and immunologic factors appear to play a
cholangitis usually show a cholestatic pattern, but bio-
part in primary sclerosing cholangitis, although the dis-
chemical abnormalities alone are never diagnostic.
order is not inherited in any distinct pattern. There are
The serum alkaline phosphatase level is usually ele-
familial occurrences of this uncommon disease,56,57
vated, although there are reports of patients in whom
as well as an association between primary sclerosing
the disease has been diagnosed by cholangiography
cholangitis and HLA-B8, DR3, DR2, and DR4.58-61
who have normal levels.79 Most patients have slight
HLA-B8 and DR3 are associated with autoimmune dis-
increases in serum aminotransferase levels, but the
The New England Journal of Medicine
Downloaded from nejm.org on April 22, 2013. For personal use only. No other uses without permission.
Copyright 1995 Massachusetts Medical Society. All rights reserved.
level of serum albumin is normal early in the disease.
Patients with active inflammatory bowel disease, how-ever, have decreased serum levels of albumin, reflect-ing the severity of that illness. In early stages of pri-mary sclerosing cholangitis, serum bilirubin valuesare usually normal, but they gradually increase as thedisease progresses. Occasionally, striking fluctuationsin bilirubin levels may occur even at early stages. Thecause is unknown, but the changes may reflect tran-sient blockage of strictured bile ducts by inflamma-tion, infection, sludge, or small gallstones. Hypergam-maglobulinemia is found in about 30 percent ofpatients, and increased IgM levels in 40 to 50 per-cent.26 Autoantibodies are less frequent than in auto-immune chronic active hepatitis and primary biliarycirrhosis. About 65 percent of patients with primarysclerosing cholangitis have perinuclear antineutrophilcytoplasmic antibodies80 and HLA-DRw52a.64 Anti–smooth-muscle antibodies are present in 11 percent ofpatients and antinuclear antibodies in 6 to 35 percent,but antimitochondrial antibodies are almost never ob-served.26 As in other chronic cholestatic liver diseases,levels of hepatic and urinary copper are increased, asis the serum ceruloplasmin level. Because copper isexcreted primarily in bile, the amount of copper in thebody increases as cholestasis worsens.
Visualization of the biliary tract is essential for mak-
ing the diagnosis of primary sclerosing cholangitis. En-doscopic retrograde cholangiopancreatography is themethod of choice. Percutaneous cholangiography istechnically more difficult in patients with the diseasebecause intrahepatic bile ducts are often attenuated orreduced in number. Transhepatic cholangiography is
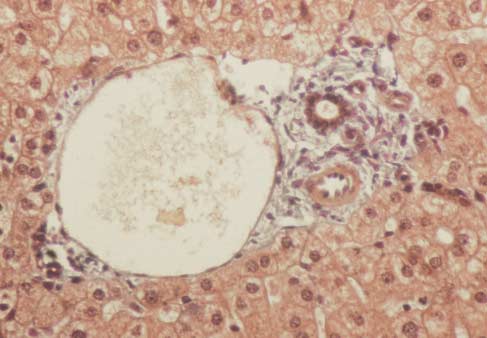
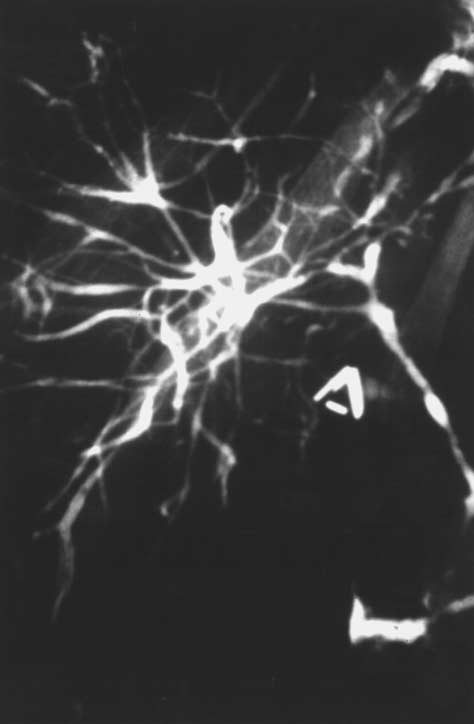
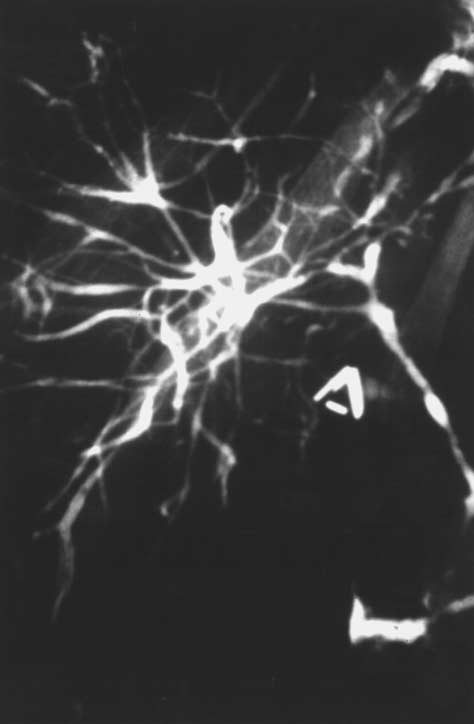
Figure 2. Endoscopic Retrograde Cholangiogram of a 62-Year-
performed only if endoscopic retrograde cholangiopan-
Old Woman with Primary Sclerosing Cholangitis.
creatography is unsuccessful. The characteristic radio-
There are multiple narrowings and dilatations of intra- and extra-
logic findings of primary sclerosing cholangitis include
hepatic bile ducts.
multifocal strictures and dilatations, usually involvingboth the intrahepatic and extrahepatic biliary tree(Fig. 2). Diffuse strictures with short intervening seg-
atograms are normal.83 This disease is probably the
ments of normal or dilated bile duct produce the classic
same as the condition called pericholangitis in ulcer-
beaded appearance. In early stages, the only cholangi-
ative colitis.84,85
ographic abnormality may be fine ulcerations of the
Although percutaneous liver biopsy may support the
common bile duct similar to those seen in the colon in
diagnosis of primary sclerosing cholangitis, it is rarely
early ulcerative colitis (Fig. 3). In other patients, there
definitive. Rather, it is useful in staging and in deter-
may be deep ulcerations in the common duct (Fig. 4).
mining the prognosis. Neither histologic examination
In our experience with more than 100 patients with pri-
nor cholangiography alone will reliably reflect the se-
mary sclerosing cholangitis, 87 percent had involve-
verity of the disease. Both must be used with blood
ment of both intrahepatic and extrahepatic bile ducts,
tests and with imaging or endoscopic tests that show
11 percent had involvement of the intrahepatic bile
the presence and severity of portal hypertension.
ducts alone, and 2 percent had involvement of only theextrahepatic bile ducts (unpublished data). The gall-
bladder and cystic duct are involved in as many as 15
The majority of patients are initially asymptomatic,
percent of patients.81,82
but can typically be identified on the basis of abnormal
There is one putative variant, called small-duct pri-
results on biochemical tests of liver function, particu-
mary sclerosing cholangitis, in which the affected bile
larly elevated levels of serum alkaline phosphatase or
ducts are too small to be seen by cholangiography.
g-glutamyltransferase. These abnormalities persist, and
Hence, cholangiograms appear normal. The preva-
eventually cholangiography, liver biopsy, or both, are
lence of small-duct primary sclerosing cholangitis is
performed. Liver-biopsy findings are usually either non-
unknown. It is diagnosed in patients with inflammatory
specific or suggestive of primary sclerosing cholangitis;
bowel disease who have biochemical tests of liver func-
the cholangiogram shows the characteristic changes.
tion that show cholestasis and characteristic liver biop-
Although asymptomatic, some patients may have sur-
sies, but whose endoscopic retrograde cholangiopancre-
prisingly advanced disease, as measured both histolog-
The New England Journal of Medicine
Downloaded from nejm.org on April 22, 2013. For personal use only. No other uses without permission.
Copyright 1995 Massachusetts Medical Society. All rights reserved.

THE NEW ENGLAND JOURNAL OF MEDICINE
those who were asymptomatic, and the survival ofasymptomatic patients was significantly shorter thanthat of a matched control population. Other studieshave reported similar findings, with median survival of9 to 12 years from diagnosis.87-90 There is no relationbetween the course of primary sclerosing cholangitisand that of accompanying inflammatory bowel disease.
Primary sclerosing cholangitis often occurs and wor-sens in patients whose inflammatory bowel disease hasbecome quiescent after colectomy.
Multivariate analysis has been used to identify prog-
nostic variables and to develop models that predict theprogression of primary sclerosing cholangitis. In a re-cent study of patients at five referral centers, the vari-ables that adversely affected survival were age, serumbilirubin and hemoglobin levels, hepatic histologicstage, and the presence of splenomegaly.91 According tothe study's model, the probability of surviving fiveyears from the time of diagnosis was 78 percent. In an-other study, prognostic variables included hepatomeg-aly, splenomegaly, serum alkaline phosphatase level,
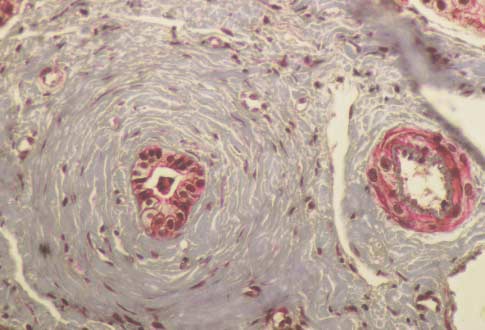
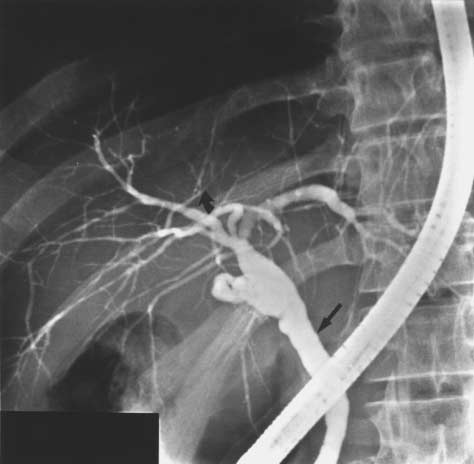
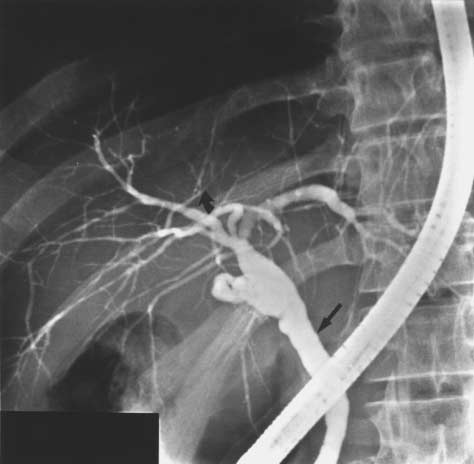
Figure 3. Endoscopic Retrograde Cholangiogram of a 28-Year-
histologic stage, and age.90 Although these models are
Old Man with Ulcerative Colitis and Early Primary Sclerosing
useful in classifying participants in therapeutic trials,
they may have limited application to the timing of liver
The patient presented with intense pruritus and a fivefold in-
transplantation in individual patients because of the
crease in the serum alkaline phosphatase level. There are fineulcerations (straight arrow) of the common bile duct and subtle
great variability of the disease.
narrowings (curved arrow) and dilatations of the intrahepatic
It is important to recognize a major difference be-
ically and radiologically. Some patients may remain
tween cholestatic liver diseases, such as primary scle-
asymptomatic for many years. Eventually, the serum
rosing cholangitis, in which bile ducts are the targets of
bilirubin level begins to increase or the serum albumin
the inflammatory and destructive processes, and chron-
level decreases (or both). When symptoms of itching,fatigue, jaundice, and weight loss develop, the patientsusually have advanced disease.
In 10 to 15 percent of patients, fever, night sweats,
chills, pain in the right upper quadrant, itching, orjaundice is present at the time of diagnosis.86 Despitethese symptoms, blood-test results, histologic featuresof the liver, and cholangiographic findings are similarto those in asymptomatic patients. The episodes of fe-ver and chills are often accompanied by transient wor-sening of the results of biochemical tests of liver func-tion; these episodes are indistinguishable from thoseproduced by acute bacterial cholangitis. They may lastfrom hours to days, but usually end without specifictreatment. Antibiotics are rarely helpful, and blood cul-tures rarely positive. It is not known whether these ep-isodes are caused by bacterial infections in areas nearstrictured and transiently occluded bile ducts or wheth-er they are simply part of the underlying inflammatoryprocess.
Although the majority of patients with primary scle-
rosing cholangitis are asymptomatic at the time of di-
Figure 4. Endoscopic Retrograde Cholangiogram of a 44-Year-
agnosis, most eventually have symptoms of fatigue,
Old Man with Primary Sclerosing Cholangitis and Crohn's
itching, and jaundice. Cirrhosis, portal hypertension,
and liver failure follow. In one study, the mean age of
There are deep ulcerations (solid arrow) in the common hepatic
patients at diagnosis was 39.9 years; the median length
duct and left intrahepatic bile duct, similar to those seen in thecolon in patients with colitis. There are filling defects (open ar-
of survival was 11.9 years from diagnosis.12 Patients
row) consistent with intraductal stones. The partially filled gall-
who were symptomatic at diagnosis lived less long than
bladder is visible on the left, and the endoscope is in place.
The New England Journal of Medicine
Downloaded from nejm.org on April 22, 2013. For personal use only. No other uses without permission.
Copyright 1995 Massachusetts Medical Society. All rights reserved.
ic hepatocellular diseases, such as hepatitis, in which
tients. Cholestyramine is effective for patients who have
hepatocytes are the targets. When bile ducts are de-
adequate bile flow.93 The dose is 4 to 8 g taken two
stroyed, they do not regenerate or they do so ineffec-
or three times daily. It usually takes two to four days
tively.86 An example of this is the vanishing-bile-duct
for cholestyramine to relieve itching. The drug is not
syndrome associated with rejection in orthotopic liver
helpful if bile flow has already been greatly decreased.
transplantation.92 In contrast, hepatocytes have an
Colestipol hydrochloride, another ammonium resin,
enormous capacity to regenerate. If patients with fulmi-
may be an alternative for those who cannot tolerate cho-
nant hepatitis survive, they recover fully and regain
lestyramine. Other therapies that have been used in
normal liver function. Likewise, patients with autoim-
patients unresponsive to cholestyramine include nal-
mune hepatitis who are deeply jaundiced and have
oxone,95 methyltestosterone,96 phenobarbital,97 rifam-
striking hypoalbuminemia may respond dramatically to
pin,98 plasmapheresis,99 ondansetron,100 antihistamines,
glucocorticoids and regain normal liver function. How-
ursodiol,101 S-adenosylmethionine,102 and ultraviolet
ever, there appears to be only a finite number of bile
ducts, which do not regenerate adequately when de-
Steatorrhea and malabsorption of fat-soluble vita-
stroyed. Primary sclerosing cholangitis should therefore
mins may occur late in the course of primary scleros-
be treated early in its course, before the serum level of
ing cholangitis. Fat malabsorption in patients with
bilirubin becomes permanently elevated. A serum bili-
jaundice is usually related to decreased secretion of
rubin level persistently greater than 1.5 mg per deciliter
conjugated bile acids into the small intestine. Other
(26 mmol per liter) is a sign of a poor prognosis and
causes are pancreatic insufficiency104,105 and celiac dis-
may indicate irreversible, medically untreatable dis-
ease,106 both of which may be associated with primary
sclerosing cholangitis. Asymptomatic vitamin A defi-
The treatment of primary sclerosing cholangitis has
ciency was found in almost 50 percent of patients with
been limited by uncertainty about its cause. As yet, no
primary sclerosing cholangitis in one study.107 A clin-
medical therapy has been proved effective. The medi-
ically important vitamin K deficiency rarely occurs
cal response to the illness may be divided into the
unless the patient has chronic jaundice and takes cho-
management of symptoms and complications, and the
lestyramine regularly. Similarly, deficiencies of vita-
treatment of the underlying disease process. But for pa-
mins D and E are uncommon and infrequently asso-
tients with end-stage disease who have symptomatic
ciated with clinical symptoms.108 However, there have
portal hypertension, liver failure, and recurrent or in-
been reports of metabolic bone disease and compres-
tractable bacterial cholangitis, liver transplantation is
sion fractures of the spine.109 As in primary biliary cir-
the only effective treatment.
rhosis, the bone disease is due to osteoporosis ratherthan osteomalacia. Fat-soluble vitamin levels should
Management of Chronic Cholestasis and Its Complications
be monitored and deficiencies treated with supple-
Many of the symptoms of primary sclerosing cholan-
gitis are similar to those of other cholestatic diseases,
Antibiotics have no role in slowing the progression of
such as primary biliary cirrhosis. However, unique
primary sclerosing cholangitis but have been used to
problems result from the mechanical bile-duct obstruc-
treat recurrent episodes of cholangitis. Bacterial cho-
tion characteristic of the disease, including bacterial
langitis is typically associated with biliary surgery, bile-
cholangitis, sepsis, and the formation of pigment stones
duct stones, or obstructing strictures. Tetracycline was
within the obstructed bile ducts. In addition, patients
determined to be ineffective in one small study of pa-
with primary sclerosing cholangitis are at risk for bile-
tients with primary sclerosing cholangitis,49 but prophy-
duct cancers. These cancers may be very difficult to dis-
lactic antibiotics, usually amoxicillin, ciprofloxacin, or
tinguish from the tight bile-duct strictures typically
trimethoprim–sulfamethoxazole, are often used for re-
seen in primary sclerosing cholangitis.
current episodes of cholangitis. Anecdotal reports sug-
Symptoms of primary sclerosing cholangitis include
gest that such drugs reduce the frequency and severity
fatigue, pruritus, and steatorrhea. One of the more
of bacterial cholangitis. Additional controlled trials are
bothersome symptoms is pruritus. Itching is worse at
needed to test this hypothesis.
bedtime and in warm weather and may be exacerbated
Dominant strictures of the extrahepatic bile ducts,
by eating rich, fatty meals. It can be severely debilitat-
which cause or exacerbate symptoms, occur in 15 to 20
ing, interfere with sleep, and provoke extensive excori-
percent of patients with primary sclerosing cholangi-
ations. The cause of the pruritus is unknown. The re-
tis.110 Endoscopic balloon dilation of strictures, with or
tention of bile acids and their sequestration in skin are
without the placement of stents, has relieved symp-
not the cause. Nevertheless, bile acid–binding resins
toms of jaundice, pruritus, and fever, and has reduced
are an effective treatment, presumably because they
serum levels of alkaline phosphatase and aminotrans-
bind to the true pruritogenic agent excreted in bile.93
ferases in selected patients.110 In several retrospective
More recently, the accumulation of endogenous opiates
studies, patients appeared to have fewer episodes of
has been proposed as a cause of the pruritus. Opiate
cholangitis if they were treated endoscopically with
antagonists may decrease pruritus, and there are in-
papillotomy of Oddi's sphincter, nasobiliary catheter
creased serum concentrations of endorphin-like sub-
irrigation of the common bile duct with glucocorti-
stances in patients with other chronic cholestastic liver
coids, or dilation of strictures with either balloons or
diseases, such as primary biliary cirrhosis.94
stents.111-113 Results of biochemical tests and cholangi-
The pruritus can be effectively treated in most pa-
ographic findings improved in some patients so treat-
The New England Journal of Medicine
Downloaded from nejm.org on April 22, 2013. For personal use only. No other uses without permission.
Copyright 1995 Massachusetts Medical Society. All rights reserved.
THE NEW ENGLAND JOURNAL OF MEDICINE
ed. There are no controlled trials evaluating endoscop-
progression of disease.124 Finally, corticosteroids may
ic therapy, but there appears to be little risk and some
hasten the onset and progression of osteoporosis and in-
potential benefit from this approach.
crease spontaneous bone fractures. There is, however,
Another method of managing dominant strictures,
one favorable report. In an uncontrolled trial of cortico-
surgical dilation, or choledochojejunostomy, is now rare-
steroid use, 10 patients with prefibrotic primary scleros-
ly used. Surgery carries the risk of postoperative infec-
ing cholangitis had improvements in the results of both
tion and increases scarring in the porta hepatis, poten-
blood tests and histologic examination of the liver. Four
tially complicating future liver transplantation.114 The
of these patients remain well after 11 years and are still
development of stomal varices is a complication unique
receiving low-dose prednisone (LaBrecque DR: person-
to patients with advanced primary sclerosing cholangi-
al communication).
tis who have undergone colectomy and ileostomy.115Treatment of bleeding from the stomal varices is diffi-
cult and usually requires either a central portosystemic
Penicillamine has been evaluated in a double-blind
shunt or liver transplantation.
prospective trial of patients followed for 36 months.125
There is an increased incidence of cholangiocarci-
The drug produced the expected urinary excretion of
noma in patients with primary sclerosing cholangitis,
copper, but had no beneficial effect on symptoms, bio-
about 9 to 15 percent.116,117 Patients with long-standing
chemical test results, liver histology, disease progres-
ulcerative colitis and cirrhosis are at highest risk.118,119
sion, or survival. In addition, 21 percent of the patients
The early diagnosis of bile-duct carcinoma is ham-
had major side effects from penicillamine. The toxicity
pered by the lack of sensitive, specific serologic markers
and the lack of efficacy have discouraged further use of
as well as the insensitivity of biliary cytology. Often an
unsuspected cholangiocarcinoma is found after livertransplantation, when the resected liver is examined in
the pathology laboratory.120 Unfortunately, there is no
Ursodiol has been associated with a clear improve-
reliable way to distinguish a dominant stricture from a
ment in the results of biochemical tests of liver function
cholangiocarcinoma, even after repeated imaging, en-
in primary sclerosing cholangitis. Therapy with the
doscopic biopsies, and cytologic examination. Most ex-
drug leads to a two-to-threefold increase in the serum
perts suggest that patients with a high likelihood of
bile acid concentration. There is an increase in the bil-
cholangiocarcinoma should be referred for liver trans-
iary and urinary excretion of bile acids and an increase
plantation and should undergo pretransplantation lap-
in bile flow. In vitro, ursodiol stabilizes liver-cell mem-
arotomy in order to rule out the extrahepatic spread of
branes exposed to toxic concentrations of the naturally
cancer.116,120,121 Unfortunately, treatment of cholangio-
occurring bile acid chenodeoxycholic acid.126 Several
carcinoma by resection, chemotherapy, and radiation
open-label trials of ursodiol have reported improve-
has had discouraging results, as has liver transplanta-
ments in symptoms and in the results of liver-function
tion for clinically apparent tumors.120
tests.27,28,127,128 There is no information on the cholangi-ographic appearance of the biliary tree. In a prospec-
Medical Therapy for Primary Sclerosing Cholangitis
tive, randomized, double-blind, placebo-controlled tri-
A variety of immunosuppressive, antiinflammatory,
al, there was improvement in the results of biochemical
and antifibrotic agents have been used to treat primary
tests of liver function and liver histology in those pa-
sclerosing cholangitis. However, no drug has been
tients receiving ursodiol.29 However, there was no dif-
shown to improve the natural history of the disease.
ference in patient survival or in referral for liver trans-
The evaluation of treatment has been limited by the in-
plantation. There are no data on the long-term efficacy
dolent course of primary sclerosing cholangitis in most
of ursodiol.
patients and the spontaneous exacerbations and remis-sions in others. Hence, it takes years before any treat-
ment can be shown to alter the natural history. Of the
On the basis of clinical and histologic improvements
various drugs used to treat primary sclerosing cholan-
in 2 patients with primary sclerosing cholangitis, we
gitis, only a few have been evaluated in randomized,
conducted an open-label trial of oral methotrexate in
controlled trials.
21 patients with the disease, 7 of whom had cirrhosis aswell30,129,130 (and unpublished data). No patients with
cirrhosis had improvement in their condition. In patients
Despite anecdotal reports of improvement in patients
without advanced disease, there was improvement in
with primary sclerosing cholangitis who took cortico-
symptoms and in the results of biochemical tests of liv-
steroids,122,123 there is little enthusiasm for their use for
er function. Follow-up liver biopsies revealed histologic
several reasons. Approximately 75 percent of patients
improvement, primarily decreased inflammation. Most
with primary sclerosing cholangitis have chronic inflam-
patients in this group had less stricturing on cholangi-
matory bowel disease and are already being treated
ography after one to eight years of methotrexate. How-
with corticosteroids while primary sclerosing cholangi-
ever, in a recently concluded prospective, double-blind
tis develops and progresses. Furthermore, combined
study, methotrexate produced no therapeutic benefit.31
treatment with both corticosteroids and colchicine nei-
Although methotrexate, as compared with placebo, sig-
ther improved biochemical test results nor slowed the
nificantly reduced the serum levels of alkaline phos-
The New England Journal of Medicine
Downloaded from nejm.org on April 22, 2013. For personal use only. No other uses without permission.
Copyright 1995 Massachusetts Medical Society. All rights reserved.
phatase, it had no effect on serum levels of bilirubin,
after transplantation, it is important to continue mon-
aminotransferases, or albumin, or on the rate of refer-
itoring for colon cancer in patients with primary scle-
ral for liver transplantation. Half the patients in this
rosing cholangitis who also have chronic ulcerative
study already had cirrhosis and may have had medical-
ly irreversible disease. A larger randomized, controlledtrial including only patients without cirrhosis is needed
to evaluate methotrexate further.
Primary sclerosing cholangitis remains an enigmatic,
difficult-to-treat disease. Progress in treating or pre-
Other Medical Agents
venting this disease will be slow until its cause is better
There have been anecdotal reports of the treatment
understood. The indolent beginnings of the illness for
of primary sclerosing cholangitis with azathioprine, col-
most patients and its slow rate of progression belie its
chicine, cholestyramine, antibiotics, and cyclosporine,
true severity. Often, physicians delay treatment, or the
but no convincing evidence that any of these agents is
referral of patients to centers conducting controlled tri-
effective.131-135
als, until the disease has become symptomatic andhence untreatable. Most symptomatic patients have ad-
vanced and medically irreversible disease. In the fu-
The close association between primary sclerosing
ture, asymptomatic patients with only early cholangio-
cholangitis and ulcerative colitis, along with the hypo-
graphic and histologic changes should be included in
thetical role of enteric bacteria in the disease's patho-
prospective trials of new therapies. New strategies that
genesis, has led some to consider proctocolectomy as a
employ combinations of drugs such as ursodiol, metho-
treatment. But in one retrospective study of patients
trexate, antibiotics, and other immunomodulatory com-
with both primary sclerosing cholangitis and chronic
pounds appear to be the most promising approach to
ulcerative colitis, patients who underwent proctocolec-
treatment at this time.
tomy had no improvement in biochemical test results,cholangiography, hepatic histology, or survival.50 Proc-
tocolectomy should be performed only because of the
1. Chapman RWG, Arborgh BA, Rhodes JM, et al. Primary sclerosing cho-
severity of proctocolitis.
langitis: a review of its clinical features, cholangiography, and hepatic his-tology. Gut 1980;21:870-7.
2. Lefkowitch JH. Primary sclerosing cholangitis. Arch Intern Med 1982;142:
Liver transplantation is now the treatment of choice
3. LaRusso NF, Wiesner RH, Ludwig J, MacCarty RL. Primary sclerosing
cholangitis. N Engl J Med 1984;310:899-903.
for patients with advanced liver disease. Indications for
4. Lindor KD, Wiesner RH, LaRusso NF. Recent advances in the manage-
liver transplantation include hemorrhage due to esoph-
ment of primary sclerosing cholangitis. Semin Liver Dis 1987;7:322-7.
ageal varices or portal gastropathy, intractable ascites
5. MacCarty RI, LaRusso NF, Wiesner RH, Ludwig J. Primary sclerosing
cholangitis: findings on cholangiography and pancreatography. Radiology
(with or without spontaneous bacterial peritonitis), re-
current episodes of bacterial cholangitis, progressive
6. Chen LY, Goldberg HI. Sclerosing cholangitis: broad spectrum of radio-
muscle wasting, and hepatic encephalopathy. Most of
graphic features. Gastrointest Radiol 1984;9:39-47.
7. Galambos JT. Epidemiology of alcoholic liver disease: United States of
the patients with these conditions are jaundiced. How-
America. In: Hall P, ed. Alcoholic liver disease: pathobiology, epidemiolo-
ever, jaundice alone, in the absence of other signs of
gy and clinical aspects. New York: John Wiley, 1985:230-49.
8. Garagliano CF, Lilienfeld AM, Mendeloff AI. Incidence rates of liver cir-
liver failure, is not an absolute indication for trans-
rhosis and related diseases in Baltimore and selected areas of the United
plantation. Three-year survival after liver transplanta-
States. J Chronic Dis 1979;32:543-54.
tion is 85 percent at most centers.136,137 A post-trans-
9. United Network for Organ Sharing update. 1993;9:27-9.
10. Wiesner RH, Grambsch P, LaRusso NF, Dickson ER. Is primary sclerosing
plantation problem, more common in patients with
cholangitis a progressive disease or not? Hepatology 1988;8:970-2.
primary sclerosing cholangitis than in other groups, is
11. Porayko MK, Wiesner RH, LaRusso NF, et al. Patients with asymptomatic
the development of strictures in the transplanted bile
primary sclerosing cholangitis frequently have progressive disease. Gastro-enterology 1990;98:1594-602.
ducts. The pattern is similar to that seen in the natural
12. Wiesner RH, Grambsch PM, Dickson ER, et al. Primary sclerosing cholan-
course of the disease.138,139 Possible causes of the stric-
gitis: natural history, prognostic factors and survival analysis. Hepatology1989;10:430-6.
tures include the recurrence of primary sclerosing cho-
13. Bartholomew LG, Cain JC, Woolner LB, Utz DC, Ferris DO. Sclerosing
langitis, ischemia, chronic rejection, and infectious
cholangitis: its possible association with Riedel's struma and fibrous retro-
cholangitis related to the Roux-en-Y biliary anasto-
peritonitis — report of two cases. N Engl J Med 1963;269:8-12.
14. Sivak MV Jr, Farmer RG, Lalli AF. Sclerosing cholangitis: its increasing
mosis and immunosuppression. Current data point to
frequency of recognition and association with inflammatory bowel disease.
infection as the cause. Creation of longer jejunal loops
J Clin Gastroenterol 1981;3:261-6.
in the Roux-en-Y anastomosis and treatment with ap-
15. Lebovics E, Palmer M, Woo J, Shaffner F. Outcome of primary sclerosing
cholangitis: analysis of long-term observation of 38 patients. Arch Intern
propriate antibiotics are usually effective in prevent-
ing or treating this complication. In patients with pri-
16. Helzberg JH, Petersen JM, Boyer JL. Improved survival with primary scle-
rosing cholangitis: a review of clinicopathologic features and comparison
mary sclerosing cholangitis and inflammatory bowel
of symptomatic and asymptomatic patients. Gastroenterology 1987;92:
disease who undergo liver transplantation, the symp-
toms of their bowel disease generally improve after
17. Lindor KD, Wiesner RH, MacCarty RL, Ludwig J, LaRusso NF. Advances
in primary sclerosing cholangitis. Am J Med 1990;89:73-80.
transplantation.140 On the other hand, there are re-
18. Rabinovitz M, Gavaler JS, Schade RR, Dindzans VJ, Chien M-C, Van Thiel
ports of colon cancer developing after liver transplan-
DH. Does primary sclerosing cholangitis occurring in association with in-
tation in two patients who had both primary sclerosing
flammatory bowel disease differ from that occurring in the absence of in-flammatory bowel disease? A study of sixty-six subjects. Hepatology 1990;
cholangitis and chronic ulcerative colitis.141 Thus, even
The New England Journal of Medicine
Downloaded from nejm.org on April 22, 2013. For personal use only. No other uses without permission.
Copyright 1995 Massachusetts Medical Society. All rights reserved.
THE NEW ENGLAND JOURNAL OF MEDICINE
19. Stockbrugger RW, Olsson R, Jaup B, Jensen J. Forty-six patients with pri-
51. Finegold MJ, Carpenter RJ. Obliterative cholangitis due to cytomegalovi-
mary sclerosing cholangitis: radiological bile duct changes in relationship
rus: a possible precursor of paucity of intrahepatic bile ducts. Hum Pathol
to clinical course and concomitant inflammatory bowel disease. Hepatogas-
52. Ludwig J, Kim CH, Wiesner RH, Krom RAF. Floxuridine-induced scleros-
20. Aadland E, Schrumpf E, Fausa O, et al. Primary sclerosing cholangitis: a
ing cholangitis: an ischemic cholangiopathy? Hepatology 1989;9:215-8.
long-term follow-up study. Scand J Gastroenterol 1987;22:655-64.
53. Cello JP. Acquired immunodeficiency syndrome cholangiopathy: spectrum
21. Fausa O, Schrumpf E, Elgjo K. Relationship of inflammatory bowel disease
of disease. Am J Med 1989;86:539-46.
and primary sclerosing cholangitis. Semin Liver Dis 1991;11:31-9.
54. Mehal WZ, Hattersley AT, Chapman RW, Fleming KA. A survey of cyto-
22. Shepherd HA, Selby WS, Chapman RWG, et al. Ulcerative colitis and per-
megalovirus (CMV) DNA in primary sclerosing cholangitis (PSC) liver
sistent liver dysfunction. Q J Med 1983;52:503-13.
tissues using a sensitive polymerase chain reaction (PCR) based assay.
23. Schrumpf E, Fausa O, Elgjo K, Kolmannskog F. Hepatobiliary complica-
J Hepatol 1992;15:396-9.
tions of inflammatory bowel disease. Semin Liver Dis 1988;8:201-9.
55. Hay JE, Rosser BG, Espy MJ, et al. Cytomegalovirus (CMV) and primary
24. Tobias R, Wright JP, Kottler RE, et al. Primary sclerosing cholangitis
sclerosing cholangitis (PSC): no evidence for pathogenic association. Gas-
associated with inflammatory bowel disease in Cape Town, 1975–1981.
troenterology 1993;104:Suppl:A913. abstract.
S Afr Med J 1983;63:229-35.
56. Quigley EMM, LaRusso NF, Ludwig J, MacSween RNM, Birnie GG, Wat-
25. Stonnington CM, Phillips SF, Melton LJ III, Zinsmeister AR. Chronic ul-
kinson G. Familial occurrence of primary sclerosing cholangitis and ulcer-
cerative colitis: incidence and prevalence in a community. Gut 1987;28:
ative colitis. Gastroenterology 1983;85:1160-5.
57. Jorge AD, Esley C, Ahumada J. Family incidence of primary sclerosing
26. Wiesner RH, Porayko MK, LaRusso NF, Ludwig J. Primary sclerosing
cholangitis associated with immunologic diseases. Endoscopy 1987;19:
cholangitis. In: Schiff L, Schiff ER, eds. Diseases of the liver. 7th ed. Vol.
1. Philadelphia: J.B. Lippincott, 1993:411-26.
58. Chapman RW, Varghese Z, Gaul R, Patel G, Kokinon N, Sherlock S. As-
27. Chazouilleres O, Poupon R, Capron JP, et al. Ursodeoxycholic acid for pri-
sociation of primary sclerosing cholangitis with HLA-B8. Gut 1983;24:38-
mary sclerosing cholangitis. J Hepatol 1990;11:120-3.
28. O'Brien CB, Senior JR, Arora-Mirchandani R, Batta AK, Salen G. Urso-
59. Schrumpf E, Fausa O, Forre O, Dobloug JH, Ritland S, Thorsby E. HLA
deoxycholic acid for the treatment of primary sclerosing cholangitis: a 30-
antigens and immunoregulatory T cells in ulcerative colitis associated with
month pilot study. Hepatology 1991;14:838-47.
hepatobiliary disease. Scand J Gastroenterol 1982;17:187-91.
29. Beuers U, Spengler U, Kruis W, et al. Ursodeoxycholic acid for treatment
60. Donaldson PT, Farrant JM, Wilkinson ML, Hayllar K, Portmann BC, Wil-
of primary sclerosing cholangitis: a placebo-controlled trial. Hepatology
liams R. Dual association of HLA DR2 and DR3 with primary sclerosing
cholangitis. Hepatology 1991;13:129-33.
30. Knox TA, Kaplan MM. Treatment of primary sclerosing cholangitis with
61. Mehal WZ, Lo YM, Wordsworth BP, et al. HLA DR4 is a marker for rapid
oral methotrexate. Am J Gastroenterol 1991;86:546-52.
disease progression in primary sclerosing cholangitis. Gastroenterology
31. Idem. A double-blind controlled trial of oral-pulse methotrexate therapy in
the treatment of primary sclerosing cholangitis. Gastroenterology 1994;
62. Eddleston AL, Williams R. HLA and liver disease. Br Med Bull 1978;34:
32. Ludwig J, LaRusso NF, Wiesner RH. Primary sclerosing cholangitis. In:
63. Prochazka EJ, Terasaki PI, Park MS, Goldstein LI, Busuttil RW. Associa-
Peters RL, Craig JR, eds. Contemporary issues in surgical pathology: liver
tion of primary sclerosing cholangitis with HLA-DRw52a. N Engl J Med
pathology. New York: Churchill Livingstone, 1986.
33. Klatskin G, Conn HO. Histopathology of the liver. Vol. 2. New York: Ox-
64. Sharma AN, Arora S, Rabson AR, Kaplan MM. HLA-DRw52a and pri-
ford University Press, 1993:99.
mary sclerosing cholangitis (PSC): linkage but less than 100%. Hepatology
34. Boden RW, Rankin JG, Goulston SJM, et al. The liver in ulcerative colitis:
the significance of raised serum-alkaline-phosphatase levels. Lancet 1959;
65. Chapman RW. Role of immune factors in the pathogenesis of primary scle-
rosing cholangitis. Semin Liver Dis 1991;11:1-4.
35. Brooke BN, Dykes PW, Walker FC. A study of liver disorder in ulcerative
66. Snook JA, Chapman RW, Fleming K, Jewell DP. Anti-neutrophil nuclear
colitis. Postgrad Med J 1961;37:245-51.
antibody in ulcerative colitis, Crohn's disease and primary sclerosing cho-
36. Warren KW, Athanassiades S, Monge JI. Primary sclerosing cholangitis: a
langitis. Clin Exp Immunol 1989;76:30-3.
study of forty-two cases. Am J Surg 1966;111:23-38.
67. Zauli D, Schrumpf E, Crespi C, Cassani F, Fausa O, Aadland E. An auto-
37. Palmer KR, Duerden BI, Holdsworth CD. Bacteriological and endotoxin
antibody profile in primary sclerosing cholangitis. J Hepatol 1987;5:14-8.
studies in cases of ulcerative colitis submitted to surgery. Gut 1980;21:851-4.
68. Bodenheimer HC Jr, LaRusso NF, Thayer WR Jr, Charland C, Staples PJ,
38. Ludwig J, Barham SS, LaRusso NF, Elveback LR, Wiesner RH, McCall
Ludwig J. Elevated circulating immune complexes in primary sclerosing
JT. Morphologic features of chronic hepatitis associated with primary scle-
cholangitis. Hepatology 1983;3:150-4.
rosing cholangitis and chronic ulcerative colitis. Hepatology 1981;1:632-
69. Brinch L, Teisberg P, Schrumpf E, Akesson I. The in vivo metabolism of
C3 in hepatobiliary disease associated with ulcerative colitis. Scand J Gas-
39. Vinnik IE, Kern F Jr, Struthers JE Jr, Hill RB, Guzak S. Experimental
chronic portal vein bacteremia. Proc Soc Exp Biol Med 1964;115:311-4.
70. Senaldi G, Donaldson PT, Magrin S, et al. Activation of the complement sys-
40. Carey JB Jr. Bile acids, cirrhosis, and human evolution. Gastroenterology
tem in primary sclerosing cholangitis. Gastroenterology 1989;97:1430-4.
71. Lindor KD, Wiesner RH, Katzmann JA, LaRusso NF, Beaver SJ. Lympho-
41. Palmer RH. Bile acids, liver injury, and liver disease. Arch Intern Med
cyte subsets in primary sclerosing cholangitis. Dig Dis Sci 1987;32:720-5.
72. Snook JA, Chapman RW, Sachdev GK, et al. Peripheral blood and portal
42. Siegel JH, Barnes S, Morris JS. Bile acids in liver disease associated with
tract lymphocyte populations in primary sclerosing cholangitis. J Hepatol
inflammatory bowel disease. Digestion 1977;15:469-81.
43. Cowen AE, Korman MG, Hofmann AF, Cass OW. Metabolism of lithocho-
73. Whiteside TL, Lasky S, Si L, Van Thiel DH. Immunologic analysis of
late in healthy man. I. Biotransformation and biliary excretion of intrave-
mononuclear cells in liver tissues and blood of patients with primary scle-
nously administered lithocholate, lithocholylglycine, and their sulfates.
rosing cholangitis. Hepatology 1985;5:468-74.
74. McFarlane IG, Wojcicka BM, Tsantoulas DC, Portmann BC, Eddleston
44. Gadacz TR, Allan RN, Mack E, et al. Impaired lithocholate sulfation in the
ALWF, Williams R. Leukocyte migration inhibition in response to biliary
rhesus monkey: a possible mechanism for chenodeoxycholate toxicity.
antigens in primary biliary cirrhosis, sclerosing cholangitis, and other
chronic liver diseases. Gastroenterology 1979;76:1333-40.
45. Allan RN, Thistle JL, Hofmann AF. Lithocholate metabolism during
75. Lindor KD, Wiesner RH, LaRusso NF, Homburger HA. Enhanced autore-
chenotherapy for gallstone dissolution. II. Absorption and sulphation. Gut
activity of T-lymphocytes in primary sclerosing cholangitis. Hepatology
46. Hobson CH, Butt TJ, Ferry DM, Hunter J, Chadwick VS, Broom MF. En-
76. Chapman RW, Kelly PMA, Heryet A, Jewell DP, Fleming KA. Expression
terohepatic circulation of bacterial chemotactic peptide in rats with exper-
of HLA-DR antigens on bile duct epithelium in primary sclerosing cholan-
imental colitis. Gastroenterology 1988;94:1006-13.
gitis. Gut 1988;29:422-7.
47. Kono K, Ohnishi K, Omata M, et al. Experimental portal fibrosis produced
77. Broomé U, Glaumann H, Hultcrantz R, Forsum U. Distribution of HLA-
by intraportal injection of killed nonpathogenic Escherichia coli in rabbits.
DR, HLA-DP, HLA-DQ antigens in liver tissue from patients with primary
sclerosing cholangitis. Scand J Gastroenterol 1990;25:54-8.
48. Lichtman SN, Sartor RB, Keku J, Schwab JH. Hepatic inflammation in rats
78. Phillips JO, Alpini G, Pham L, Ueno Y, LaRusso NF. Cholestasis induces
with experimental small intestinal bacterial overgrowth. Gastroenterology
cell-specific gene and protein expression of MHC class II antigen in rat liv-
er. Gastroenterology 1993;104:Suppl:A972. abstract.
49. Mistilis SP, Skyring AP, Goulston SJ. Effect of long-term tetracycline ther-
79. Balasubramaniam K, Wiesner RH, LaRusso NF. Primary sclerosing cho-
apy, steroid therapy and colectomy in pericholangitis associated with ulcer-
langitis with normal serum alkaline phosphatase activity. Gastroenterology
ative colitis. Australas Ann Med 1965;14:286-94.
50. Cangemi JR, Wiesner RH, Beaver SJ, et al. Effect of proctocolectomy for
80. Duerr RH, Targan SR, Landers CJ, et al. Neutrophil cytoplasmic antibod-
chronic ulcerative colitis on the natural history of primary sclerosing cho-
ies: a link between primary sclerosing cholangitis and ulcerative colitis.
langitis. Gastroenterology 1989;96:790-4.
The New England Journal of Medicine
Downloaded from nejm.org on April 22, 2013. For personal use only. No other uses without permission.
Copyright 1995 Massachusetts Medical Society. All rights reserved.
81. Brandt DJ, MacCarty RL, Charboneau JW, LaRusso NF, Wiesner RH, Lud-
112. Huibregtse K. Endoscopic biliary and pancreatic drainage. Stuttgart, Ger-
wig J. Gallbladder disease in patients with primary sclerosing cholangitis.
many: Georg Thieme Verlag, 1988.
AJR Am J Roentgenol 1988;150:571-4.
113. Cotton PB, Nickl N. Endoscopic and radiologic approaches to therapy in
82. Jeffrey GP, Reed WD, Carrello S, Shilkin KB. Histological and immuno-
primary sclerosing cholangitis. Semin Liver Dis 1991;11:40-8.
histochemical study of the gall bladder lesion in primary sclerosing cho-
114. Cameron JL, Pitt HA, Zinner MJ, et al. Resection of hepatic duct bifurca-
langitis. Gut 1991;32:424-9.
tion and transhepatic stenting for sclerosing cholangitis. Ann Surg 1988;
83. Wee A, Ludwig J. Pericholangitis in chronic ulcerative colitis: primary
sclerosing cholangitis of the small bile ducts? Ann Intern Med 1985;102:
115. Wiesner RH, LaRusso NF, Dozois RR, Beaver SJ. Peristomal varices after
proctocolectomy in patients with primary sclerosing cholangitis. Gastroen-
84. Vinnik IE, Kern F Jr. Liver diseases in ulcerative colitis. Arch Intern Med
116. Rosen CB, Nagorney DM, Wiesner RH, Coffey RJ Jr, LaRusso NF. Cho-
85. Mistilis SP. Pericholangitis and ulcerative colitis. I. Pathology, etiology,
langiocarcinoma complicating primary sclerosing cholangitis. Ann Surg
and pathogenesis. Ann Intern Med 1965;63:1-16.
86. Kaplan MM. Medical approaches to primary sclerosing cholangitis. Semin
117. Fausa O, Schrumpf E. Cholangiocarcinoma occurs with high frequency in
Liver Dis 1991;11:56-63.
primary sclerosing cholangitis. Scand J Gastroenterol 1989;24:Suppl 159:
87. Herrmann R, Dooley JS, Sherlock S, McIntyre N. Natural history and mor-
59. abstract.
tality in primary sclerosing cholangitis. Gut 1988;29:A1430. abstract.
118. Ross AP, Braasch JW. Ulcerative colitis and carcinoma of the proximal bile
88. Taub W, Barnes D, Sivak M Jr. The natural history of primary sclerosing
ducts. Gut 1973;14:94-7.
cholangitis. Gastroenterology 1988;94:A598. abstract.
119. Ritchie JK, Allan RN, Macartney J, Thompson H, Hawley PR, Cooke WT.
89. Martin FM, Rossi RL, Nugent FW, et al. Surgical aspects of sclerosing cho-
Biliary tract carcinoma associated with ulcerative colitis. Q J Med 1974;
langitis: results in 178 patients. Ann Surg 1990;212:551-8.
90. Farrant JM, Hayllar KM, Wilkinson M, et al. Natural history and prognos-
120. Marsh JW Jr, Iwatsuki S, Makowka L, et al. Orthotopic liver transplanta-
tic variables in primary sclerosing cholangitis. Gastroenterology 1991;100:
tion for primary sclerosing cholangitis. Ann Surg 1988;207:21-5.
121. Stieber AC, Marino IR, Iwatsuki S, Starzl TE. Cholangiocarcinoma in scle-
91. Dickson ER, Murtaugh PA, Wiesner RH, et al. Primary sclerosing cholan-
rosing cholangitis: the role of liver transplantation. Int Surg 1989;74:1-3.
gitis: refinement and validation of survival models. Gastroenterology 1992;
122. Myers RN, Cooper JH, Padis N. Primary sclerosing cholangitis: complete
gross and histologic reversal after long-term steroid therapy. Am J Gastro-
92. Batts KP, Moore SB, Perkins JD, Wiesner RH, Grambsch PM, Krom RA.
Influence of positive lymphocyte crossmatch and HLA mismatching on
123. Burgert SL, Brown BP, Kirkpatrick RB, LaBrecque DR. Positive corticos-
vanishing bile duct syndrome in human liver allografts. Transplantation
teroid response in early primary sclerosing cholangitis. Gastroenterology
93. Datta DV, Sherlock S. Cholestyramine for long term relief of the pruritus
124. Lindor KD, LaRusso NF, Wiesner RH. Prednisone and colchicine are not
complicating intrahepatic cholestasis. Gastroenterology 1966;50:323-32.
of benefit after two years in patients with primary sclerosing cholangitis.
94. Thornton JR, Losowsky MS. Opioid peptides and primary biliary cirrhosis.
Hepatology 1989;10:638. abstract.
125. LaRusso NF, Wiesner RH, Ludwig J, MacCarty RL, Beaver SJ, Zinsmeis-
95. Bergasa NV, Talbot TL, Alling DW, et al. A controlled trial of naloxone
ter AR. Prospective trial of penicillamine in primary sclerosing cholangitis.
infusions for the pruritus of chronic cholestasis. Gastroenterology 1992;
126. Galle PR, Theilmann L, Raedsch R, Kommerell B, Stiehl A. Ursodeoxy-
96. Lloyd-Thomas H, Sherlock S. Testosterone therapy for the pruritus of ob-
cholate reduces hepatotoxicity of glycochenodeoxycholate in primary hu-
structive jaundice. BMJ 1952;2:1289-91.
man liver cells. Gastroenterology 1990;98:Suppl:A588. abstract.
97. Bloomer JR, Boyer JL. Phenobarbital effects in cholestatic liver diseases.
127. Podda M, Ghezzi C, Battezzati PM, et al. Effect of different doses of ur-
Ann Intern Med 1975;82:310-7.
sodeoxycholic acid in chronic liver disease. Dig Dis Sci 1989;34:Suppl:
98. Podesta A, Lopez P, Terg R, et al. Treatment of pruritus of primary biliary
cirrhosis with rifampin. Dig Dis Sci 1991;36:216-20.
128. Hayashi H, Higuchi T, Ichimiya H, Hishida N, Sakamoto N. Asymptomatic
99. Cohen LB, Ambinder EP, Wolke AM, Field SP, Schaffner F. Role of plas-
primary sclerosing cholangitis treated with ursodeoxycholic acid. Gastro-
mapheresis in primary biliary cirrhosis. Gut 1985;26:291-4.
100. Raderer M, Müller C, Scheithauer W. Ondansetron for pruritus due to
129. Kaplan MM, Arora S, Pincus SH. Primary sclerosing cholangitis and low-
cholestasis. N Engl J Med 1994;330:1540.
dose oral pulse methotrexate therapy. Ann Intern Med 1987;106:231-5.
101. Calmus Y, Gane P, Rouger P, Poupon R. Hepatic expression of class I and
130. Kaplan MM. Methotrexate treatment of chronic cholestatic liver diseases:
class II major histocompatibility complex molecules in primary biliary cir-
friend or foe? Q J Med 1989;72:757-61.
rhosis: effect of ursodeoxycholic acid. Hepatology 1990;11:12-5.
131. Javett SL. Azathioprine in primary sclerosing cholangitis. Lancet 1971;1:
102. Almasio P, Bortolini M, Pagliaro L, Coltorti M. Role of S-adenosyl-L-
methionine in the treatment of intrahepatic cholestasis. Drugs 1990;40:
132. Wagner A. Azathioprine treatment in primary sclerosing cholangitis. Lan-
Suppl 3:111-23.
cet 1971;2:663-4.
103. Hanid MA, Levi AJ. Phototherapy for pruritus in primary biliary cirrhosis.
133. Leiser A, Kadish U. Beneficial effect of colchicine in a case of sclerosing
Lancet 1980;2:530.
cholangitis. Am J Med Sci 1986;291:416-8.
104. Borkje B, Vetvik K, Odegaard S, Schrumpf E, Larssen TB, Kolmannskog
134. Polter DE, Gruhl V, Eigenbrodt EH, Combes B. Beneficial effect of
F. Chronic pancreatitis in patients with sclerosing cholangitis and ulcerative
cholestyramine in sclerosing cholangitis. Gastroenterology 1980;79:326-33.
colitis. Scand J Gastroenterol 1985;20:539-42.
135. Wiesner RH, Steiner B, LaRusso NF, Lindor KD, Baldus WP. A con-
105. Epstein O, Chapman RWG, Lake-Bakaar G, Foo AY, Rosalki SB, Sherlock
trolled clinical trial evaluating cyclosporine in the treatment of primary
S. The pancreas in primary biliary cirrhosis and primary sclerosing cholan-
sclerosing cholangitis. Hepatology 1991;14:Suppl:63A. abstract.
gitis. Gastroenterology 1982;83:1177-82.
136. Langnas AN, Grazi GL, Stratta RJ, et al. Primary sclerosing cholangitis:
106. Hay JE, Wiesner RH, Shorter RG, LaRusso NF, Baldus WP. Primary scle-
the emerging role for liver transplantation. Am J Gastroenterol 1990;85:
rosing cholangitis and celiac disease: a novel association. Ann Intern Med
137. McEntee G, Wiesner RH, Rosen C, Cooper J, Wahlstrom E. A compara-
107. Sartin JS, Wiesner RH, LaRusso NF. Fat-soluble vitamin deficiencies in
tive study of patients undergoing liver transplantation for primary scleros-
primary sclerosing cholangitis. Gastroenterology 1987;92:1615. abstract.
ing cholangitis and primary biliary cirrhosis. Transplant Proc 1991;23:
108. Munoz SJ, Heubi J, Deems R, Ross R, Maddrey WC. Vitamins D and E
deficiency in primary sclerosing cholangitis: mechanism, frequency and re-
138. Letourneau JG, Day DL, Hunter DW, et al. Biliary complications after liver
lation to deficiency in other lipid soluble vitamins. Gastroenterology 1991;
transplantation in patients with preexisting sclerosing cholangitis. Radiol-
109. Hay JE, Lindor KD, Wiesner RH, Dickson ER, Krom RAF, LaRusso NF.
139. Hunter EB,Wiesner RH, MacCarty RL, et al. Does primary sclerosing cho-
Metabolic bone disease in primary sclerosing cholangitis. Hepatology
langitis recur after liver transplantation? Gastroenterology 1989;96:Suppl:
A610. abstract.
110. May GR, Bender CE, LaRusso NF, Wiesner RH. Nonoperative dilatation
140. Gavaler JS, Delemos B, Belle SH, et al. Ulcerative colitis disease activity
of dominant strictures in primary sclerosing cholangitis. AJR Am J Roent-
as subjectively assessed by patient-completed questionnaires following
orthotopic liver transplantation for sclerosing cholangitis. Dig Dis Sci
111. Johnson GK, Geenen JE, Venu RP, Schmalz MJ, Hogan WJ. Endoscopic
treatment of biliary duct strictures in sclerosing cholangitis: a larger se-
141. Higashi H, Yanaga K, Marsh JW, Tzakis A, Kakizoe S, Starzl TE. Devel-
ries and recommendations for treatment. Gastrointest Endosc 1991;37:
opment of colon cancer after liver transplantation for primary sclerosing
cholangitis associated with ulcerative colitis. Hepatology 1990;11:477-80.
The New England Journal of Medicine
Downloaded from nejm.org on April 22, 2013. For personal use only. No other uses without permission.
Copyright 1995 Massachusetts Medical Society. All rights reserved.
Source: http://www.gustavostork.com.ar/doc/profesionales_bibliografia/higado/colangitis%20esclerosante%20primaria%20revision%20nejm%202013.pdf
The pharmaceutical industry in Brazil Market overview and trends Overview of the for labor began to stabilize in 2013 and started to lose some of its vigor and there is a feeling among specialists that the market will tend towards a rise in unemployment. Therefore, some reduction in salary levels can be expected in the local
Saliva Direct Cup size: Kit Oral Fluid Drugtest THC - COC - OPI - MET - AMP - BZD THC - COC - OPI - MET - AMP - MTD All Kits come Security Seal for either the Sample Cup or the resealable Device Bag Saliva Direct Cup