Kamagra gibt es auch als Kautabletten, die sich schneller auflösen als normale Pillen. Manche Patienten empfinden das als angenehmer. Wer sich informieren will, findet Hinweise unter kamagra kautabletten.
Adcs.org

Alzheimer's Disease Information Network
ADIN Monthly E-News
For more informa-
tion on clinical
trials, visit the
ADEAR Clinical
Trials Website
Alzheimer's Disease
Cooperative Study
March 2016
_
Can Common Heartburn Drugs Raise Dementia Risk?
This newsletter is pre-
pared monthly by the
Alzheimer's Disease
A widely used class of medications that treat acid reflux has been tied to dementia. In the
Cooperative Study at
the University of
February 15 JAMA Neurology, scientists led by Britta Haenisch, at the German Center for
California San Diego.
Neurodegenerative Diseases in Bonn, reported that elderly people who regularly used pro-
Content is intended to
ton pump inhibitors (PPIs) had a 44 percent greater risk of developing dementia than peo-
educate the public
ple who didn't use these drugs. Although correlative, the results suggest that avoiding these
about AD research
medications could help prevent cognitive decline, the authors claim.
endeavors and other
"This is an interesting study and certainly an attention-grabber," said Ralph Nixon, New
York University School of Medicine. While the paper may make people worry about being
Questions or
on PPIs, they will need to balance this degree of dementia risk with a need to lower risks
associated with acid-related disorders, which may be substantial, he told Alzforum.
Please email:
_
PPIs such as omeprazole, pantoprazole, and lansoprazole treat gastroesophageal reflux dis-
ease and peptic ulcers—some would say far more often than necessary. Studies estimate
that 3 to 5 percent of the population over age 65 takes PPIs, which are among the top-
selling drugs worldwide. PPIs are available by prescription and over-the-counter, and their
use is growing, especially in older people.
These drugs bind and inhibit the cellular gastric proton pump that supplies the stomach with acid. Found in all cells, several types of proton pumps use energy from ATP to trans-
port ions across membranes. An example is the vacuolar-type adenosine triphosphatase (V-ATPase). It acidifies lysosomes so that they can degrade unwanted proteins. PPIs weakly
block those lysosomal pumps. In rodents, these drugs have been found to cross the blood-brain barrier, leading some scientists to wonder if they affect cells in the brain .
Analyzing data from the longitudinal AgeCoDe study, which follows more than 3,000 peo-ple age 75 or older in primary care settings in Germany, Haenisch and colleagues had previ-
ously found that those taking PPIs were at a 38 percent greater risk of developing dementia 18 months later.
Continued on next page.
Heartburn and Dementia cont'd….
To expand on their finding, co-first authors Willy Gomm and Klaus von Holt exam-ined longitudinal medical records from the massive database of the public health in-
surer Allgemeine Ortskrankenkassen, which was founded in 1884 and insures a third of the German population. The researchers tracked people aged 75 years and older
who were living dementia-free from 2004 to 2011. Of 73,679 people, 2,950 had taken PPIs long-term, while 70,729 took none. After adjusting for factors such as age, gen-der, depression, diabetes, and stroke, people on PPIs were 44 percent likelier to de-
velop various types of dementia, including Alzheimer's and vascular dementia. An-other 66,008 people in the database used PPIs occasionally; their risk rose by 16 percent.
An accompanying editorial puts these numbers in perspective. A 44 percent increase
in dementia among PPI users in the United States could translate to 10,000 addi-tional new cases every year among people aged 75 to 84, assuming about 3 percent of them took these acid reflux meds, noted Lewis Kuller, University of Pittsburgh. Kuller
cautioned that the link may be coincidental. General drug use in this population may signal poor health overall, and the reasons that lead people to take PPIs could make also them more vulnerable to dementia. The association needs to be validated in large
cohorts and tested in case-control studies, he wrote. Nevertheless, Kuller acknowl-edges that a causal link is plausible.
Haenisch and colleagues point out that PPI use can lead to vitamin B12 deficiency, which has been associated with cognitive decline. The PPI lansoprazole has been re-ported to augment processing of the amyloid precursor protein by β- and γ-secretases in mice, which would imply increased amyloid production in the brain, though an-other study reported that lansoprazole acts as an LXR agonist, which would imply amyloid reduction
Continued on next page.

Heartburn and Dementia cont'd….
Researchers in Iran proposed years ago that PPIs cross the blood-brain barrier and
reduce the acidity of microglial lysosomes by blocking their V-ATPase pumps, making them less able to break down fibrillar brain amyloid . Michael Heneka, German Cen-
ter for Neurodegenerative Disease, Bonn, commented that there is no evidence to
suggest treatment with PPIs makes microglial lysosomes less acidic in vivo.
Nixon, who studies neuronal and glial lysosomes in AD, noted that PPIs enter the
brain poorly even at high doses, and that they have much lower affinity for the micro-
glial V-ATPase than they do for the gastric proton pump. Unpublished data from
Nixon's lab suggests that even if a PPI got into the brain, cells there would compen-
sate by upregulating V-ATPase expression. Frederick Maxfield, Weill Cornell Medical
College, New York, agreed that PPIs are unlikely to reach sufficiently high concentra-
tions in the brain to affect microglial lysosomes. However, he and Nixon said the po-
tential link is worth investigating further. Even a small decrement in lysosomal func-
tion could be meaningful if the lysosome is already compromised, Nixon said.
Other mechanisms could explain the association with dementia. For one, Peter Scott, University of Michigan, Ann Arbor, proposed that since lansoprazole inhibits
p-glycoprotein, which may help shuttle Aβ from the brain to the blood, amyloid might
accumulate as a result (ott agreed that further clinical
studies are warranted (see full comment on original article at AlzForum). —Gwyneth Dickey Zakaib
This article originally appeared on Alzforum. Reprinted with permission.
To view the original article please visit:
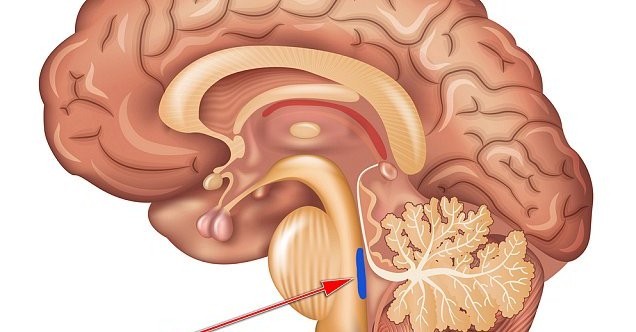
Researchers Pinpoint Brain Region as ‘Ground Zero' of
Alzheimer's Disease
By Beth Newcomb, University of Southern California
A critical but vulnerable region in the brain appears to be the first place affected by late onset Alzheimer's disease and may be more important for maintaining cognitive
function in later life than previously appreciated, according to a scien-tific literature.
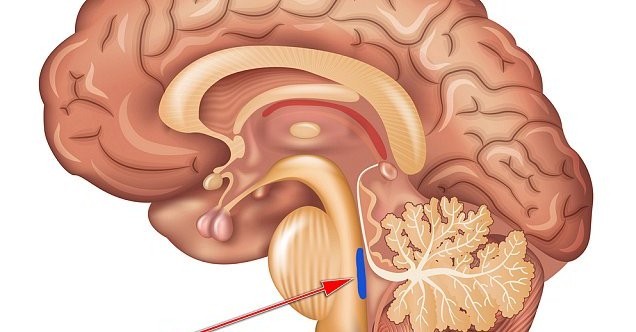
The locus coeruleus is a small, bluish part of the brainstem that releases norepineph-
rine, the neurotransmitter responsible for regulating heart rate, attention, memory and cognition. Its cells, or neurons, send
branch-like axons throughout much of the brain and help regulate blood vessel activ-
ity. Its high interconnectedness may make it more susceptible to the effects of toxins
and infections compared to other brain regions, lead author id.
Mather, professor of gerontology at the USC Davis School of Gerontology, added that the locus coeruleus is the first brain region to show tau pathology — the slow-
spreading tangles of protein that can later become telltale signs of Alzheimer's. Though not everyone will get the disease, autopsy results indicate that most people
have some initial indications of tau pathology in the locus coeruleus by early adult-hood, she added.
The norepinephrine released from the locus coeruleus may contribute to preventing Alzheimer's symptoms. Studies conducted with rats and mice have shown that nore-pinephrine helps protect neurons from factors that kill the cells and accelerate Alz-
heimer's, such as inflammation and excessive stimulation from other neurotransmit-ters.
Norepinephrine is released when someone is engaged in or mentally challenged by an activity, whether it's solving problems in the workplace, completing a word puzzle or playing a difficult piece of music.
"Education and engaging careers produce late-life ‘cognitive reserve,' or effective brain performance, despite encroaching pathology," said Mather, who holds a joint appointment as professor of psychology at the USC Dornsife College of Letters, Arts and Sciences. "Activation of the locus coeruleus-norepinephrine system by novelty and mental challenge throughout one's life may contribute to cognitive reserve."
"The Locus Coeruleus: Essential for Maintaining Cognitive Function and the Aging Brain" appears in Trends in Cognitive Sciences and was funded by the National Insti-tutes of Health grant RO1AG025340. The study was co-authored by Professor Emeri-tus Carolyn Harley of the Memorial University of Newfoundland.

UC Davis School of Nursing partners with statewide nursing
home organization to improve dementia care
Researchers from the Betty Irene Moore School of Nursing at UC Davis collaborate
with the California Association of Health Facilities (CAHF) on a quality improvement initiative aimed at improving dementia care in skilled nursing facilities. Associate
Adjunct Professor Debra Bakerjian and Assistant Professor Elena O. Siegel will conduct independent research in a project aimed at improving dementia care.
Associate Adjunct Professor Debra Bakerjian, left, and Assistant Professor Elena O. Siegel
conduct independent research in a project aimed at improving dementia care in nursing homes.
Approximately 70 percent of residents with dementia living in nursing homes are re-
ported to have significant behavioral and psychiatric symptoms. Historically, one of the first lines of treatment was antipsychotic drugs, which are now not recommended for residents with dementia. This three-year "CAHF Improving Dementia Care
through Music & Memory" project will use iPods to re-introduce nursing home resi-dents to their favorite, personalized music to improve their day-to-day life and deter-
mine if familiar tunes can reduce the need for medication and improve their quality of life. "We are very interested in having a better understanding of whether or not the pro-gram can help reduce use of antipsychotics and whether the program is sustainable over time," Bakerjian explained. "Many short-term studies indicate positive out-
comes, but this will be the first comprehensive, 36-month study to determine if it works, how it works and if practices can be sustained for this and other quality im-provement programs in long-term care facilities."
The $1.4 million grant program is funded from civil monetary penalties ― fines col-
lected in California for nursing home violations. CAHF will distribute Music & Mem-ory℠ to 4,500 residents across 300 nursing homes in order to document its effects on reducing antipsychotic medication for people with dementia. First, the UC Davis team will evaluate if the music program works and how nursing homes implement it.
Cont'd on next page.

UC Davis cont'd….
Second, researchers will independently test two to three Quality Assurance Perform-ance Improvement (QAPI) tools to support implementation of the program. QAPI is
essentially a roadmap developed by the Centers for Medicaid & Medicare Services re-quired by nursing homes to improve the quality of life, care and services. Whereas the
federal guidelines are broad, Bakerjian and Siegel will tailor them specifically for the music program.
Finally, they will study, document and report on organizational factors present in the success or failure of the adoption and sustainment of Music & Memory℠ in the par-ticipating facilities. CAHF leaders and UC Davis researches hope to document the ef-
fects of this program and identify ways to help skilled nursing centers sustain the gains they make in all of their quality improvement efforts.
"We look forward to our partnership with two, well-respected UC Davis nurse re-searchers who have great expertise in the science of quality improvement in skilled
nursing settings," said Jocelyn Montgomery, a registered nurse and CAHF's lead on the project. "Their work will allow us to examine organizational practices that influ-ence the success or failure of projects such as Music & Memory℠ in the nursing-home setting."
Bakerjian's more than 25 years of one-on-one, long-term patient experience, coupled
with Siegel's focus on administrative and managerial leadership in long-term-care settings, bring expertise to quantitatively and qualitatively document the impact of
the program and identify strategies to spread and sustain the program as a quality assurance/performance improvement project.
Continued on next page…….

UC Davis cont'd…….
"We both dedicate our careers to improving quality of care and quality of life of older
adults in nursing homes, using different perspectives," Siegel added. "Understanding how the clinical and administrative components of care delivery practices work to-gether is essential to improving quality."
In the first phase of the study, School of Nursing researchers pilot test the various processes for the study and will consult with CAHF on development of criteria for
which facilities are selected. They will then collect data and independently
evaluate how facilities are implementing the program and determine the chal-lenges that impede success or organiza-
tional structures that foster success. Additionally, Siegel and Bakerjian will develop and test an intervention to
support nursing homes in the imple-mentation and sustainability of the MU-
SIC & MEMORY℠ program. The inter-vention includes a quality-assurance tool consistent with upcoming regula-
tory requirements for all nursing homes that care for Medicare and Medicaid beneficiaries.
"We know nursing homes face many
challenges with implementing and sus-taining quality improvement initiatives, and translating new regulations into
practice brings another set of chal-
lenges. Our intervention offers nursing homes a practical resource to both translate and integrate the upcoming QAPI regulatory requirement into their everyday work
practices," Siegel said. "This project exemplifies our research goals to support prac-tice and policy efforts to improve nursing home quality and value."
"California is a microcosm of the rest of the nation in terms of diversity, its popula-tion of older adults and the number of nursing homes that operate throughout the
state," Bakerjian added. "As all nursing homes will be mandated to implement QAPI programs, this work will enable us to develop guidelines for this project and many others that may improve quality in the long run."
Courtesy of that UC Davis.
Lipid Based Diets Effectively Combat Alzheimer's in Mouse
Models of Disease
Researchers have devised several lipid-based diets aimed at slowing down
progression and relieving symptoms of Alzheimer's disease.
Alzheimer´s disease (AD) is the most common disease underlying memory problems and dementia in the elderly. One of the invariable pathologies in AD is degeneration of
cholinergic synapses in brain cortex and hippo-campus. Despite enormous effort to find out an efficient treatment, current pharmacological
interventions are limited to a few drugs that al-leviate symptoms but do not slow down the un-
derlying disease processes. These drugs include inhibitors of cholinesterases, enzymes that de-grade the neurotransmitter acetylcholine, or
memantine, a modulator of glutamate neuro-transmission.
It is generally accepted that lifestyle and particularly dietary habits influence mental health, and prevalence and progression of AD. Numerous epidemiological studies have
revealed profitable effects of dietary intake of especially fish oil on cognitive decline during aging and dementia.
Within the EU-funded project LipiDiDiet (FP7-211696), therapeutic and preventive im-pact of nutritional lipids on neuronal and cognitive performance in aging, Alzheimer´s disease and vascular dementia, researchers devised several lipid-based diets aimed at slowing down progression and relieving symptoms of AD. Short-term (3 weeks) feeding of young adult APPswe/PS1dE9 mice (transgenic mouse model of AD) with experimen-tal diets containing fish oil or stigmasterol reversed the decrease in responsiveness of hippocampal muscarinic receptors to acetylcholine compared to their non-transgenic littermates. Only fish oil based diet enriched with nutrients supporting neuroprotection (Fortasyn diet) increased in addition the density of muscarinic receptors and cholinergic synapses in the hippocampus.
These findings yield important proof-of-principle evidence that regular intake of spe-cific dietary components may help to prevent some of the key early functional changes that take place in the Alzheimer brain. These findings support viability of the dietary approach in AD.
This article appeared in Neuroscience News.
Original Research: or "Lipid-Based Diets Improve Muscarinic Neuro-
transmission in the Hippocampus of Transgenic APPswe/PS1dE9 Mice" by Helena Janickova, Vladimir Rudajev, Eva Dolejsi, Hennariikka Koivisto, Jan Jakubik, Heikki Tanila, Esam E. El-Fakahany and Vladimir Dolezal in Current Alzheimer Research. Published online February 20
The following studies will be enrolling in 2016. For
information on these studies please visit :
Follow us on Twitter
Connect with us at
Source: http://www.adcs.org/Research/doc/eNewsLetter/ADIN_E-News_Mar_2016.pdf
TitelDer Name »Esther« diente zu allen Zeiten unverändert als Titel dieses Buches. Die Bücher Esther und Ruth sind die einzigen Bücher des AT, die nach Frauen benannt sind. Wie die Sprüche Salomos, Obadja und Nahum wird das Buch Esther im NT nicht erwähnt oder zitiert. »Hadassa« (2,7) bedeutet »Myrte« oder »Braut« und war der hebräische Name von Esther, der entweder vom
Discovery News for Discovery Health members Discovery's Average Annual Increase for 2013: 10.9% September 2012 This email is written by an Contribution increases range from 11.9% on Executive, Comprehensive, independent commentator and not Priority, and Coastal plans, to 9.8% on Classic and Essential Saver, by Discovery Health. Any Discovery