Kamagra gibt es auch als Kautabletten, die sich schneller auflösen als normale Pillen. Manche Patienten empfinden das als angenehmer. Wer sich informieren will, findet Hinweise unter kamagra kautabletten.
A guide to the management of occupational asthma
Occupational Safety and Health Information Series
A GUIDE TO THE
This booklet was written by Dr Chris Walls with assistance from theOSH Departmental Medical Practitioners and Dr Julian Crane(Physician, Wellington), Dr Margaret Wilsher (Physician, Auckland)and Dr Colin Wong (Physician, Dunedin), members of the NODSAsthma Panel.
Dr John Allen (Pukekohe), Dr Charles Skinner (Auckland) and DrRob Stewart (Auckland) provided a critique from a general practiceview point and their assistance is greatly appreciated.
Published by:Occupational Safety and Health ServiceDepartment of LabourWellingtonNew Zealand
Issued February 1995
ISBN 0-477-03559-0
The History and Incidence of Occupational Asthma
What is Occupational Asthma?
Occupational and Clinical History
Clinical Findings
Interpretation of Peak Flow Recordings
Treatment of Occupational Asthma
Compliance with the Health and Safety in Employment Act 199218
Appendix 1: Materials Recognised as Causing OccupationalAsthma (adapted to New Zealand conditions)
Appendix 2: OSH Occupational Asthma Investigation Form 24
Appendix 3: Occupational Asthma Peak Flow Chart
Occupational Safety and Health Service Branches (February1995)
Departmental Medical Practitioners (February 1995)
4 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
The Occupational Safety and Health Service of the Department of Labour(OSH) is committed to providing health and safety information so thatmanagers and their employees are able to control the risks arising in theworkplace to their health and wellbeing.
In New Zealand 90 percent of businesses employ less than ten people. Thissize of enterprise is unable to afford an occupational health nurse or doctorand local general practitioners act as the default occupational health advisersfor this size of industry. General practitioners play a crucial role in thediagnosis and treatment of all occupational illnesses includinga s t h m a .
This booklet is the fourth of a series of publications by OSH,highlighting important occupational health problems. It is aimedat providing general practitioners and other primary health carepractitioners with diagnostic information and practical solutions tothe occupational health problems they face in their day-to-daypractice. It is not intended to act as a textbook but as a conciseand practical aid to the general practitioner in his or her everydaypractice.
Asthma is recognised as a major health problem in New Zealand.
What is unknown is the extent of occupational influences on theincidence of asthma amongst the New Zealand working popula-tion. Because of this lack of knowledge and because occupationalinfluences are often overlooked, occupational asthma has beenincluded in the OSH Notifiable Occupational Disease System(NODS).
I hope that this information complements the other clinical mate-rial available on diagnosing and treating asthma, makes the gen-eral practitioner's task easier and contributes towards preservingthe health of all those at work.
R HillGeneral Manager
A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA 5
■ The exact incidence of occupational asthma is unknown but probably
affects about 10 percent of adult asthmatics.
■ An occupational origin must be considered in any case of asthma arising
for the first time in an adult.
■ The majority of occupational asthmatics suffer considerable ongoing
clinical and financial problems because of their asthma — earlyrecognition and control is vital for them and their families.
■ The diagnosis can be inexact but relies on:
- a clinical history consistent with asthma,
- an exposure history to some potential causative agent,
- evidence of reversible airways obstruction associated with the
workplace exposure.
■ The best measure of the occupational origin of a patient's asthmatic
symptoms is obtained by peak flows.
A minimum of
four peak flow measurements a day for
two weeks isrecommended.
■ OSH expertise is available to help make the diagnosis by elucidating the
workplace factors and advising on control measures.
■ Recognition and control of the causative agent is the most important
step in controlling the patient's symptoms.
■ Treatment of symptoms is no different from other types of asthma but
will often be unsuccessful if the exposure is not identified and controlled.
■ In the experience of the panel, the four most common agents to date
causing occupational asthma in New Zealand are:
Isocyanate paints,
Car and furniture painters using
foams and plastics
two-pot paints, foam and plasticmanufacturers.
Animal fur and proteins
Laboratory workers, veterinaryworkers, etc.
Flour and grain dusts
Farmers, grain workers, bakers.
Epoxy resins and other
Boat builders, mould manufacturers,
plastic manufacturing processors.
6 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
The History and Incidence of Occupational Asthma
Asthma arising from occupational exposures has long been recog-nised. It is now clear that developing such an asthma can beserious medically andfinancially for the patient.
Occupational factors have long been recognised as causing asthma and inaggravating the symptoms of people with pre-existing asthma. In 1713Ramazzini, an Italian physician who interested himself in the occupationalcauses of illness, noted urticaria and shortness of breath in grain siftersexposed to organic dusts.1
In the 1920s Hunter2 first published his classical textbook
The Diseases ofOccupations and dealt with occupational asthma under the category of pneu-moconiosis (dust diseases of the lungs). He listed numerous individualoccupations where asthma-like conditions have arisen. With the industrialdevelopment that has occurred this century many of these occupations nolonger exist but have been superseded by other agents in new occupations.
Occupations well recognised as being at risk of causing asthma include spraypainting with isocyanate paints (two-pot paints used extensively by car paint-ers), carpenters working with Western red cedar and aluminiumsmelting (potroom asthma at Ti Wai Point Aluminium Smelter).
Both overseas and in New Zealand it is clear that developing anoccupational asthma has a profound impact on the wellbeing of that person.
Gannon and Burge3 in the UK and Garrett4 in NZ have shown that people inwhom the diagnosis of occupational asthma has been made suffer ongoingproblems. Some continue to be exposed and suffer continuing symptoms,others change jobs but suffer a financial loss (Gannon reports a median loss of54 percent of annual income), while other investigators have found thatstatutory financial compensation awarded to sufferers did not match their lossof income.
Up to 50 percent of people who have suffered from occupational asthma areleft with persisting asthma after removal from exposure and this may besevere and disabling5. Occasionally asthma attacks, precipitated by occupa-tional exposures, are fatal even though the preceding disease may have beenconsidered quite mild.
The frequency of occupational asthma is unknown in New Zealand. Overseasincident rates vary, but Tarlo6 estimates 5 percent of asthma being caused byoccupational factors while Gannon and Burge, reporting on the SHIELDscheme in the West Midlands region of the United Kingdom7, quote an inci-dence (the number of new cases in one year) of 43 per million employed. InNew Zealand terms this means that some 77 new asthmatics each year suffer atotally preventable illness attributable to their occupation.
The UK Guidance Note14 on occupational asthma quotes incidence figuresranging from 2 to 10 percent of all adult asthma as being occupational inorigin.
A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA 7
Why Has Occupational Asthma Been Included in the NODS System ?
What NODS is trying to achieve
NODS has been established for three principal reasons:
To obtain statistical information about the trends in occupationaldiseases in New Zealand. This allows OSH to fulfil its requirements toGovernment, professional agencies and the appropriate public healthagencies.
To act as a source of information for employers, employees and thoseprofessionals involved in providing occupational safety and healthinformation and health care — hence this series of guidelines.
To focus interventions back into workplaces so as to reduce theincidence of occupational disease in the future.
Notification to this system requires patient consent which ensurescompliance with medical ethics and the Privacy Act 1992.
For certain diseases, including occupational asthma, validation panels havebeen formed and these panels gather any further information required(workplace data, patient factors, etc.) to validate the diagnosis. If necessary,this can include an investigation of the workplace by OSH (which does notrequire the patient's identity to be revealed).
The diagnostic criteria for occupational asthma, like a number of diseases, arethe subject of debate and definitions differ from country to country and,indeed, amongst specialists within any one country.
As a consequence, the advisory panel for this booklet has made some arbitrarydecisions concerning diagnostic criteria, recommended methods of investigat-ing the illness and the possible range of specialist investigations. Thesedecisions will be reviewed as the panel gains experience with the casesreported to OSH, but are intended to aid statistical clarity.
What is Occupational Asthma?
A brief background to the complexities of occupational asthma
What seems a neat diagnostic category of occupational asthma becomesincreasingly blurred as experience is gained with the condition. The termcan be used to encompass pre-existing asthma exacerbated by the workenvironment, while other definitions refer only to asthma causally related toexposure in the work environment, i.e. "de novo" asthma.
Diagnostic definitions are often complicated by the parallel issue ofcompensation.
8 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
The mechanisms that underlie the development of occupational asthma arenot fully understood. Some definitions require sensitisation to be provenbefore the diagnosis can be accepted* while other definitions take a muchbroader approach.
There appear to be two causal pathways in the aetiology of occupationalasthma13.
A sensitising agent (either a high molecular weight agent by itself ora low molecular weight hapten conjugated with body proteins) cancause asthma.
Subsequent exposure may cause early bronchoconstrictive reactionsoccurring within minutes, or later reactions of longer duration. Theremay be a combination of dual early and late reactions.
However, the nature and timing of laboratory-induced responsesdescribed above do not necessarily reflect the pattern of asthmaarising from constant exposure at work.14
A heavy, sudden exposure to an irritating agent can give rise toasthma. The latter experience has been called "Reactive AirwaysDysfunction Syndrome" (RADS) and may be the mechanism for suchoccupational asthma as the "potroom asthma" experience inaluminium smelting.
The late asthmatic response or the after effects of a sudden heavy exposure toan irritating agent are associated with "bronchial hyper-responsiveness"where the airways react to a variety of stimuli such as cold, exercise, smokeand dusts as well as the original provoking agent. Many of these stimuli areencountered outside the workplace and this pattern of complaint can makethe diagnosis of occupational asthma very difficult.
The diagnosis of occupational asthma, like that of all occupational diseases, isbuilt upon the foundation of a good occupational and clinical history, aframework of knowledge of what the patient is exposed to and, to completethe metaphor, the roof of clinical findings.
Smith proposes six criteria for establishing the diagnosis of occupationalasthma8 and these criteria are useful to use as a check when considering thediagnosis.
Clinically demonstrable variable airways obstruction.
A known provoking agent is present in the workplace.
There must be exposure to this agent for a sufficient time.
* Industrial Injuries Advisory Council (UK) — Asthma that develops after a variable
period of symptomless exposure to a sensitising agent at work.
A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA 9
Tests of pulmonary function show airways obstruction after exposureto a specific agent. (This can be demonstrated by getting the patientto note their exposures on the peak flow chart as they challenge them-selves in the workplace by working with the suspected exposure.)
The asthmatic condition usually develops when inhaling lowconcentrations of the specific agent.
Symptomatic improvement occurs in many cases when the patient isaway from work, and symptoms are aggravated during the work day orworking week.
These criteria can be used as a guide when making the diagnosis ofoccupational asthma.
Occupational and Clinical History
Steps in making the diagnosis
A careful history is the most important tool to making a diagnosis of occupa-tional asthma. The main point of the history is to establish the temporal linkbetween the work and the asthma.9
The occupational history attempts to establish the likely agent and the lengthand degree of exposure.
The occupational history should record the work that the patient has donesince leaving school and the exposures that the patient had in these occupa-tions. The intention is to identify the causative agent and whether thesymptoms are totally new or an aggravation of longstanding problems.
Particular attention should be paid to what these exposures (e.g. dusts, chemi-cals) consisted of. For example, "lots of dust" needs some clarification asdusts may be inert as in soil dusts, contain wood and chemicals as in wooddust, biological material (animal protein and spores) as in dust from a poultryshed, or dried chemicals (powder coating plants or timber treatment plants).
Chemicals are often only known by their commercial names or are a mixtureof other chemicals. OSH occupational hygienists are available to offer adviceas to the potential of materials or products to cause asthma or to research theconstituent parts of a product. They may be contacted at the OSH branchoffices listed in this guide.
A useful tool when trying to assess a product is to obtain the Material SafetyData Sheet usually referred to as the MSDS. This can be obtained from themanufacturer of the chemical product free of charge or from the PoisonsCentre in Dunedin. The MSDS presents information concerning the product
10 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
in a standard way and is useful as a shorthand, quick reference when assessingthe risk to patients.
An occupational asthma investigation form used by the OSH occupationalhealth nurses is included in Appendix 2 for use if desired.
Note should be made of:
1. Latency Period
There should be a time lapse between the first exposure and the developmentof symptoms. This can vary according to the specific agent and the degree ofexposure. For example, a large spill of a substance or a fire involvingisocyanates can cause immediate symptoms.
However, it is usual for a longer period of exposure to occur before symptomsdevelop. (It should be remembered that a person may have been sensitised ina previous occupation and develop symptoms very quickly on beingrechallenged by the exposure in a new workplace.)
Commonly, occupational asthma begins within one or two months of initialexposure and will usually have occurred within one to two years of exposure.
Very uncommonly, the sensitising period can be a matter of days or weeks.5
2. Exposure History
Exposure means taking a guess at the dose of a substance the person received.
It is essentially a dose (or concentration of the substance) time calculationand takes into account the following:
■
How messy was the workplace ?
Sometimes you must rely on anecdotal estimates ("I couldn't seeacross the workshop because of the dust"). Occasionally environ-mental monitoring (i.e. dust concentration measurements) has beenperformed and can be used. (This sort of information may have beencollected by OSH or the employer.)
■
How many hours a week was the patient exposed ?
Try to rough out a time estimate for the exposure — so many hoursper week for so many years. This is essentially similar to thecalculation of pack years used for smokers.
■
What protection was in place and was it working ?
Protection can range from sophisticated exhaust booths with theirown ventilation through to the personal protection offered by arespirator.
It is important to assess how well this protection worked. In manyworkplaces there is no protection available, or the ventilation wasswitched off or inoperative because of faulty maintenance.
A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA 11
Personal protection (e.g. respiratory masks) is often ineffective because people find such protection uncomfortable and won't wear themand no effort is made by management to ensure the protection is used.
The key questions to ask your patient
The clinical history is vital to making the diagnosis and is composed of severalparts. Usually, it is the clinical history that enables the diagnosis of occupa-tional asthma to be made. There are four key screening questions to ask.
Although the actual pattern of asthma varies according to the substance andthe patient, these questions will help identify the majority of sufferers:
■
Does your asthma vary during the working week ?
Usually, occupational diseases including asthma worsen during theworking week so that by the end of the shift period there has been asteady deterioration in symptoms and clinical measurements.
Often questioning reveals certain days and tasks where symptoms aremore pronounced helping to identify the cause of the asthma.
■
Is your asthma better or worse on days away from work ?
Patients may note a continued improvement away from work,especially on long weekends or holidays. Identifying work/non-workperiods on peak flow charts gives a vital clue to occupational asthma.
■
Is your asthma better or worse on holidays ?
For those patients with severe asthma and who have a slow recovery,the two- or three-day break may not be sufficient to allow a return tothe non-asthmatic state. Patients often report a dramatic improve-ment of symptoms after several days away from the workplace and arelapse of symptoms within 48 hours of returning to work.
In complex cases it is necessary to differentiate between holidays athome or away from home because of the compounding effect ofirritants.
■
Is your sleep disturbed by cough or breathing problems ?
Occupational asthma often causes "night" cough or episodes ofwheezing or shortness of breath waking the patient from sleep. Thesesymptoms can be quite mild, are often initially misinterpretedbecause they do not occur at work (e.g. the shift worker will blame thelight and noise outside for waking him or her or attribute thesymptoms to a recurrent cold).
12 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
Burge12 notes that the prevalence of occupational asthma is higher in smokersand smoking enhances the production of specific IgE in an occupationalsetting. A variety of mechanisms have been postulated to explain this in-creased prevalence including an increase in exposure to an occupational agentby smoking in the at risk environment.
Smoking history is always relevant. Some employers or insurance companieswill attempt to blame smoking as the cause of the symptoms rather thanaccepting that work can be a causative agent. It will be impossible to controlan occupational asthma while your patient continues to smoke in theworkplace in the presence of the causative exposure. Without a smokinghistory you cannot properly advise the patient or their employer.
The Role of Atopy
Obtaining a history of atopy is important when considering whether anasthma is the result of becoming sensitised or when trying to assess whetherthe work situation has aggravated a pre-existing asthma. Positive skin pricktests to a variety of common allergens and an increased total serum IgE helpsupport the diagnosis of atopy.
Measurements used to make the diagnosis
The NODS Asthma Panel tries to obtain the following information whenassessing a case:
■ Clinical evidence of reversible airways obstruction (peak flow
variability, response to inhaled beta-agonist such as an increased peakflow or FEV ).
■ A peak flow pattern demonstrating a increased peak flow variability
associated with exposure. To measure this adequately the panelrecommends:
A minimum of four peak flows a day for two weeks.
The best of three (to ensure a consistent result) peak flows isrecorded. Before work, during work (mid shift), immediately afterwork and as the patient goes to bed are the suggested times. A peakflow chart is available in Appendix 2 and pads of this peak flow chartare available from the local OSH branch office.
The patient must mark the time at work and not at work and, ifpossible, periods when they were exposed to the suspected aetiologicalagent, presuming the exposure was not continuous. They should also
A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA 13
try and record symptoms such as cough, wheeze and shortness ofbreath on the chart.
Ideally, these peak flows should be performed over a week at the end ofthe patient's holidays and the beginning of their work period. Thepeak flow chart should always include time away from work, evenweekends or the long shift break.
■ Lung function tests (FEV and FEV /FVC) both before and after
administration of a bronchodilator.
To gain the maximum benefit these tests should be arranged for atime when the patient is in the middle of their working cycle and aftera medication-free period of at least 4 hours.
This might be the counsel of perfection for some general practitioners,but many practices now have spirometers and will have the ability tofollow this protocol.
■ In specialist centres the measurement of non-specific bronchial
responsiveness or irritability is a useful tool in assessing the patient.
This involves measurement of the provocative concentration ofhistamine or methacholine that causes a 20 percent fall in FEV . This
concentration is called the PC . A positive methacholine or histamine
challenge supports a clinical diagnosis of asthma when baselinepulmonary function is normal. A negative study result does not,however, rule out occupational asthma.10
In some industries serial measurements of bronchial responsivenessare used to:
(a) Monitor at risk employees;
(b) Assess suspected cases of occupational asthma;
(c) Assess response to treatment; and
(d) Monitor a person's wellbeing after re-introduction to the
Other specialised tests are available overseas. These include skin testing,radioallergosorbent testing (RAST assays) and specific inhalation challenges.
Skin testing with common allergens (house dust, grass and tree pollens) canbe useful in determining the atopic status of a patient. These tests do notpredict the reaction of the airways to these allergens. Atopy may point to anoccupational exacerbation of a pre-existing asthma.
In a few cases, appropriate extracts of potential occupational allergens areavailable for skin testing, but it must be remembered that both skin testingand serologic testing document exposure and sensitisation but may notnecessarily be associated with symptoms of asthma10. Such tests are notperformed routinely in New Zealand to the knowledge of the NODS panel andit is often not clear what the tests mean when they are performed.
14 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
Specific inhalation challenges are not performed in New Zealand. They havebeen described as the final arbiter of proof9 but they are exceedingly expensiveand are not without considerable risk to the patient. Furthermore, problemsarise in estimating the actual inhaled dose encountered in the workplace,often of a mixture of substances and, in evaluating the results of artificialdoses given, in an artificial environment.
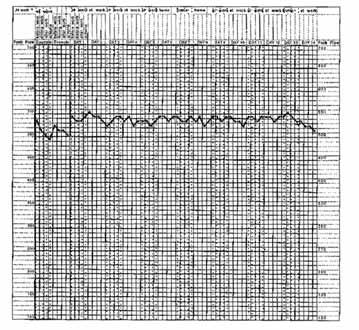
Interpretation of Peak Flow Recordings
The common patterns of peak flow recording in occupational asthma
The peak flows seek to establish the relationship between work and symp-toms. Once occupational asthma is occurring the symptoms usually worsenduring the working week and recover, to some extent, during the weekend orshift break.
Burge reports the following patterns of peak flow response9:
■ A normal record with a peak flow in the normal range (age and height)
with a diurnal variation of < 15 percent demonstrated by the followinggraph.
A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA 15
■ Patients with a reduced mean peak flow or an increased diurnal
variation that fail to show an improvement over weekends. Occupa-tional asthma may be missed because of the long period needed forsome people to recover and, in these cases, peak flows over a period oftwo weeks away from work may be necessary.
■ Patients showing clear evidence of occupational asthma where peak
flow records show an increased diurnal variation and deterioratingpeak flows when at work and improvement when away from work.
■ Patients who show a deterioration at work and improvement away
from work where the diurnal variation is less than 15 percent. Thissituation can occur where these is severe occupational asthma withlow peak flow values, or where there is an additional workplace irritanton top of unrelated chronic airflow obstruction.
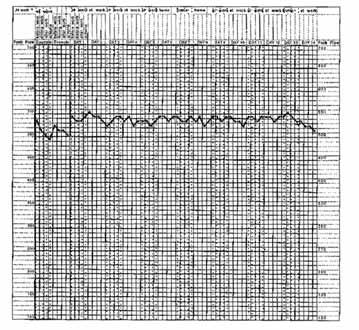
Discussion of these various patterns can be confusing and the following peakflow chart measured by a welder working in the ship repair industry is a goodexample of a positive peak flow chart. It shows an excessive diurnal variationwith a steady deterioration over the working period. Extra peak flows taken inthe middle of the night show dramatic falls in peak flow values. The peakflows at the beginning of the chart represent the only time the welder wasn'tworking and give a baseline of his non-exposed lung function.
16 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
A number of exposures are the possible culprit(s) and include the weldingfumes composed of oxides of nitrogen, sulphur dioxide, metal fumes from themetal, and the products of combustion from cutting isocyanate foaminsulation and ozone produced by the welding process.
This welder was using little in the way of personal protection and the weldingoften took place in a confined space where the oxygen content of the inhaledair could be reduced because of its consumption in the welding process.
A second peak flow chart is from an electronic worker referred by her generalpractitioner with persistent and poorly controlled asthma. This patient wasexposed to solder fumes containing colophony and her peak flow values showa steady deterioration during the working week and a recovery over theweekend.
This person's symptoms were controlled by the installation of some efficientlocal exhaust ventilation and remains well and in continued employment.
Getting the Information to Make the Diagnosis
When you suspect one of your patients has occupational asthma, but you areunsure of the possible causes or the condition of the workplace, OSH is ableto provide information or have its officers inspect the workplace if it iswarranted.
A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA 17
The Departmental Medical Practitioners, members of the OSH Asthma Paneland the local OSH office are listed at the back of this booklet and can becontacted for advice or assistance.
Treatment of Occupational Asthma
How can you help your patient?
The pharmacological treatment of occupational asthma is no different fromany other form of asthma. The only important difference between the treat-ment of occupational asthma compared with non-occupational asthma is thenecessity of identifying the causative exposure and controlling it.
Too often it seems that advice given to sufferers consists of telling the suffererto "wear a mask" or alternatively to "find another job". Neither of these twooptions are necessarily the best way of dealing with the problem.
There is evidence that the early recognition of occupational asthma andcontrol of the causative exposure lessens the severity of the condition.15
What advice you can give to control the problem?
The Health and Safety in Employment Act (1992) requires that employersidentify hazards and then control them by elimination, isolation andminimisation.
This hierarchy of control measures is a useful tool to use when advising yourpatients or their employers of the steps to consider.
In today's industrial climate substituting the hazard with another product ormaterial is often feasible. For example, the employer of the electronic worker,whose peak flows are represented above, was able to purchase a rivetingmachine which did away with the need to use solder in some of the circuit-board manufacturing processes. OSH occupational hygienists can advisedoctors if alternative products or processes are available.
By restricting the agent to some part of the factory or to specific times, it maybe possible to remove your patient from exposure to the asthma-causingagent and relieve their symptoms. It should be remembered that for thesensitised patient very small exposures will be sufficient to precipitatesymptoms.
18 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
The minimisation of the risk from the asthma-causing agent can be achievedby a number of measures. The first control measure to consider is adequateventilation (both local and environmental) and the last measure is personalprotection by means of respirators.
Ventilation is a complex solution and the employer is well advised to seeksome expert advice before purchasing equipment or approaching the problemon a piecemeal basis.
Personal protection (a respirator) is not a cheap option. To be used success-fully, the respirator must be appropriate for the agent or mixture in question,be individually fitted, maintained correctly and, most importantly, wornwhenever the person is exposed to the agent or mixture. It should only beused in conjunction with other measures and where substitution of theoffending agent is not practicable.
Most people find wearing a respirator a nuisance and compliance with rules towear a respirator is often poor because of a number of factors. Such protec-tion may be suitable where the exposures are not heavy and are for only asmall portion of the working shift.
Respiratory protection is a subject in its own right and rather than cover itinadequately in this booklet a copy of A Guide to Respirators and BreathingApparatus may be obtained from any OSH branch office.
Only as a last resort, and after consultation with a respiratory or occupationalmedical specialist, should someone be advised to abandon their occupation.
The decision is obviously of great importance to the individual and has impli-cations for compensation issues as well as the more obvious treatment issues.
Compliance with the Health and Safety in Employment Act 1992
Occupational asthma is defined in the Health and Safety in Employment Actas "serious harm". As such there is a duty on the employer to inform OSH "assoon as is possible" when an employee is diagnosed as suffering occupationalasthma. The obligation is not on the doctor, although the doctor is able toinform OSH via the NODS scheme if the patient consents.
A doctor would have fulfilled any obligation under law by giving the patient aletter to hand to their employer stating that the patient was suffering fromoccupational asthma.
Occupational asthma is relatively uncommon, but when it does occur it has aprofound impact on the individual's wellbeing. It should be considered in anyadult who is suffering asthma for the first time in their lives.
A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA 19
Many other asthma sufferers have their condition made worse by workplacefactors, and the suggestions about control measures apply to them as well asthe "pure" occupational asthmas.
The most important difference in the treatment of occupational asthma is totry and identify the causative exposure and control the patient's exposureto it.
As with most medical problems, this requires a team approach in which theOSH health and technical services are able to play a part in protecting yourpatients.
If you have any comments about this booklet, or suggestions for futureinformation booklets, please write to:
OSH Health ServicesOccupational Safety and Health ServiceDepartment of LabourPO Box 3705Wellington
Ramazzini B: De Morbus Artificum Diatriba (Wright WC, Trans Diseaseof Workers). Chicago: University of Chicago Press, 1940.
Hunter D: The Diseases of Occupations (6th Ed) Hodder and Stoughton,1978. ISBN 0-340-22084-8.
Gannon PF, Weir DC, Robertson AS, Burge PS: Health Employmentand Financial Outcomes in Workers with Occupational Asthma, Br J IndMed, 1993 50 (6) 491-6.
Garrett JE: Asthma and Employment Experience, N Z Med J, Aug 221990, 103 (896) 399-401.
Stenton S, Hendrick D: Occupational Asthma. Postgrad Med J (1991) 67,271-277.
Tarlo S, Broder I: Outcome of Assessments for Occupational Asthma,Chest, 1991, 100, 329-335.
Gannon P, Burge PS: The SHIELD scheme in the West Midlands Region,United Kingdom. Br J Ind Med, 1993, 50 791-796.
Smith D: Medico-Legal Definition of Occupational Asthma, Chest, 1990,98 1007-11.
Burge PS: Diagnosis of Occupational Asthma, Clinical and ExperimentalAllergy, 1989, 19 649-52.
20 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
10. Alberts W, Brooks S: Advances in Occupational Asthma, Clinics in Chest
Medicine, 13 (2) June, 1992, 281-303.
11. Chan-Yeung M, Lam S: Occupational Asthma, Am Rev Respir Dis 1986;
133: 686-703.
12. Burge PS: New Developments in Occupational Asthma, British Medical
Bulletin, (1991), Vol 48, No. 1, 221-230.
13. Venables K: Preventing Occupational Asthma (Editorial), Br J Ind Med
1992; 49: 817-19.
14. Medical Aspects of Occupational Asthma, Guidance Note MS25 from the
Health and Safety Executive, December 1991.
15. Chan Yeung M: Occupational Asthma, Chest, 1990: 98 5 (Supplement)
A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA 21
Appendix 1: Materials Recognised as Causing Occupational
Asthma (adapted to New Zealand conditions)
High Molecular Weight Compounds
Industry and At Risk Occupations
Animal products, insects, other
Laboratory workers
laboratory animals
Research laboratory
Laboratory workers
Fish bait breederEntomologists
BuckwheatCoffee beans
Detergent industry
Plastic, pharmaceutical
Manufacturing, bakers
Gum manufacturing
22 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
Low Molecular Weight Compounds
Industry and At Risk Occupations
Toluene diisocyanate (TDI)
Polyurethane foam industry, plastics, varnish
Diphenyl methane diisocyanate (MDI)
Foundries, plastics
Hexamethylene diisocyanate (HDI)
Automobile spray painting
Phthalic anhydride
Eposy resins, plastics (boat building)
Trimellitic anhydrideTetrachlorophthalic anhydrideMaleic anhydride
Western red cedar
Carpentry, construction, cabinet making,
California redwood
Cedar of LebanonCocoboilaIrokoOakMahoganyAbiruanaAfrican mapleTanganyika aningreCentral African walnutKejaatAfrican zebra woodNZ rimuParticle board (formaldehyde)
Platinum refining, jewellery manufacture,photography
Metal plating, stainless steel welding
Hard metal industries (steel making,
Cobalt, vanadium, tungsten carbide
tool hardening, etc)
Aminoethyl ethanolamine
Aluminium soldering
Electronic industries, welding
Phenylglycine acid chloride
Poultry feed mixer
Sulphone chloramides
Manufacturer, brewer
A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA 23
Low Molecular Weight Compounds (Continued)
Industry and At Risk Occupations
Dimethyl ethanolamine
Persulphate salts and henna
Plastics and rubber
Photocopying and dyes
Urea formaldehyde
Insulation, resins, particle boards
Health care workers, radiographic processors
Paraphenylene diamine
Furtfuryl alcohol (furan bases resin)
Foundry mould making
Aliphatic polyamines
Hardeners, particle board
Diethylene triamineTriethylene tetramine
24 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
Appendix 2: OSH Occupational Asthma Investigation Form
Questions 1-41 of this form should be completed by
8. Name and address of family doctor?
the Occupational Health Nurse while interviewing theperson notified as a possible case. Questions 42-53may be completed later.
Please return this form to the Regional DepartmentalMedical Practitioner when complete.
Personal details of person investigated
9. Have you ever smoked for as long as a year?
Go to question 11
Go to question 10
Go to question 10
10. At what age did you begin smoking?
On average how many cigarettes did you/do you
4. Telephone numbers:
If you no longer smoke how old were you when
you stopped smoking?
Occupational History
5. Date of birth:
11. Current employment status?
Go to question 12
Go to question 14
Go to question 14
On a sickness benefit
Go to question 14
7. Ethnic origin?
13. Current employer's name and address:
If other please specify below:
A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA 25
14. Please list your past employers and the number of years worked for each employer (use additional paper if needed).
Job title and employer
from 19. Please describe the nature of the work performed in this jobto 19.
19. Does the wheezing or tightness in your chest
15. Have you had wheezing or whistling in your
improve when you are away from work such as
chest in the last twelve months?
holidays or weekends?
16. In the last 12 months have you been breathless
20. Have you woken up with a feeling of tightness in
when the wheezing was present?
your chest at any time in the last twelve months?
17. Have you had this wheezing or whistling when
21. Do you have a persistent cough?
you did not have a cold?
No Go to question 23
Yes Go to question 22
18. Have you had wheezing or tightness in your
chest during or straight after work?
22. Do you tend to cough up phlegm on most days?
No Go to question 20
Yes Go to question 19
23. Do you get short of breath walking on the flat?
26 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
24. Do you get short of breath walking up a slight
33. Are you currently taking any medicines for
asthma (e.g. inhalers, aerosols or pills)?
No Go to question 34
Yes Please specify below
25. Do you get short of breath more than other
people of the same age?
26. Do you notice that the wheeze or cough gets
worse during the working week?
34. Have you been seen by a respiratory specialist?
27. Do you get short of breath when you are away
from work on a holiday or a long break?
If yes, please enter the name of the specialist below.
28. Do you wake up at night short of breath?
35. Have you been seen admitted to a hospital because of asthma?
29. Do you wake up at night because of persistent
If yes, please enter the name of the hospital below.
30. Do you know what makes you wheeze?
No Go to question 33
Yes Go to question 31
31. If you answered "yes" to Question 30, what are
36. Did you get asthma when you were a child
all the things that make you wheeze? (Mark the
appropriate boxes)
37. Have you ever suffered from eczema?
38. Have you ever suffered from hayfever?
Chemicals such as solvent or isocyanate
Go to question 32
39. Do you have a family history of asthma?
Go to question 32
32. If you answered yes to "chemicals" or "other"
please specify.
40. Do you have a family history of eczema?
41. Do you have a family history of hayfever?
A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA 27
42. Please complete the following table indicating:
substances used in the workplace that could be
implicated in this patient's problems; length of
exposure; intensity of exposure. Use extra paper
if necessary.
In order to assess whether this person's exposure
Attach the peak flow diary to this form. Peak flow
was heavy or moderate, take into account factors
forms must record time away from work and time
such as the percentage of the day that the person
since last dose of bronchodilator was taken by the
was exposed and whether any protection was
patient. (Peak flow forms are compulsory for this
used by the person.
Exposure estimate
(e.g. in your opinion was
48. When was the last dose of brochodilator taken by
this person's exposure
heavy, moderate or light)
Details of investigating nurse
49. Investigated by
50. Branch office
Workplace environmental monitoring
51. Date investigation commenced
43. Has environmental monitoring for the suspected
workplace substances been carried out?
52. Date investigation concluded
53. Which of the following actions were initiated as a
If yes, please attach results.
result of this notification?
44. Does environmental monitoring need to be
Discussion with management re safety
Workplace health and safety assessment
Investigatory biological tests
45. What environmental monitoring have you and/
or the occupational hygienist done? Tests
ordered (attach a copy of the results to this
Recommendation for consultation with
private sector health and safety providers
Investigation of other workers
46. Is there a problem in the place of work?
Workplace improvements recommended
Workplace improvements raised
Enforcement action required
Biological monitoring
Environmental monitoring
47. Patient clinical data
Please use additional paper if you would like to
make any comments (e.g. justification for yourexposure estimate), and return with this form toyour regional DMP.
28 A GUIDE TO THE MANAGEMENT OF OCCUPATIONAL ASTHMA
Appendix 3: Occupational Asthma Peak Flow Chart
Peak Flow
Peak Flow
Source: http://www.eat.worksafe.govt.nz/worksafe/information-guidance/all-guidance-items/asthma-a-guide-to-the-management-of-cccupational/asthma.pdf
M&A: Using Uncertainty to Your AdvantageA Survey of European Companies' Merger and Acquisition Plans for 2012 André Kronimus, Peter Nowotnik, Alexander Roos, and Sebastian Stange This report was prepared by The Boston Consulting Group on the basis of a survey of corporate executives in Europe conducted jointly with UBS Investment Bank.December 2011
TEMPLE UNIVERSITY Office of the Vice Provost for Research Division of Research Compliance Institutional Biosafety Committee Standard Operating Procedure (SOP) - Tamoxifen Principal Investigator: _ Room & Building #: _ Department: Phone # Date: _ Location(s) Covered by this SOP. Building Lab # Fume hood area Animal procedure Animal Holding