Kamagra gibt es auch als Kautabletten, die sich schneller auflösen als normale Pillen. Manche Patienten empfinden das als angenehmer. Wer sich informieren will, findet Hinweise unter kamagra kautabletten.
Doctorhuff.net


Practice Management and Human Relations
Ethical decision-making for multiple
prescription dentistry
Kevin Huff, DDS, MAGD n Marlene Huff, PhD, RN n Constantin Farah, DDS, MSD
Technology provides a selection of treatment choices for dental
This article presents four case studies that illustrate the process of
problems. Dental ethics must be applied to the development of a
ethical decision-making for the appropriate treatment.
treatment plan and the selection of methods. Treatment options
Received: August 2, 2007
should consider the patient's circumstances and desires as well
Accepted: September 19, 2007
as the dentist's decision as it relates to best practices in dentistry.
The art and science of dentistry a given patient may be different for mendations. The American Dental
has progressed very rapidly
the same patient at different times
Association's Code of Ethics lays
since the introduction of the
in his or her life.
the groundwork; how the Code is
high-speed handpiece in the 1950s.1
Recognizing the importance of
applied reflects the dentist's indi-
There has been a paradigm shift
optimal oral health, coupled with
vidual values (see the table).3
from paternalistic management
the rapid advancements in technol-
It often is possible to achieve
of obvious problems to a medical
ogy, may lead the practitioner to
similar results from the application
model of dental care, which includes
be overzealous in treatment. A
of different approaches to treatment
prevention and management
comprehensive plan of care that is
or prevention.4 Having multiple
of dental disease and prosthetic
appropriate for the patient should
options leads to what Sadowsky
rehabilitation to restore normal
include the application of ethical
cal ed the "moral dilemma of the
oral function. Discovery of the
principles in the development,
multiple prescription in dentistry."5
relationship between oral health and
acceptance, and implementation of
One approach may be considered
systemic disease has raised awareness
treatment. The science of dentistry
more beneficial than another at
concerning the importance of oral
makes it possible to offer multiple
a given time. The options that a
health. In 2000, the U.S. Surgeon
options to patients; however, the
dentist offers and a patient selects
General cited oral health as a major
art of dentistry includes the need
can be influenced by changes in the
concern.2 Advancements in tech-
to communicate with the patient
patient's lifestyle or physical condi-
nology offer a variety of solutions
and to apply ethical principles
tion or a change in terms of available
for managing similar dental situa-
when making treatment recom-
treatment methods. The clinician
tions and it is incumbent upon each
practitioner, as a member of an ethi-
cal profession, to educate patients
about their appropriate treatment
Table. Ethical principles.3
options, allowing them to make
autonomous treatment choices that
are in their best interest.
Patient autonomy ("self-governance")
The dentist has a duty to respect the patient's
It generally is understood that
rights to self-determination and confidentiality
many treatment options are avail-
Nonmaleficence ("do no harm")
The dentist has a duty to refrain from harming
able for any given dental condition.
A definite decision-making process
Beneficence ("do good")
The dentist has a duty to promote the patient's
helps to determine the appropriate-
ness of each treatment modality. It
Justice ("fairness")
The dentist has a duty to treat people fairly
also must be acknowledged that the
Veracity ("truthfulness")
The dentist has a duty to communicate truthful y
ethically appropriate treatment for
538 September/October 2008 General Dentistry www.agd.org
should share his or her reasons
col to matters of human concern.
Informed consent is an important
for recommending one treatment
Normative ethics refers to an area
component of decision-making;
option over another; however, other
of inquiry that investigates right or
however, sharing all of the details
reasonable treatment options should
wrong conduct, looking at ethical
about a case may complicate the
be presented as well. An ethical
principles and rules commonly
process. The dentist must decide
decision-making process is necessary
associated with the situation and
how much information to share
when discussing the risks and ben-
assessing duties and obligations.
with the patient. For example, fair
efits for the patient and arriving at an
Autonomy includes self-determi-
fee structures are included in the
appropriate decision for treatment.
nation, confidentiality, and the right
principle of veracity; misrepresenta-
Professional responsibility includes
to select and/or to refuse treatment.
tion is considered to be untruthful.
acting in a manner that promotes
The dentist must inform the patient
Beneficence and nonmaleficence
"good" for the patient. Ethical prin-
of all reasonable and appropriate
include benefits versus harm. Com-
ciples should be the underpinning
treatment options. This way, the
bined, this dichotomy is a utilitarian
for the plan of care and should affect
patient is actively involved in treat-
principle that includes acting in a
al choices made concerning care
ment decisions. Dentists serve not
manner that promotes the good
only as diagnosticians but also as
of the patient. Even though a
Dentistry is a moral profession,
educators. Trust may be weakened
particular technique could address
guided by normative principles.4
if dentists limit the amount of infor-
an immediate problem, the overall
As a result, dentists are obligated
mation patients receive.
effect may harm the patient in a way
to choose a course of treatment
Too much information also can
that is not immediately apparent.
that allows them to be "caring
present a problem.9 The dentist
Weinstein has proposed a process
and fair in their contact with
must use good judgment when
for making ethical decisions for
patients."3 Although increased
obtaining informed consent.
patient care. This process involves
commercialism may be difficult to
Education may inform patients as
gathering relevant facts, including
avoid, patient autonomy should
to what they need but that may
medical history and social factors,
be the overwhelming decision-
not be what they want. Autonomy
ascertaining possible treatment
making principle. Preservation
involves decision-making from both
options, and answering questions
of the profession of dentistry and
the patient and the dentist. The
concerning what course of treat-
the self-policing autonomy that it
right to refuse treatment is inherent
ment should be followed and why.7
enjoys necessitates adherence to the
in the principle of autonomy.10
The first step involves gathering
normative picture.7 Members of the
Justice includes trust and kind-
all of the relevant facts, including
dental profession and of the com-
ness. Trust is built upon being
medical history, dental history, and
munity at large expect dentists to
honest; patients trust that dentists
social factors. Relevant ethical prin-
act ethically, according to a balance
have a current working knowledge
ciples are identified and a decision
of certain norms: nonmaleficence,
of modern dental techniques. As a
is made regarding conflicts. For
beneficence, justice, veracity, and
result, continuing education is an
example, when a patient requests
respect for patient autonomy.3 The
ethical obligation of the dental pro-
a treatment that would knowingly
personal virtues of the dentist and
fession (one which may or may not
render his or her condition more
the intrinsic values of the profession,
be required by law). If the patient
unstable or uncertain than at the
the patient, and society must be
requires treatment that is beyond
time of the initial visit, the personal
considered when choosing appropri-
the skill of the primary dentist,
virtues of the dentist and the
ate treatment for any given situation
it is expected that the dentist will
principles of nonmaleficence may
(see the table).3
refer the patient to more qualified
conflict with the need to respect the
Codes of ethics describe expected
clinicians. Ethical decision-making
patient's autonomy.
standards of behavior for self-
reduces the tendency toward over-
Next, all of the treatment options
policing professions (dentistry,
treatment; that is, a dentist should
available for the given situation
medicine, nursing, and so forth).
not perform a procedure that is
should be ascertained (for example,
Ethics also may be considered a
not indicated simply to please the
a Class II carious lesion may be
mode of inquiry for processing the
treated with an interim glass
moral dimensions of an issue.8 To
Veracity includes judgment
ionomer restoration, an interim
engage in ethics is to apply a proto-
concerning what to tell the patient.
zinc oxide/eugenol restoration,
www.agd.org General Dentistry September/October 2008 539



Practice Management and Human Relations Ethical decision-making
a composite resin restoration, an
amalgam restoration, a porcelain
inlay, a resin inlay, or a gold inlay).
Finally, the dentist selects the
appropriate treatment option by
answering the questions "What
should be done?" and "Why should
it be done?" Although it is inherent
in the process, perhaps a fourth
step should be added: to arrive at a
treatment option that is acceptable
to both the patient and the dentist.
Autonomy, or the patient's decision
about treatment, is an important
This article presents four case
reports that illustrate how ethical
Fig. 1. A 45-year-old woman with a loose maxil ary anterior FPD from teeth No. 6–9.
principles were applied in the deci-
sion-making process to determine
the most appropriate treatment.
The authors acknowledge that the
treatment rendered is not consid-
ered to be ideal in these situations
according to accepted standards.
However, in each case, ideal treat-
ment options were presented as part
of the informed consent process.
Weinstein's model was used to guide
Case report No. 1
A 45-year-old woman sought treat-
ment for a failing four-unit fixed
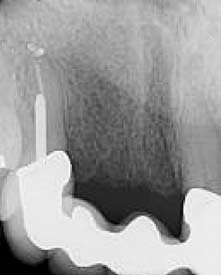
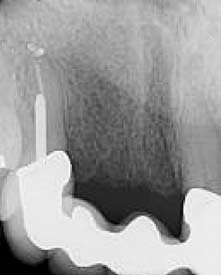
Fig. 2. A radiograph and occlusal view of the patient, indicating the recurrent caries that caused
partial denture (FPD) that had
the existing FPD abutment to fail. The cavosurface of the healthy tooth after excavation is at the
been placed more than ten years
osseous crest.
earlier (from teeth No. 6–9). She
had recurring dental caries under
the distal abutment crown that
was inaccessible for repair without
removing the FPD (Fig. 1). The
contraindication to dental surgery.
lengthening surgery, individual
right maxillary canine abutment
The patient wanted to receive the
abutment crown therapy for teeth
was mobile and fractured at the
least costly restoration as quickly as
No. 6 and 9, and removable partial
gingival margin (Fig. 2); in addi-
possible. The function, esthetics,
denture (RPD) therapy. A second
tion, the patient had an Angle's
and durability of her previous FPD
option involved the aforementioned
Class I occlusion with stable centric
were acceptable to her. She was
endodontic therapy and crown-
occlusion and anterior guidance.
opposed to any type of removable
lengthening surgery plus FPD
The patient had received a nine-
therapy, utilizing teeth No. 6 and 9
unit, four implant-supported FPD
Based on the patient's wishes, three
as abutments. A third option would
(from teeth No. 19–27) more
treatment options were available.
involve extracting the right canine
than a year earlier; it was in good
One option involved endodontic
and placing implants in the sites of
condition. Medically, there was no
therapy on the right canine, crown-
teeth No. 6 and 8, with an implant-
540 September/October 2008 General Dentistry www.agd.org

that have improved the feasibility of
fixed prostheses and in an era that
places a high value on esthetics.
The costs associated with complex
restoration of severely compromised
teeth, the associated morbidity,
and the unfavorable comparative
prognoses suggest a need to consider
utilizing dental implant therapy
and/or FPD therapy as alternatives.
The decision should be based on the
Fig. 3. The patient in Figure 2 after receiving appropriate endodontic therapy and phased FPD
patient's medical history and socio-
therapy. Note the favorable tissue response and esthetic appearance created by wel -developed
economic status, as well as proper
ethical principles.
Ethical considerations
Autonomy
The patient was presented with all
supported FPD and an independent
and a full-coverage restoration
possible treatment options, includ-
crown on tooth No. 9. After thor-
subsequent to endodontic therapy.
ing the option to do nothing with
ough discussion, the patient chose
For adequate retention, it generally
her failing FPD. As with all of the
the second of the three plans.
is understood that the final crown
cases presented in this article, the
The existing FPD was removed,
margin should be at least 2.0 mm
patient was well-educated through
endodontic therapy was completed
apical to the cavosurface margin of
discussion and commercially
on tooth No. 6, and a pre-fabricated
the core, creating a ferrule. This
prepared video presentations. In
post and a bonded resin core were
complex approach to restoration is
addition, she had received implant
placed. A provisional FPD was
technique-sensitive and the progno-
therapy on her mandibular arch
fabricated and crown-lengthening
sis for the tooth as an abutment for
previously without complication.
surgery was completed from teeth
No. 6–11. After ten weeks of tissue
For healthy biologic width, there
healing, a porcelain-fused-to-high
must be adequate space between the
The patient had been treated previ-
noble metal FPD was fabricated
crown margin and the crestal bone.
ously with a very functional and
and luted with resin-reinforced glass
Osseous crown-lengthening surgery
esthetic FPD. FPD therapy has
ionomer cement (Fig. 3).
is indicated when coronal tooth
been utilized for many years in
The patient had enjoyed acceptable
structure loss is significant enough to
conventional dentistry and there
success with her previous four-
compromise the biologic width when
was no absolute contraindication
unit FPD and understood that an
an ideal restoration is placed. This
for FPD therapy, since the abut-
implant-supported prosthesis would
procedure is a subtractive approach
ment teeth were prepared and
provide the best longevity and that
that requires removing bone in an
would have required crown therapy
crown-lengthening surgery is a sub-
era when efforts are conscientiously
regardless of the therapy selected.
tractive therapy rather than additive.
being made to provide additive treat-
The risks of crown-lengthening
ments that regenerate bone.
surgery (and the fact that bone
Dental considerations of
When a tooth is severely com-
would need to be removed) were
promised, an alternative to the
discussed thoroughly. The patient
Periodontally sound teeth that
aforementioned therapy would be
clearly understood her condition
have endured severe structural
to extract the tooth and replace it
and made an educated choice. The
loss (that is, more than 50% of
with either an RPD or an implant-
same clinicians who completed the
the coronal tooth structure) and
supported prosthesis. Although
previous implant therapy and pros-
still are deemed restorable usually
RPDs once were common practice,
thesis presented and performed this
require either a prefabricated or
they have fallen out of favor in light
particular treatment, so the patient
laboratory-made post and core
of modern materials and techniques
was not subjected to outside bias.
www.agd.org General Dentistry September/October 2008 541

Practice Management and Human Relations Ethical decision-making
Fig. 5. The patient in Figure 4, after receiving a zirconia-based FPD that replicated the original
Fig. 4. An anterior view and a radiograph of a 64-year-old woman with failing restorations on her
position of the natural dentition in accordance
central incisors.
with the patient's esthetic demands.
a stable, esthetic solution for her in
options were considered. The first
Although it may be argued that
accordance with her chief concerns.
option involved endodontic retreat-
crown-lengthening surgery removes
ment, bonded resin cores, and crown
bone, it also would allow the
Case report No. 2
therapy on teeth No. 8 and 9. The
dentist to save the canine. Since all
A 64-year-old woman sought treat-
second option involved extracting
procedures were performed accord-
ment for failing restorations of her
teeth No. 8 and 9, fol owed by
ing to accepted protocols (with
maxillary central incisors (teeth No.
phased FPD therapy. The third
2.5 mm of ferrule for abutment
8 and 9). External root resorption
option involved extracting teeth No.
retention on tooth No. 6, while the
was evident (Fig. 4). The patient
8 and 9, followed by phased remov-
abutment teeth had been prepared
had an Angle's Class II Division
able denture therapy. The fourth
as abutments previously), no harm
II occlusion and a moderate shift
option involved extraction of teeth
was caused to the patient. Healing
from centric occlusion to maximum
No. 8 and 9, fol owed by implant
discomfort and surgical involvement
intercuspal position without pain.
replacement therapy for teeth No. 8
were similar to what would have
There was steep anterior guidance
and 9 and implant-supported crowns.
resulted from implant therapy.
and a high maxillary lip attachment.
The patient selected extraction
The patient was in good health with
and the FPD. Once that decision
a history of seasonal sinusitis and
was made, teeth No. 8 and 9 were
The benefits of implant therapy
was not taking any medications on
extracted and the maxil ary lateral
were superseded by the patient's
a regular basis. Her dental history
incisors were prepared for abutment
concerns about the short-term cost
included multiple minimally accept-
crowns. Synthetic ridge preservation
of therapy. A plan for failure was
able alloy and resin restorations.
material (Bioplant, Kerr Dental,
discussed with the patient, who
More than 40 years earlier, the
Orange, CA; 800.537.7123) was
clearly understood that the lifespan
patient had received endodontic
placed according to standard proto-
of the FPD was expected to be
therapy on teeth No. 8 and 9; this
col and a provisional FPD was fab-
shorter than that of an implant-
therapy was followed by the placing
ricated to al ow for adequate tissue
supported prosthesis. The patient
of porcelain veneers that had been
maturation. The preparations on
understood that failure could
repaired multiple times. She had a
the lateral incisors were refined and a
require either a removable prosthesis
history of sporadic recall visits and
four-unit zirconia-substructure FPD
or a more costly implant-supported
poor oral hygiene. The patient said
(Lava, 3M ESPE, St. Paul, MN;
prosthesis. The patient benefited
that she wanted "whiter" incisors
888.364.3577) was fabricated for
from crown-lengthening, endodon-
but she did not want the position or
teeth No. 7–10. The FPD was luted
tic therapy, and conventional FPD
shape of her teeth to change.
with resin-reinforced glass ionomer
therapy because this plan provided
Given these factors, four treatment
cement (Fig. 5).
542 September/October 2008 General Dentistry www.agd.org
understood that the lifespan of an
FPD therapy has been utilized in
FPD most likely would be shorter
conventional dentistry for many
than that of an implant-supported
years, with predictable outcomes.
prosthesis. The patient understood
No absolute contraindication
that in the event of failure, her
for FPD therapy exists in this
only choices of therapy might be
particular case, although it would
a removable or implant-supported
require altering the abutment teeth.
prosthesis. The patient benefited
However, when the patient's desired
from phased FPD therapy in this
esthetic outcome was considered
case because it was the most predict-
carefully, there were reasonable
able treatment option for meeting
contraindications for an implant-
her demands and expectations.
retained prosthesis or RPD therapy.
The dentist and patient had a frank
Case report No. 3
Fig. 6. A radiograph of a 62-year-old man with
discussion about the difficulties that
A 62-year-old man had a failing
a failing cantilever FPD. No photograph was
would be encountered in meeting
cantilevered FPD that replaced the
the patient's esthetic demands
left maxillary central incisor (Fig.
and the expected results of each
6). Tooth No. 8, the single abut-
treatment option were reviewed.
ment, was mobile and elicited pain
The patient clearly understood her
on percussion. An Angle's Class I
condition and made an educated
occlusion existed with stable centric
The prognosis of re-restoring teeth
choice. No guarantees or promises
occlusion and anterior guidance.
No. 8 and 9 was guarded due to the
were made. It was made clear to
The patient had a history of acid
lack of substantial remaining root
the patient that her home compli-
reflux, asthma, chronic sinusitis,
structure and external root resorp-
ance would determine the success
primary tension headaches, and
tion. The patient's esthetic demands
of any treatment option and the
arthritis; his current medications
and existing anatomy created a
relative fees for each treatment
included Prilosec (AstraZeneca,
contraindication for RPD therapy.
option were discussed openly and
Westborough, MA; 800.236.9933)
It was unclear whether the patient
and lactase. The patient had a his-
would be satisfied with implant
tory of excellent oral hygiene and
therapy due to the uncertain gin-
compliance with recommended
gival esthetic outcome, which cur-
Since all procedures were performed
dental treatment. Seven years
rently is a risk factor for implants in
according to accepted protocols
earlier, the same dentist had placed a
the esthetic zone. Since the patient
and because the patient was clearly
crown that was not esthetic on tooth
desired an exact duplication of the
informed about all procedures prior
No. 7. Since the patient was an
crowding of her original anterior
to treatment initiation, no harm
optometrist and had direct and close
teeth, an FPD was considered to be
was caused to the patient. Healing
personal contact with the public, he
the best course of therapy.
discomfort and surgical involvement
did not want any long-term remov-
were within normal limits.
able prostheses; he also was opposed
to further tooth reduction unless it
was absolutely necessary.
The patient was presented with
Since the patient's home hygiene
Three treatment options were con-
all reasonable treatment options,
practices were questionable, the
sidered. The first option involved
including the option to do nothing
success of dental implant therapy
endodontic therapy, with a new
with her existing dentition. She
was uncertain. The potential need
crown for tooth No. 8 and a single-
was made aware of the anticipated
for future extraction might require a
tooth RPD. The second option
difficulty of fabricating a prosthesis
multi-tooth RPD; the design of such
involved performing endodontic
that would comply completely with
a prosthesis might be complicated
therapy on tooth No. 8 and conven-
her esthetic demands. The patient's
by endosseal implants in the sites of
tional FPD therapy from teeth No.
desire to recreate her existing maloc-
teeth No. 8 and 9. A plan for failure
8–10, replacing tooth No. 9 with a
clusion was honored.
was discussed with the patient, who
pontic. The third option involved
www.agd.org General Dentistry September/October 2008 543
Practice Management and Human Relations Ethical decision-making
Fig. 7. The patient in Figure 6, after receiving dental implants and an
Fig. 8. The patient in Figure 6, after splinted, implant-supported crowns
interim acrylic RPD. The existing crown on tooth No. 7 was made to
were fabricated to replace teeth No. 8 and 9. The crown on tooth No. 7
match the existing cantilever FPD.
was replaced to provide a more esthetic result.
extracting tooth No. 8 and utilizing
nothing with his existing dentition.
were within normal limits. An
implant therapy to replace teeth No.
He was made thoroughly aware of
interim RPD was fabricated during
8 and 9. The patient selected the
the difficulty of providing a prosthe-
the healing period so that the patient
third option; in addition, he wished
sis that complied with his esthetic
did not have to endure social stigma
to replace the crown on tooth No. 7
demands. The dentist exercised
due to missing central incisors.
with a more esthetic restoration.
professional autonomy by replacing
Once a treatment plan was
the restoration on the lateral incisor
selected, tooth No. 8 was extracted
at no fee because he was not satis-
Considerations for the patient's
and bovine bone was grafted for
fied with the result of his previous
profession and psychosocial success
ridge preservation. Two endosseous
solidified the selection of implant
dental implants were placed and
therapy over other treatment alter-
an interim acrylic RPD (with no
natives. This treatment choice cre-
contact over the implant sites) was
There was no absolute contraindica-
ated a situation that was more stable
fabricated for esthetic function
tion for FPD therapy but there
and predictable than his original
only (Fig. 7). Definitive implant-
were relative contraindications for
prosthesis. The dentist's decision
supported crowns were fabricated
an implant-retained or removable
to replace the restoration on tooth
to replace teeth No. 8 and 9 and the
prosthesis. The patient was given
No. 7 at no fee was made with the
crown on tooth No. 7 was replaced
the same options for treating his
patient's best interest in mind.
(Fig. 8). The restorability of tooth
condition as anyone else would have
No. 8 was questionable and tooth
received in a similar situation. He
Case report No. 4
No.10 was virgin. Because of the
also was clearly informed that his
On two different occasions (two
patient's profession and his desire
home compliance would determine
years apart), a 62-year-old woman
to avoid a removable prosthesis, a
the success of any treatment option.
sought treatment for maxillary
definitive RPD was contraindicated.
incisors that had fractured 2.0 mm
The crown on tooth No. 7 was
coronal to the free gingival margin.
replaced at no fee to the patient.
Since al procedures were performed
Tooth No. 7 was the first to fracture
according to accepted protocols
(Fig. 9); tooth No. 10 fractured two
Ethical considerations
and because the patient was clearly
years later (Fig. 10). An Angle's
informed about al procedures prior
Class I second premolar bilateral
The patient was presented with
to treatment initiation, no harm
occlusion had been restored previ-
all possible treatment options,
was caused to the patient. Healing
ously, with stable centric occlusion
including the option to do
discomfort and surgical involvement
and adequate anterior guidance.
544 September/October 2008 General Dentistry www.agd.org
therapy to replace tooth No. 20
without incident.
The first treatment option
involved endodontic therapy on
the involved lateral incisor, crown-
lengthening surgery, fabrication of
a post and core, and crown therapy.
The second option involved extrac-
tion of the fractured lateral incisor
and phased FPD therapy, utilizing
the lateral canine and central inci-
sor as abutments. The third option
involved extracting the fractured
Fig. 9. A radiograph and anterior view of a 62-year-old woman with a fracture just above the
lateral incisor and utilizing an
gingival margin on tooth No. 7.
RPD. The fourth option involved
extracting the incisor and utiliz-
ing implant replacement therapy,
replacing the lateral incisor with an
implant-supported crown.
Crown-lengthening therapy would
alter the gingival profile significantly
and expose the margins of the exist-
ing adjacent crowns. FPD therapy
was contraindicated at both visits
due to the cost already invested in
crown therapy on adjacent teeth.
Implant therapy appeared to be the
best treatment option.
Although the patient was given the
same four treatment options at both
Fig. 10. A radiograph of the patient in Figure
Fig. 11. A radiograph of the patient in Figure
visits, she made a different choice
9 taken two years later demonstrates a similar
9, after receiving a dental implant to replace
each time. At her first visit, the
fracture on tooth No. 10.
tooth No. 7 while the gingival architecture was
patient requested implant replace-
ment therapy because she had been
pleased with the results of previous
implant therapy. At the second visit,
the patient's situation had changed
and she was concerned about under-
The patient had a history of fibro-
Inc.), Oxycontin (Purdue Pharma,
going any additional surgery, leading
myalgia, osteoarthritis, hypothy-
Stamford, CT; 800.877.5666),
her to choose the first option.
roidism, sleep apnea, hypertension,
and aspirin with calcium. A his-
Tooth No. 7 (the first fractured
depression, anxiety, chronic sinus-
tory of excellent home care and
tooth) was extracted atraumatically
itis, and primary tension head-
compliance with dental therapy
and an endosseous implant was
aches. At the time of both visits,
was obvious upon the initial visit,
placed immediately at the time of
she was taking Prinivil (Merck &
but declining health and dexterity
extraction. The patient declined to
Co., Inc., Whitehouse Station, NJ;
became evident by the time of
receive a provisional restoration. An
800.444.2080), Zoloft (Pfizer, Inc.,
the next visit two years later. The
implant-supported crown was fabri-
New York, NY; 800.223.0182),
patient was pleased with her smile
cated (Fig. 11). When tooth No. 10
Xanax (Pfizer Inc.), Levoxyl (King
and did not wish to alter her gin-
fractured similarly two years later,
Pharmaceuticals, Bristol, TN;
gival profile; she had been treated
endodontic therapy was completed,
800.776.3637), Neurontin (Pfizer,
previously with dental implant
a prefabricated post and resin core
www.agd.org General Dentistry September/October 2008 545
Practice Management and Human Relations Ethical decision-making
Fig. 12. A radiograph of the patient in Figure 9, after conven-
Fig. 13. An anterior view of the patient in Figure 9, after receiving a conventional
tional therapy was completed to restore tooth No. 10. An ideal
crown supported by a prefabricated post and core on tooth No. 10. The gingival
ferrule was sacrificed to preserve biologic width.
architecture was maintained.
was placed (Fig. 12), and the tooth
treatment option. She declined
the best possible prognosis, based on
was restored using a porcelain-
crown-lengthening surgery with
the patient's prior experience with
fused-to-high noble metal crown
the thorough understanding that it
dental care and the fact that remov-
without osseous crown-lengthening
may be necessary in the future for
ing the adjacent crowns to fabricate
surgery. (The biologic width viola-
optimal gingival health.
an FPD would subject those teeth
tion was minimized to the greatest
to unnecessary trauma and lead to
extent possible.) The patient's
additional expense. By the time
esthetic and functional needs were
All reasonable treatment options
the patient sought treatment for
met appropriately with two different
were presented to the patient. Her
tooth No. 10, it was apparent that
approaches to care (Fig. 13).
medical history, desires, and capa-
elective surgical procedures should
bilities were considered carefully
be avoided due to medical risks.
Ethical considerations
and independently at the time of
Therefore, the patient's health at the
each presentation.
time of each event was factored into
In both scenarios, the patient was
the selection of a treatment modal-
presented with all possible treatment
ity for each situation.
options, including the option to do
Although the "ideal" protocol was
nothing with her existing dentition.
not followed in the restoration of
She was made aware of the difficulty
tooth No. 10, the patient was clearly
In each of these case reports, ethical
that would result from crown-
informed about al procedures prior
principles guided the plan of care.
lengthening therapy. At her first
to treatment initiation and no harm
Patient autonomy was the last step
visit, she was predisposed to dental
was caused to her. Healing discom-
in the ethical decision-making pro-
implant therapy because of suc-
fort and surgical involvement were
cess. The dentist used knowledge
cessful previous implant therapy; at
within normal limits. The patient's
and ability to answer the questions
that time, she declined a provisional
request for the course of therapy in
regarding why treatment was neces-
prosthesis to reduce the cost of ther-
both scenarios was reasonable.
sary, enabling the patient to make
apy. By the time of the second visit,
a sound autonomous decision. The
she was aware of the decline in her
principle of veracity was not noted
health and was willing to accept the
Initially, implant therapy appeared
for each case because it is a value of
risks of a somewhat compromised
to be the best treatment option with
the authors to tell the truth about
546 September/October 2008 General Dentistry www.agd.org
treatment options within the limits
tion of technological advances in
of the information that is available
dental medicine integrates the art
1. A mil ennium of dentistry—A look into the
and necessary to make a choice.
and science of dentistry, personal
past, present and future of dentistry. Available
Trust is considered an integral
values and beliefs, and a profes-
part of the dentist-patient relation-
sional code of ethics into a decision-
Accessed July 20, 2007.
ship and is essential for informed
making framework for providing
2. Healthy People 2010, vol. 2. Washington, DC:
Department of Health and Human Services;
appropriate care.
Even as technology advances
3. American Dental Association. Principles of eth-
rapidly and aggressive marketing
ics and code of professional conduct. Available
practices appear to be increasingly
The authors wish to thank the team
ada_code.pdf. Accessed June 2007.
necessary, clinicians cannot be con-
of technicians at BecDen Dental
4. Windholrn R, Cuenin M. An implant versus a
sidered incompetent simply because
Laboratory (Draper, Utah) for their
conventional fixed prosthesis: A case report.
Gen Dent 2007;55:44-47.
they make decisions that other cli-
artistic talents demonstrated in each
5. Sadowsky D. The moral dilemmas of the multi-
nicians may view as inappropriate,
case and the staff in the Department
ple prescription in dentistry. J Am Coll Dent
provided there is sound scientific
of Nursing at the University of
6. Ethics handbook for dentists. Gaithersburg,
rationale behind the choice of treat-
Akron for their assistance.
MD: American College of Dentists;2004.
ment rendered in good faith. Pro-
7. Weinstein B. Dental ethics. Philadelphia: Lea
viding treatment without informed
& Febiger;1993.
8. Huff KD, Leffler WG, Campbell D. Ethics are
consent devalues patient autonomy.
The authors have received no
moral, but morality is not ethics. Gen Dent
Because dentistry is an ethical
financial reward from any of the
profession, the ethical obligations
products, companies, or laboratories
9. Kelley J. Ethical dentistry: A time proven solu-
tion to a modern problem. J Am Coll Dent
of the dentist must guide every
mentioned in this article.
treatment decision. If neither the
10. Nichols P, Winslow G. What patients need ver-
patient nor the dentist are comfort-
sus what they want. Gen Dent 2003;51:503-
able with the decision, there is no
Dr. Kevin Huff is a clinical instruc-
11. Perel M. Endodontics or implants: Is it that
obligation for the dentist to treat
tor, Department of Comprehensive
simple? Implant Dent 2006;15:111.
the patient beyond stabilizing a life-
Care, Case School of Dental Medi-
Published with permission by the Academy of General
threatening urgent condition. A
cine in Cleveland, Ohio, where Dr.
Dentistry. Copyright 2008 by the Academy of
dentist should not perform a treat-
Farah is an associate clinical profes-
General Dentistry. All rights reserved.
ment that would violate another
sor. Dr. Marlene Huff is an associate
ethical principle simply to support
professor, Col ege of Nursing,
patient autonomy. Ethical utiliza-
University of Akron in Akron, OH.
www.agd.org General Dentistry September/October 2008 547
Source: http://www.doctorhuff.net/wp-content/uploads/2015/12/EthicalDecisionMakingforMultiplePrescriptionDentistry.pdf
UNIVERSITAS SCIENTIARUM Enero-junio de 2005 Revista de la Facultad de CienciasPONTIFICIA UNIVERSIDAD JAVERIANA Vol. 10, No. 1, 97-108 EFFECTIVENESS OF ELECTROLYZED OXIDIZING WATER Listeria monocytogenes IN LETTUCE Casadiego Laíd Paola1, Cuartas Vivian Rocío1, Mercado Marcela 1, Díaz Milciades2 y Carrascal Ana Karina1 1Laboratorio de Microbiología de Alimentos, Departamento de Microbiología
CATALOGO GENERALEGENERAL CATALOGUE made in Italy, made in F.A.R.G. Nei primi anni Sessanta ad Invorio, nella provincia di Novara, da sempre distretto di eccellenza nella produzione dell'industriadella rubinetteria, Giampiero Conton inizia la sua attività fondando la Rubinetteria Conton. Inizialmente l'azienda ebbe comescopo principale la commercializzazione di materiale idrosanitario; l'intuito del fondatore e alcuni segnali provenienti dallaclientela fecero capire le aperture del mercato e la possibilità di investire con ottimi risultati nella produzione di rubinetti agalleggiante con relative sfere in materiale plastico e in rame, senza dover fare i conti con una concorrenza troppo numerosa.E' nel 1996 che nasce F.A.R.G., naturale evoluzione di Rubinetteria Conton, che opera oggi su un'area di circa 15.000 mq dicui 5.000 mq coperti dedicati ai processi produttivi. Nel tempo la gamma dei prodotti si è ampliata con l'introduzione dialcuni componenti per impianti idrosanitari mantenendo la garanzia di qualità attestata da una produzione interamente ‘Made in Italy'. La costante attenzione della qualità, l'utilizzo di tecnologie avanzate e una rete di vendita che si avvale dellacollaborazione di agenti presenti sul territorio, hanno portato l'azienda a imporsi sul mercato nazionale e su quello estero.