Kamagra gibt es auch als Kautabletten, die sich schneller auflösen als normale Pillen. Manche Patienten empfinden das als angenehmer. Wer sich informieren will, findet Hinweise unter kamagra kautabletten.
Acknowledgements
Basic Facts About
12th edition 2004
British Columbia Schizophrenia Society
"We'd like to change your mind"
A LETTER TO YOUNG PEOPLE,
EDUCATORS, PARENTS, AND OTHERS
If you want to learn some basic facts about schizophrenia, we hope you will find this booklet useful. Please remember, the text is meant only as an introduction it should not be used as a diagnostic tool.
Most of the information in the booklet comes from other books, articles, and people's personal experience. If you need to know more about schizophrenia, you should talk to your doctor or to a mental health professional.
Please note: You are welcome to reproduce this information in quantity, provided it is required for bona fide educational purposes.
We would like to hear your comments about how useful you found this booklet —or any ideas you might have for future improvements. You can contact us at:
British Columbia Schizophrenia Society
201-6011 Westminster Hwy, Richmond, BC V7C 4V4
(604) 270-7841 or 1-888-888-0029
[email protected]
http://www.bcss.org
British Columbia Schizophrenia Society
ii
TABLE OF CONTENTS
Schizophrenia: Get the Facts . 1 What Causes Schizophrenia? . 2 Symptoms . 4 Early Warning Signs . 6 Ageing Parents, Future Plans. 7 What is it Like to Have Schizophrenia? . 8 How Schizophrenia Affects Families . 10 The "Blame and Shame" Syndrome. 12 How Families Can Help .……13 Finding Good Treatment. 18 Promising Developments . 21 Medication Update . 22 Recovery. 24 FAQ's:
Frequently Asked Questions . 25
"I'm a TeacherWhat Can I Do?". 28 Myths and Misconceptions . 30 Benefits of Research . 32 Cost and Prevalence of Schizophrenia . 33 BC Schizophrenia Society:
Branches. 34 Regional Coordinators. 35 Family Support Outside B.C. 36 Resource Materials, Suggested Reading . 37 Glossary: The Language of Mental Illness . 38 The BC Mental Health Act . 41
Early Psychosis Education Resources
Description . 42 Order Form . 43
British Columbia Schizophrenia Society
iii
British Columbia Schizophrenia Society
iv
SCHIZOPHRENIA: GET THE FACTS
• Schizophrenia is a disease that strikes young people in their prime • The disease impairs cognition and distorts the senses, making it
difficult for the individual to tell what is real from what is not real
• Usual age of onset is between 16 and 25
• Schizophrenia is a medical illness.
Period • Treatment works!
•
Early diagnosis and stabilization on modern treatment can
greatly improve prognosis for the illness.
SCHIZOPHRENIA IS NOT RARE: NO ONE IS IMMUNE
• Schizophrenia is found all over the world—in all races, in all cultures
and in all social classes
• It affects
1 in 100 people worldwide. That's approximately 40,000 of
our BC neighbours or 290,000 fellow Canadians
MEN AND WOMEN ARE AFFECTED WITH EQUAL FREQUENCY
• For men, the age of onset for schizophrenia is often ages 16 to 20 • For women, the age of onset is sometimes later—ages 20 to 30
WE ARE ALL AFFECTED
• More hospital beds in Canada (8%) are occupied by people with
schizophrenia than by sufferers of any other medical condition
• The cost to Canadian society due to hospitalization, disability
payments, welfare payments, and lost wages ranks in the billions of dollars annually
• Other costs—such as loss of individual potential, personal anguish,
and family hardships—are impossible to measure.
British Columbia Schizophrenia Society
1
WHAT CAUSES SCHIZOPHRENIA?
"We do not yet understand precisely the cause of schizophrenia, but research is progressing rapidly."
— Seeman, Littmann, et al.
Researchers now agree thatwhile we do not yet know what "causes"
schizophreniamany pieces of the puzzle are becoming clearer. Areas of
study and interest are:
• BIOCHEMISTRY People with schizophrenia appear to have a
neurochemical imbalance. Thus, some researchers study the neuro-
transmitters that allow communication between brain cells. Modern
antipsychotic medications now primarily target three different neurotransmitter
systems (
dopamine,
serotonin, and
norepinephrine.)
• CEREBRAL BLOOD FLOW With modern brain imaging techniques (PET
scans), researchers can identify areas that are activated when the brain is
engaged in processing information. People with schizophrenia appear to have
difficulty "coordinating" activity between different areas of the brain. For
example, when thinking or speaking, most people show increased activity in
their frontal lobes, and a
lessening of activity in the area of the brain used for
listening. People with schizophrenia show the same increase in frontal lobe
activity—but there is
no decrease of activity ("dampening" or "filtering") in the
other area. Researchers have also been able to identify specific areas of
unusual activity during hallucinations.
• MOLECULAR BIOLOGY People with schizophrenia have an irregular pattern
of certain brain cells. Since these cells are formed long before a baby is born,
there is speculation that:
1. This irregular pattern may point towards a possible "cause" of
schizophrenia in the prenatal period; or
2. The pattern indicates a predisposition to acquire the disease at a
• GENETIC PREDISPOSITION Genetic research continues, but has not yet positively identified a hereditary gene for schizophrenia. Schizophrenia
does appear more regularly in some families. Then again, many people with schizophrenia have no family history of the illness.
British Columbia Schizophrenia Society
2
• STRESS Stress does not
cause schizophrenia. However, it has been
proven that
stress makes symptoms worse when the illness is already
present.
• DRUG ABUSE Drugs (including alcohol, tobacco, and street drugs)
themselves do not cause schizophrenia. However, certain drugs can make
symptoms worse or trigger a psychotic episode if a person already has
schizophrenia. Drugs can also create schizophrenia-like symptoms in
otherwise healthy individuals.
• NUTRITIONAL THEORIES While proper nutrition is essential for the well-
being of a person with the illness, it is not likely that a lack of certain vitamins
causes schizophrenia. Claims that promote megavitamin therapy have not
been substantiated.
Some people do improve while taking vitamins. However, this can be due to
concurrent use of antipsychotic medication, or to the overall therapeutic effect
of a good diet, vitamin and medication regime. Or—these individuals may be
part of that group who will recover no matter what treatment is used.
So — while we don't know the actual cause of schizophrenia, we do
SCHIZOPHRENIA IS:
• A brain disease, with concrete and specific symptoms due to
physical and biochemical changes in the brain
• An illness that strikes young people in their prime—age of onset
is usually between 16 and 25
• Almost always treatable with medication
• More common than most people think. It affects 1 in 100 people
worldwide—that's about 290,000 Canadians, including over 40,000 of our BC neighbours.
SCHIZOPHRENIA IS
NOT:
• A "split personality"
• Caused by childhood trauma, bad parenting, or poverty
• The result of any action or personal failure by the individual.
British Columbia Schizophrenia Society
3
"I just couldn't accept the fact that he had an above average I.Q., was good looking, had a good personality—and was so ill."
— Parent of a child with schizophrenia
Just as other diseases have signs or symptoms, so does schizophrenia. Symptoms are not identical for everyone. Some people may have only one episode of schizophrenia in their lifetime. Others may have recurring episodes, but lead relatively normal lives in between. Others may have severe symptoms for a lifetime. Schizophrenia
always involves a change in ability and personality. Family members and friends notice that the person is "not the same." Because they are experiencing perceptual difficulties—trouble knowing what is real from what is not real—the person who is ill often begins to withdraw as their symptoms become more pronounced. Deterioration is usually observed in:
• Work or academic activities • Relationships with others • Personal care and hygiene
CHARACTERISTIC CHANGES
• PERSONALITY CHANGE is often a key to recognizing schizophrenia. At first,
changes may be subtle, minor and go unnoticed. Eventually, such changes become obvious to family, friends, classmates or co-workers. There is a loss or lack of emotion, interest and motivation. A normally outgoing person may become withdrawn, quiet, or moody. Emotions may be inappropriate—the person may laugh in a sad situation, or cry over a joke—or may be unable to show any emotion at all.
• THOUGHT DISORDER is the most profound change, since it prevents clear
thinking and rational response. Thoughts may be slow to form, or come extra fast, or not at all. The person may jump from topic to topic, seem confused, or have difficulty making simple decisions. Thinking may be coloured by delusions—false beliefs that have no logical basis. Some people also feel they are being persecuted—convinced they are being spied on or plotted against. They may have grandiose delusions or think they are all-powerful, capable of anything, and invulnerable to danger. They may also have a strong religious drive, or believe they have a personal mission to right the wrongs of the world.
British Columbia Schizophrenia Society
4
• PERCEPTUAL CHANGES turn the world of the ill person topsy-turvy. Sensory
messages to the brain from the eyes, ears, nose, skin, and taste buds become confused—and the person may actually hear, see, smell or feel sensations that are not real. These are called
hallucinations.
People with schizophrenia will often hear voices. Sometimes the voices are threatening or condemning; they may also give direct orders such as, "kill yourself".
There is always a danger that such commands will be obeyed.
People who are ill may also have visual hallucinations—a door in a wall where no door exists; a lion, a tiger, or a long-dead relative may suddenly appear. Colours, shapes, and faces may change before the person's eyes.
There may also be hypersensitivity to sounds, tastes, and smells. A ringing telephone might seem as loud as a fire alarm bell, or a loved one's voice as threatening as a barking dog. Sense of touch may also be distorted. Someone may literally "feel" their skin is crawling—or conversely, they may feel nothing, not even pain from a real injury.
• SENSE OF SELF: When one or all five senses are affected, the person may
feel out of time, out of space—free floating and
bodiless—and non-existent as a person.
Someone who is experiencing such profound and frightening
changes will often try to keep them a secret.
There is often a strong need to deny what is happening, and to avoid other people and situations where the fact that one is "different" might be discovered. Intense misperceptions of reality trigger feelings of dread, panic, fear, and anxiety—natural reactions to such terrifying experiences.
Psychological distress is intense, but most of it remains hidden—so there may be strong denial, born out of fear. The pain of schizophrenia is further accentuated by the person's awareness of the worry and suffering they may be causing their family and friends.
People with schizophrenia need understanding, patience, and
reassurance that they will not be abandoned.
British Columbia Schizophrenia Society
5
EARLY WARNING SIGNS
The following list of warning signs was developed by people whose family members have schizophrenia. Many behaviours described are within the range of normal responses to situations. Yet families sense—even when symptoms are mild—that behaviour is "
unusual"; that the person is "
not the same". The number and severity of these symptoms differ from person to person—although almost everyone mentions
noticeable social withdrawal. • Deterioration of personal hygiene
• Losing possessions
• Extreme reactions to criticism
• Bizarre behaviour
• Inability to express joy
• Irrational statements
• Inability to cry, or excessive
• Sleeping excessively
or inability
• Inappropriate laughter
• Social withdrawal, isolation, and
• Unusual sensitivity to stimuli
(noise, light, colours, textures)
• Shift in basic personality
• Attempts to escape through
• Unexpected hostility
frequent moves or hitchhiking
• Deterioration of social
• Drug or alcohol abuse
• Hyperactivity or inactivity—or
alternating between the two
• Strange posturing
• Inability to concentrate or to cope
• Refusal to touch persons or
with minor problems
objects; wearing gloves, etc.
• Extreme preoccupation with
• Shaving head or body hair
religion or with the occult
• Cutting oneself; threats of self-
• Excessive writing without
• Staring without blinking—or
• Indifference
blinking incessantly
• Dropping out of activities—or out
• Flat, reptile-like gaze
of life in general
• Rigid stubbornness
• Decline in academic or athletic
• Peculiar use of words or odd
language structures
• Forgetting things
• Sensitivity and irritability when
touched by others.
British Columbia Schizophrenia Society
6
AGEING PARENTS FUTURE PLANS
Encouraging an adult child to live away from home is a loving
positive act, not a rejection. For someone with schizophrenia, this
can be the first step towards independent living…
Living apart can also mean that the quality of family time spent together is
actually better—resulting in less stress for everyone. No one can be on duty
24 hours a day (doing what three hospital shifts do) and also be emotionally
involved, without suffering physical and psychological damage.
Remember that schizophrenia does NOT interfere with a person's
intelligence. If parents continue to "give their all" and ultimately burn out, they
are of little use to
anyone. In addition, the person who is ill ends up unfairly
carrying a terrible burden of guilt for such sacrifices.
• Families must meet their own needs
now for the benefit of the ill person
in the long run. It is beneficial for
all family members to develop their own outside social life—even it if is not large.
• It's always hard to "let go", but to do so GRADUALLY can be the
beginning of a positive move towards adult independence.
• Moving away from home is ultimately necessary for all human beings.
No matter how loving and capable, parents will become less and less able to provide support as they grow older—and no one lives forever. Thus, it is usually best to establish independent living arrangements at a reasonable age.
• It's a good idea for someone who is ill to try living away from home on
an experimental basis at first. If it doesn't work out, they can return home for a shorter period of time, and then try again. Everyone should be clear that this is a just a beginning. That way, if things don't happen to work out immediately—no one feels the whole exercise was a failure.
British Columbia Schizophrenia Society
7
WHAT IS IT LIKE TO HAVE SCHIZOPHRENIA?
Despite her illness, Janice Jordan has successfully worked as a technical editor for over 20 years and has written a book of poetry based on her experience. "The schizophrenic experience can be a terrifying journey through a world of madness no one can understand, particularly the person travelling through it. It is a journey through a world that is deranged, empty, and devoid of anchors to reality. You feel very much alone. You find it easier to withdraw than cope with a reality that is incongruent with your fantasy world. You feel tormented by distorted perceptions. You cannot distinguish what is real from what is unreal. Schizophrenia affects all aspects of your life. Your thoughts race and you feel fragmented and so very alone with your "craziness." "I have suffered from schizophrenia for over 25 years. In fact, I can't think of a time when I wasn't plagued with hallucinations, delusions, and paranoia. At times, I feel like the operator in my brain just doesn't get the message to the right people. It can be very confusing to have to deal with different people in my head. When I become fragmented in my thinking, I start to have my worst problems. I have been hospitalized because of this illness many times, sometimes for as long as 2 to 4 months. I guess the moment I started recovering was when I asked for help in coping with the schizophrenia. For so long, I refused to accept that I had a serious mental illness. During my adolescence, I thought I was just strange. I was afraid all the time. I had my own fantasy world and spent many days lost in it. I had one particular friend. I called him the "Controller." He was my secret friend. He took on all of my bad feelings. He was the sum total of my negative feelings and my paranoia. I could see him and hear him, but no one else could. The problems were compounded when I went off to college. Suddenly, the Controller started demanding all my time and energy. He would punish me if I did something he didn't like. He spent a lot of time yelling at me and making me feel wicked. I didn't know how to stop him from screaming at me and ruling my existence. It got to the point where I couldn't decipher reality from what the Controller was screaming. So I withdrew from society and reality. I couldn't tell anyone what was happening because I was so afraid of being labelled as "crazy." I didn't understand what was going on in my head. I really thought that other "normal" people had Controllers too. While the Controller was his most evident, I was desperately trying to earn my degree. The Controller was preventing me from coping with everyday events. I tried to hide this illness from everyone, particularly my family. How could I tell my family that I had this person inside my head, telling me what to do, think, and say?
British Columbia Schizophrenia Society
8
It was becoming more and more difficult to attend classes and understand the subject matter. I spent most of my time listening to the Controller and his demands. I really don't know how I made it through college.
Since my degree was in education, I got a job teaching third grade. That lasted about 3 months, and then I ended up in a psychiatric hospital for 4 months. I just wasn't functioning in the outside world. I was very delusional and paranoid, and I spent much of my time engrossed with my fantasy world and the Controller.
My first therapist tried to get me to open up, but.I didn't trust her and couldn't tell her about the Controller. I was still so afraid of being labelled "crazy." I really thought that I had done something evil in my life and that was why I had this craziness in my head. I was deathly afraid that I would end up like my three uncles, all of whom had committed suicide.
I didn't trust anyone. I thought perhaps I had a special calling in life, something beyond normal. Even though the Controller spent most of the time yelling his demands, I think I felt blessed in some strange way. I felt "above normal." I think I had the most difficulty accepting that the Controller was only in my world and not in everyone else's world. I honestly thought everyone could see and hear him.I thought the world could read my mind and everything I imagined was being broadcast to the entire world. I walked around paralysed with fear.
My psychosis was present at all times. At one point, I would look at my co-workers and their faces would become distorted. Their teeth looked like fangs ready to devour me. Most of the time I couldn't trust myself to look at anyone for fear of being swallowed. I had no respite from the illness. I knew something was wrong, and I blamed myself. None of my siblings have this illness, so I believed I was the wicked one.
I felt like I was running around in circles, not going anywhere but down into the abyss of "craziness." Why had I been plagued with this illness? Why would God do this to me? Everyone around me was looking to blame someone or something. I blamed myself. I was sure it was my fault because I just knew I was wicked. I could see no other possibilities.
I do know that I could not have made it as far as I have today without the love and support of my family, my therapists, and my friends. It was their faith in my ability to overcome this potentially devastating illness that carried me through this journey.
…So many wonderful medications are now available to help alleviate the symptoms of mental illness. It is up to us, people with schizophrenia, to be patient and to be trusting. We must believe that tomorrow is another day, perhaps one day closer to fully understanding schizophrenia, to knowing its cause, and to finding a cure."
Adrift In An Anchorless Reality
Schizophrenia Bulletin, Volume 21, No. 3, 1995
British Columbia Schizophrenia Society
9
HOW SCHIZOPHRENIA AFFECTS FAMILIES
"The typical family of a mentally ill person is often in chaos. Parents look frantically for answers that often can't be found; siblings flee. Hope turns to despair, and some families are destroyed no matter how hard they try to survive."
— Parents of a teen with schizophrenia
When parents learn their child has schizophrenia, they experience a range of strong emotions. They are usually shocked, sad, angry, confused, and dismayed. Some have described their reactions as follows: • Sorrow ("
We feel like we've lost our child".) • Anxiety ("
We're afraid to leave him alone or hurt his feelings.") • Fear ("
Will the ill person harm himself or others?") • Shame and guilt ("
Are we to blame? What will people think?") • Feelings of isolation ("
No one can understand.") • Bitterness ("
Why did this happen to us?") • Ambivalence toward the afflicted person ("
We love him very much, but when
his illness causes him to be cruel, we also wish he'd go away.")
• Anger and jealousy ("
Siblings resent the attention given to the ill family
member.")
• Depression ("
We can't even talk without crying.") • Total denial of the illness ("
This can't happen in our family.") • Denial of the
severity of the illness ("
This is only a phase that will pass".) • Blaming each other ("
If you had been a better parent.") • Inability to think or talk about anything but the illness ("
All our lives were bent
around the problem.")
• Marital discord ("
Our relationship became cold. I felt dead inside.") • Divorce ("
It tore our family apart.") • Preoccupation with "moving away" ("
Maybe if we lived somewhere else, things
would be better.")
• Sleeplessness ("
I've aged double time in the last seven years.") • Weight loss ("
We've been through the mill, and it shows in our health.") • Withdrawal from social activities ("
We don't attend family get-togethers.") • Excessive searching for possible explanations ("
Was it something we did?) • Increased use of alcohol or tranquilizers ("
Our evening drink turned into three
or four.")
• Concern for the future ("
What's going to happen after we're gone? Who will take care of our child?")
British Columbia Schizophrenia Society
10
"A SISTER'S NEED" BY MARGARET MOORMAN
New York Times, September 11, 1988
"My sister Sally is mentally ill. Now 47, she was first hospitalized almost 30 years
ago, during her senior year in boarding school. Labelled schizophrenic then, she is
now diagnosed as having bipolar—or manic-depressive—illness. Generally speaking,
schizophrenia causes thought disorders and bipolar illness causes mood disorders.
When Sally has been manic, she has given away possessions, become obsessed with
elaborate projects, stopped eating and finally, suffered from delusions.
Sally has not worked for pay since 1980, when she was forced to retire from the part-
time position she held as a government clerk. For almost two years after losing her
job, she lived in various apartments, halfway houses and rented rooms. In 1982, our
mother brought her home.
I missed most of the crises of Sally's 20's and 30's. At first, being eight years
younger, I was just not old enough to understand or even to pay much attention. As a
teenager, I tried to ignore Sally because she was different, and I was afraid of being
different myself. I went away to college; after graduating, I moved to Seattle—
about as far as one can get from Arlington. I kept in touch by phone, but I visited
infrequently.
It isn't unusual for someone with a chronically mentally ill sibling to try to run away
from family tensions. It was only by physically removing myself that I felt I could
survive. I was abetted in my escape by my mother, who loved for me to be happy and
was, I know, relieved to have one independent child. Unfortunately, like many
escapees, I had mixed feelings about it, including guilt and dread.
I once thought that when my mother died I would rather kill myself than have to take
care of Sally as she did. It seemed clear: either I would go back home to monitor
Sally, or I would fail my sister utterly and be unable to live with myself. It was just a
choice of which way to give up my life."
"NEVER become a moth around the flame of self-blame. It can
destroy your chance of coping, forever. It can destroy you."
— Dr. Ken Alexander,
14 Principles for the Relatives
British Columbia Schizophrenia Society
11
THE "BLAME AND SHAME" SYNDROME
"People do not cause schizophrenia; they merely blame each other for doing so."
— E. Fuller Torrey, MD.
Unfortunately, there is a common tendency among people with schizophrenia and their family members to blame themselves or to blame one another. Sisters and brothers often share the same worries and fears as their parents. In the following story, a parent describes "blame and shame" from personal experience.
"I have two sons. My older son is 22 and is in an advanced stage of muscular dystrophy. My younger son is 21 and has been diagnosed as chronically mentally ill. The son who is physically disabled has many special needs. He gets emotional support everywhere he turns. His handicap is visible and obvious and the community, family and friends open their hearts to him and go out of their way to make his life better. My other son, on the other hand, has been misunderstood and shunned by all. He is also terribly disabled.but his disability is not visible. His grandparents, aunts, uncles and cousins all think that he's lazy, stupid, weird and naughty. They suggest that somehow, we have made some terrible mistake in his upbringing. When they call on the phone they ask how his brother is and talk to his brother but they never inquire about him. He upsets them. They also wish that he'd go away."
—Excerpt from
Alliance for the Mentally Ill of Southern Arizona Newsletter
"Compassion follows understanding. It is therefore incumbent on us
to understand as best we can. The burden of disease will then
become lighter for all." Dr. E. Fuller Torrey
British Columbia Schizophrenia Society
12
HOW FAMILIES CAN HELP
1. LEARN TO RECOGNIZE SYMPTOMS
When odd behaviour is experienced or observed, it makes good sense to seek advice from a doctor. An acute episode may happen suddenly, or symptoms may develop over a period of time. The following symptoms are important:
• Marked change in personality • A constant feeling of being watched • Difficulty controlling one's thoughts • Hearing voices or sounds others don't hear • Increasing withdrawal from social contacts • Seeing people or things that others don't see • Difficulties with language—words do not make sense • Sudden excesses, such as extreme religiosity • Irrational, angry, or fearful responses to loved ones • Sleeplessness and agitation
These symptoms, even in combination, may not be evidence of schizophrenia. They could be the result of injury, drug use, or extreme emotional distress (a death in the family, for example.) The crucial factor is
the ability to turn off the imagination.
2. GET PROPER MEDICAL HELP
• TAKE THE INITIATIVE. IF SYMPTOMS OF SCHIZOPHRENIA ARE OCCURRING, ASK
YOUR DOCTOR FOR AN ASSESSMENT OR REFERRAL. Family members are usually
the first to notice symptoms and suggest medical help. Remember, if the ill
person accepts hallucinations and delusions as reality, they may resist
treatment.
• BE PERSISTENT. FIND A DOCTOR WHO IS FAMILIAR WITH SCHIZOPHRENIA.
The assessment and treatment of schizophrenia should be done by people
who are well-qualified. Choose a physician who has an interest in the illness,
who is competent and has empathy with patients
and their families.
Remember—if you lack confidence in a physician or psychiatrist, you always
have the right to seek a second opinion.
British Columbia Schizophrenia Society
13
• ASSIST THE DOCTOR/PSYCHIATRIST. Patients with schizophrenia may not be
able to volunteer much information during an assessment. Talk to the doctor
yourself, or write a letter describing your concerns. Be specific. Be persistent.
The information you supply can help the physician towards more accurate
assessment and treatment.
• OTHER SOURCES OF ASSESSMENT AND TREATMENT: The Ministry of Health is
the government department responsible for Mental Health Services in British
Columbia. Assessment and treatment are available through regional Mental
Health centres throughout the province. Check your phone book, or
call the BC Schizophrenia Society to find the one nearest you.
TIPS FOR FIRST CONTACT!
! Rehearse before you call. State what you need
clearly and briefly.
! Make a note of the names of the people you talk to,
along with the date and approximate time.
! If you cannot get the help or information you need,
ask to speak to a case manager, supervisor, or the person in charge.
! If you cannot immediately reach the doctor or case
manager, ask when you may expect a return call, or when the person will be free for you to call back.
British Columbia Schizophrenia Society
14
3. MAKING THE MOST OF TREATMENT
There may be exchanges between doctor and patient that the patient feels are of a highly personal nature and wants to keep confidential. However,
family members need information related to care and treatment. You should be able to discuss the following with the doctor:
• Signs and symptoms of the illness
• Expected course of the illness
• Treatment strategies
• Signs of possible relapse
• Other related information
Provide plenty of support and loving care. Help the person accept their
illness. Try to show by your attitude and behaviour that
there is hope, that the
disease can be managed, and that life can be satisfying and productive.
Help the person with schizophrenia maintain a record of information on:
• Symptoms that have appeared
• All medications, including dosages
• Effects of various types of treatment
4. LEARN TO RECOGNIZE SIGNS OF RELAPSE
Family and friends should be familiar with signs of "relapse"—where the person may suffer a period of deterioration due to a flare up of symptoms. It helps to know that relapse signs often recur for an individual. These vary from person to person, but the most common signs are:
• Increased withdrawal from activities
• Deterioration of basic personal care.
You should also know that:
• Stress and tension make symptoms worse
• Symptoms often diminish as the person gets older.
5. MANAGING FROM DAY TO DAY
ENSURE THAT MEDICAL TREATMENT CONTINUES AFTER HOSPITALIZATION. This
means
taking medication and
going for follow-up treatment.
PROVIDE A STRUCTURED AND PREDICTABLE ENVIRONMENT. Recovering patients
have problems with sensory overload. To reduce stress, keep routines simple, and allow the person time alone each day. Try to plan non-stressful, low-key regular daily activities, and keep "big events" to a minimum.
British Columbia Schizophrenia Society
15
BE CONSISTENT. Caregivers should agree on a plan of action and follow it. If
you are predictable in the way you handle recurring concerns, you can help reduce confusion and stress for the person who is ill. Set limits on how much abnormal behaviour is acceptable, and consistently apply the consequences.
MAINTAIN PEACE AND CALM AT HOME. Thought disorder is a great problem for
most people with schizophrenia. It generally helps to keep voice levels down. When the person is participating in discussions, try to speak one at a time, and at a reasonably moderated pace. Shorter sentences can also help. Above all, avoid arguing about delusions (false beliefs).
BE POSITIVE AND SUPPORTIVE. Being positive instead of critical will help the
person more in the long run. People with schizophrenia need frequent encouragement, since self-esteem is often very fragile. Encourage all positive efforts. Be sure to express appreciation for a job even half-done, because the illness undermines a person's
confidence, initiative, patience, and
memory.
HELP THE ILL PERSON SET REALISTIC GOALS. People with schizophrenia need
lots of encouragement to regain some of their former skills and interests. They may also want to try new things, but should work up to them gradually. If goals are unreasonable, or someone is nagging, the resulting stress can worsen symptoms.
GRADUALLY INCREASE INDEPENDENCE. As participation in a variety of tasks and
activities increases, so should independence. Some relearning is usually necessary for skills such as handling money, cooking, and housekeeping. If outside employment is too difficult, try to help the person plan to use their time constructively.
LEARN HOW TO COPE WITH STRESS TOGETHER. Anticipate the ups and downs
of life and try to prepare accordingly. The person who is ill needs to learn to deal with stress in a socially acceptable manner. Your positive role-modelling can help. Sometimes just recognizing and talking about something in advance that might be stressful can also help.
ENCOURAGE YOUR RELATIVE TO TRY SOMETHING NEW. Offer help selecting an
appropriate activity. If requested, go along the first time for moral support.
British Columbia Schizophrenia Society
16
6. LOOK AFTER YOURSELF AND OTHER FAMILY MEMBERS
BE GOOD TO YOURSELF. SELF-CARE
is very important—even crucial—to
every individual, and ultimately helps the functioning of the entire family. Let go of guilt and shame. Remember—poor parenting or poor communication did not cause this illness, nor is it the result of any personal failure by the individual.
VALUE YOUR OWN PRIVACY. Keep up your friendships and outside interests,
and try to lead as orderly a life as possible.
DO NOT NEGLECT OTHER FAMILY MEMBERS. Brothers and sisters often secretly
share the same guilt and fear as their parents. Or they may worry that they might become ill too. When their concerns are neglected, they may feel jealous or resentful of the ill person. Siblings of people with schizophrenia need special attention and support to deal with these issues.
GET SUPPORT. LEARN FROM OTHERS WHO HAVE SIMILAR EXPERIENCE
Check for resources in your community. If you are the parent, spouse, sibling, or child of someone with schizophrenia—it helps to know
you are not alone. Support groups are good for sharing experiences with others. You will also get useful advice about your local mental health services from those who have "been there." Knowing where to go and who to see—and how to avoid wasting precious time and energy—can make a world of difference when trying to find good treatment. Continuity of care is also important. Ultimately, this involves ongoing medical, financial, housing, and social support systems. All these services are crucial for recovery—yet they tend to be very poorly coordinated. Support groups can help you start putting the pieces of this puzzle together. They can also advocate for better, more integrated services for people with schizophrenia and their families.
√ Call the Mental Health clinic in your community — Ask about
their family education program
√ Look for family support organizations in your region √ Join the BC Schizophrenia Society. Call 604-270-7841 or 1-888-888-0029 for information on becoming a member.
British Columbia Schizophrenia Society
17
FINDING GOOD TREATMENT
"Schizophrenia is not the dreaded disease it was years ago. Now, with early diagnosis and treatment, regular follow-up, proper residential, vocational and rehabilitative support systems, the long-term outcome is quite favourable."
— Psychiatric professional
"Health professionals talk about how things could be or should be. The way things are is that many crucial support systems do not exist. As a result, schizophrenia can become a living hell for the sufferer and his family."— Parent of a young man with schizophrenia
"HOW CAN WE FIND APPROPRIATE MEDICAL HELP?"
Many families are shocked when they try to find a doctor for a relative with
schizophrenia. It seems that very few doctors either know about, or have any
interest in, schizophrenia. There is no easy solution to this problem.
First of all—schizophrenia can resemble other diseases, so assessment and
treatment
must involve well-qualified people. Furthermore, since
schizophrenia is a chronic illness, continuing medical care and prescription
medications are needed. As prominent psychiatrist Fuller Torrey says, "There
is no avoiding the doctor-finding issue."
One way to start is to ask someone in the medical profession whom they
would go to if someone in their family had schizophrenia. Another way is by
talking with other families who have an ill relative. They will often be able to
put you in touch with the best resources in your community, and save you a
lot of time and frustration.
Sharing this type of information is one of the most
valuable assets of your local Schizophrenia Society, and is an important
reason to join the organization. Besides finding someone who is medically competent, you need to find
someone who is interested in the disease, has empathy with its sufferers, and
is good at working with other members of the treatment team.
British Columbia Schizophrenia Society
18
As Dr. Torrey points out:
"Psychologists, psychiatric nurses, social workers, case managers, rehab specialists and others are all part of the therapeutic process. Doctors who are reluctant to work as team members are not good doctors for treating schizophrenia, no matter how skilled they may be in psychopharmacology." Specifically, you need to find a doctor who:
• Believes schizophrenia is a brain disease • Takes a detailed history • Screens for problems that may be related to other possible illnesses • Is knowledgeable about antipsychotic medications • Follows up thoroughly • Adjusts the course of treatment when necessary • Reviews medications regularly • Is interested in the patient's entire welfare, and makes appropriate
referrals for aftercare, housing, social support, and financial aid
• Explains clearly what is going on • Involves the family in the treatment process
In order to get enough information to make informed decisions, you will have to ask the doctor some direct questions:
What do you think causes schizophrenia? What has been your experience with the newer medications like risperidone, clozapine or olanzapine? How important is psychotherapy in treating schizophrenia? What about rehabilitation? If you are uneasy or lack confidence in the medical advice you receive, remember—you do have the right to another opinion from other doctors, even if from another city.
"HOW IS SCHIZOPHRENIA TREATED?"
Although schizophrenia is not yet a "curable" disease, it
is treatable. The proper treatment of schizophrenia includes the following:
MEDICATION Most patients with schizophrenia have to take medication
regularly to keep their illness under control. It is not possible to know in advance which medication will work best for an individual. Many medication adjustments may be required. This period of trial and error can be very difficult for everyone involved. Some medications have unpleasant side effects—dry mouth, drowsiness, stiffness, restlessness, etc.
British Columbia Schizophrenia Society
19
EDUCATION Patients and their families must learn all they can about
schizophrenia.
They should also be directly included in planning the treatment program. Families should find out what assistance is available in their community—including day programs, self-help groups, and work and recreation programs. It is most important for the patient and the family to accept the fact of the illness, and begin to learn how best to manage it.
FAMILY COUNSELLING Since the patient and the family are often under
enormous emotional strain, it may be advantageous to obtain counselling from professionals who understand the illness.
HOSPITALIZATION AND REGULAR FOLLOW-UP If someone becomes acutely ill
with schizophrenia, they will probably require hospitalization. This allows the patient to be observed, assessed, diagnosed, and started on medication under the supervision of trained staff. The purpose of hospitalization is proper medical care and protection. Once the illness is stabilized and the patient is discharged from hospital,
regular follow-up care will reduce the chances of relapse.
RESIDENTIAL AND REHABILITATION PROGRAMS Social skills training, along
with residential, recreational, and vocational opportunities tailored to people with mental illness are very important. Used as part of the treatment plan, they can result in improved outcomes for even the most severely disabled people.
SELF-HELP GROUPS Families can be very effective in supporting each other
and in advocating for much-needed research, public education, and community and hospital-based programs. People with mental illness can also provide consultation and advocacy in these areas, as well as offering peer support to other individuals with schizophrenia.
NUTRITION, REST AND EXERCISE Recovery from schizophrenia, as with any
illness, requires patience. It is aided by a well-balanced diet, adequate sleep, and regular exercise. However, the illness and the side effects of medication can interfere with proper eating, sleeping, and exercise habits. There may be appetite loss, lack of motivation, and withdrawal from normal daily activity. Someone who is ill may simply forget to eat, or become very suspicious about food, so supervision of daily routines may be required. If you are a family member or friend who is trying to help—
be patient. Above all, don't take seeming carelessness or disinterest personally.
ELECTROCONVULSIVE THERAPY (ECT) ECT is
not normally used for patients
with schizophrenia unless they are also suffering from extreme depression, are suicidal for long periods, and do not respond to medication or other treatments.
British Columbia Schizophrenia Society
20
PROMISING DEVELOPMENTS
"Schizophrenia is a most complex and puzzling disease. And now, after 100 years of enigmatic puzzling, I believe we may be on the threshold of an entire new era of understanding."
Dr. Peter Liddle, Jack Bell Chair in Schizophrenia Research
Head, Schizophrenia Division, University of British Columbia, 2001
According to Dr. Liddle, the more we understand the higher functions of the brain and its interactions, the more we can explore, in a meaningful way, how the mind and the brain work together.
In other words, we can finally go beyond
notions and provide rational bases for why certain treatments work. The reason for this is the development of tools and techniques that now allow us to systematically explore patterns of brain activity.
• EEG's
(Electroencephalograms) show that electrical impulses used by the brain to send messages to other parts of the body are abnormal in many people with schizophrenia.
• CT
(Computerized Tomography) and MRI
(Magnetic Resonance
Imaging) scans show that brain structures of some people with
schizophrenia are different from people without the illness. One important
anomaly in schizophrenia, for example, is enlarged ventricles the small
spaces in the brain through which cerebral spinal fluid circulates.
• PET
(Positron Emission Tomography) uses a radioactive compound to help measure blood flow in different parts of the brain. It is possible to see, for instance, how the brain activity in people with schizophrenia differs from that of people who are not ill—and to identify the specific areas where such differences occur.
Partly because of the development of these new tools, treatment for schizophrenia has greatly improved—and will continue to be influenced by new research discoveries.
British Columbia Schizophrenia Society
21
MEDICATION UPDATE
"
There is no way at present to predict who will respond best to which medication."
— E. Fuller Torrey
Trying to understand a bewildering array of medication terminology can be frustrating. It's always a good idea to learn at least some of the technical "lingo" that mental health professionals use. A user-friendly reference book, such as Fuller Torrey's
Surviving Schizophrenia, is a great help.
Generally, medications for treating psychotic symptoms of schizophrenia are referred to as
antipsychotics, or sometimes
neuroleptics.
"STANDARD" ANTIPSYCHOTICS
Until recently, doctors referred to antipsychotic medications as
neuroleptics because of their tendency to cause neurological side effects. Medications that have been around for a number of years are now called "standard" antipsychotics. Examples of standard antipsychotics include
Thorazine, Mellaril, Modecate, Proloxin, Navane, Stelazine and
Haldol.
SIDE EFFECTS (EPS)
Side effects can be a major problem with standard antipsychotic medications. These
neurological side effects are called
"extrapyramidal symptoms" (
EPS for short).
Specific examples of EPS include akinesia (slowed movement), akathisia (restless
limbs), and tardive dyskinesia (permanent, irreversible movement disorders.)
"ATYPICAL" ANTIPSYCHOTICS
The newer antipsychotic drugs are called "atypical" antipsychotics. Atypical medications are being used more and more frequently. They are called "atypical" because they:
• do not have the same chemical profiles as standard medications;
• seem to work in a different way than standard medications; and
• cause fewer side effects than standard medications, helping patients to stabilize
At the moment, there are four atypical antipsychotics available in BC—
risperidone (Risperdal),
clozapine (Clozaril),
olanzapine (Zyprexa) and the newest medication,
quetiapine (Seroquel).
RISPERIDONE (ALSO KNOWN AS
RISPERDAL)
The use of risperidone to date has been encouraging. While not effective for everyone, it is now generally accepted as first-line treatment for newly-diagnosed patients. Side effects—which often discourage people from taking their medication—are usually minimal at regular maintenance dosages.
CLOZAPINE (
CLOZARIL)
Clozapine has been acclaimed because about one-third of patients with treatment-resistant (called
refractory) schizophrenia who do not respond to other medications show at least some improvement on clozapine. It is also recommended for people who are showing signs of tardive dyskinesia, since it rarely causes or worsens this condition.
British Columbia Schizophrenia Society
22
The major drawback of clozapine is the slight risk (1%) that it will cause white blood cells to decrease, thereby decreasing the person's resistance to infection. People taking clozapine must have their blood counts monitored very regularly (once a week or every two weeks.)
OLANZAPINE (
ZYPREXA)
Reports to date on the use of olanzapine are very encouraging, showing high rates of efficacy and a low side effect profile. All of this makes it ideal as a first-line treatment. Unfortunately, it is still not available for this purpose on the BC
Pharmacare formulary a situation which we hope will change in the near future. The BC Schizophrenia Society continues to encourage government to make all new medications equally available to all patients.
QUETIAPINE (
SEROQUEL)
Quetiapine, the most recently-approved medication, also shows high rates of efficacy and low side effects, making it also a good choice for first-line treatment. It is now accessible to all patients in BC through the province's
Pharmacare formulary.
OTHER NEW ANTIPSYCHOTICS
Several new antipsychotic medications are being tested or waiting for approval. Most of the new drugs are "atypicals"— meaning they fall into the same category as risperidone, olanzapine, quetiapine, and clozapine.
REASONS FOR SWITCHING MEDICATION
The most common reasons for switching from a standard to an "atypical" antipsychotic are:
• Persistent positive symptoms (hallucinations, delusions, etc.)
despite taking medication regularly
• Persistent negative symptoms (blunted emotions, social
withdrawal, etc.) despite medication
• Severe discomfort from side effects, little or no relief from the
usual side effect medications
• Tardive dyskinesia
In most cases, switching medications from standard to "atypical" can be done
at any time. The person who is ill should take lots of time to think about it and
talk it over with family, friends, and their treatment team. People should also
be aware that atypical antipsychotics may have side effects of their own, such
as weight gain and sexual dysfunction. It's true that the newer medications
tend to produce fewer side effects—but they may still cause some.
Patients
taking atypical antipsychotics must continue to be monitored for side effects.
British Columbia Schizophrenia Society
23
Rehabilitation can be provided only after stabilization.
REALITY:
Rehabilitation should begin on Day One.
— Dr. Courtenay Harding, University of Colorado School of Medicine
Some of the most recent and hopeful news in schizophrenia research is emerging from studies in the field of psychosocial "
rehab." New studies challenge several long-held myths in psychiatry about the inability of people with schizophrenia to recover from their illness. It appears that such myths, by being overly pessimistic about outcomes, may significantly reduce patients' opportunities for improvement and/or recovery. In fact, the long-term perspective on schizophrenia should give everyone a renewed sense of hope and optimism. According to Dr. G. Gross, author of a 22-year study of 508 patients with schizophrenia:
"
.schizophrenia does not seem to be a disease of slow, progressive deterioration. Even in the second and third decades of illness, there is still potential for full or partial recovery."
It is now clear that appropriate cognitive assessments and good rehabilitation
programs are an important part of treatment strategy. In addition, where
family input is solicited and families are included as part of the treatment
"team", patient outcomes are greatly improved.
Families need and want education, information, coping and communication
skills, emotional support, and to be treated as collaborators. For this reason,
knowledgeable clinicians make a special effort to involve family members.
Once a relationship is established, clinician, patient and family can work
together to identify needs and appropriate interventions. When everyone has
the information they need, they are better able to have realistic yet optimistic
expectations about improvement and possible recovery.
Studies show that families who are educated are supportive, non-judgmental,
and, most especially,
non-critical. They can do much to help patients recover.
On the other hand, patients who are around chaotic or volatile family
members usually have a more difficult time, and have to return to hospital
more often.
Since we now know this, it is important for family members to assess their
own coping skills and try to anticipate and adapt to the ups and downs of the
illness. Calm assurance, assistance, and support from family members can
make a difference to the person with schizophrenia.
British Columbia Schizophrenia Society
24
FAQ'S: "FREQUENTLY ASKED QUESTIONS"
"Schizophrenia affects young people in the prime of their lives. It can be a major set-back in their plans and hopes for the future."
Dr. Ian Falloon
1. Q. WHAT ARE MY CHANCES OF DEVELOPING SCHIZOPHRENIA?
A. There is no way of knowing exactly who will get schizophrenia.
However, about 1 in 100 people worldwide will develop the illness. Since schizophrenia tends to run in families, your chances may be higher if someone in your family has the disease. For example, it is estimated that:
• If one of your parents or a brother or sister is ill, the risk factor is
• If both your parents are ill, your chances are about 40% • If a nonidentical twin is ill, your chances are 10-15% • If an identical twin is ill, your chances are 35-50% • If you are a grandchild, niece, nephew, aunt or uncle of someone
who is ill, your chances are about 3%.
• Schizophrenia does not discriminate between the sexes. Young men
and women are equally at risk for developing the illness.
2. Q. CAN CHILDREN DEVELOP SCHIZOPHRENIA?
A. Yes. In rare instances, children as young as five have been diagnosed
with the illness. They are often described as being different from other
children from an early age. Most people with schizophrenia, however, do
not show recognizable symptoms until adolescence or young adulthood.
3. Q. HOW CAN I TELL IF I HAVE SCHIZOPHRENIA BEFORE IT BECOMES SERIOUS?
A. If you think you have symptoms of schizophrenia, you should talk to a
doctor who has experience treating the illness. This is very important because
early diagnosis and treatment means a better long-term prognosis.
4. Q. IF I HAVE SCHIZOPHRENIA, SHOULD I HAVE CHILDREN?
A. Schizophrenia tends to run in families, but that doesn't necessarily
mean you should not marry and have children. Since everyone wants to be a good parent and provider for their family, you will need to ask yourself some important questions:
• Is my illness sufficiently under control? If I have to work full-time in
order to support my children, can I do it?
• Will the stress and expense of raising children cause me to become
British Columbia Schizophrenia Society
25
• What if my children inherit the illness? (The chance of each of your
children developing schizophrenia is 1 in 10. If your partner also has schizophrenia, the chance of each child developing the illness increases to 2 in 5.)
• Is my partner a capable person who can help provide a secure and
peaceful home environment for a child?
As you see, these decisions are very personal—and will depend entirely on you and your own particular situation.
5. Q. MY FRIEND HAS SCHIZOPHRENIA. HOW CAN I HELP?
A. We all need friends who stick with us through good times and bad.
People with schizophrenia will value your friendship. They are often discriminated against by those who are ignorant about the illness. Many people with schizophrenia have high IQ's. Unless someone is experiencing symptoms of their illness, there will be nothing especially unusual about their behaviour.
You can be a real friend by trying to understand the illness and by educating others when the opportunity arises. Let them know the facts. Also, if you can, try to get to know your friend's family. For example, the family might help you understand how your friend may sometimes be overwhelmed and discouraged because of the chronic and persistent nature of the illness. Once you know this, you can help by just being supportive and encouraging during these rough times.
If you're planning social activities with your friend, it helps to remember:
• People with schizophrenia need to take their medication on time,
keep a fairly regular schedule, and get enough sleep and rest.
• Because there may be some disabling periods of thought disorder,
term papers and studying for exams can't be left until the last minute
• Using street drugs is very dangerous because they often trigger a
return of symptoms (a relapse).
6. Q. DO STREET DRUGS EVER
CAUSE SCHIZOPHRENIA?
A. No. Street drugs do not actually
cause schizophrenia. Since some
people who take street drugs may show schizophrenia-like symptoms, people who have schizophrenia are sometimes accused of being "high" on drugs. A person suffering from psychotic symptoms may also become involved in substance abuse, where having such symptoms in the setting of
getting high is seen as normal.
British Columbia Schizophrenia Society
26
Q. DOES A HISTORY OF MENTAL ILLNESS OR SCHIZOPHRENIA IN MY FAMILY
MEAN THERE IS A GREATER RISK OF HAVING A PSYCHOTIC EPISODE IF I
USE STREET DRUGS?
A. Evidence indicates that if someone has a predisposing factor, drugs
like cannabis (marijuana, hash, hash oil, etc.) may trigger an episode of schizophrenia. This may or may not clear up when use of the drug stops. If your family has a history of mental illness, extra caution might be wise.
Street drugs can be risky for anyone, but for people with schizophrenia, they are particularly dangerous. As mentioned earlier, certain drugs can cause relapses and make the illness worse.
All street drugs should be avoided, including:
• PCP (angel dust) • cocaine/crack • LSD • amphetamines • marijuana and other cannabis products • ecstasy
Q. WHAT ABOUT ALCOHOL, COFFEE AND TOBACCO?
A.
Moderate use of alcohol (one or two glasses of wine or beer) doesn't
seem to trigger psychotic symptoms, but heavy use certainly does.
People on medication should be especially careful. Since alcohol is a depressant, it can be life-threatening when combined with medications like tranquilizers (clonazapam, Rivotril, Ativan, Valium, alprazolam, etc.) Each multiplies the effect of the other—often with disastrous results.
THE FOLLOWING MAY ALSO TRIGGER SYMPTOMS OF SCHIZOPHRENIA:
• large amounts of nicotine and/or caffeine • cold medications and nasal decongestants.
British Columbia Schizophrenia Society
27
EDUCATION AND SCHIZOPHRENIA "I'M A TEACHER—WHAT CAN I DO?"
"Professionals . must help the ill person set realistic goals. I would entreat them not to be devastated by our illness and transmit this hopeless attitude to us. I urge them never to lose hope; for we will not strive if we believe the effort is futile."
— Esso Leete, patient who has had schizophrenia for 20 years
1. ARM YOURSELF WITH THE FACTS
Schizophrenia is a very common illness (1 in 100.) It strikes in the mid to late teens and early twenties. You need to be aware that:
•
Early intervention and early use of new medications lead to better
medical outcomes for the individual
• The earlier someone with schizophrenia is diagnosed and stabilized
on treatment, the better the long-term prognosis for their illness
• Teen suicide is a growing problem—and teens with schizophrenia
have a
50% risk of attempted suicide
• In rare instances, children as young as five can develop
2. BRING THE ILLNESS INTO THE OPEN
• Discuss schizophrenia in class in a matter-of-fact way. This helps dispel
some of the myths and reduces discrimination and injustice associated with the illness.
• Provide information on precipitating factors, such as drug abuse.
3. BE ALERT TO EARLY WARNING SIGNS OF SCHIZOPHRENIA
Young people are sometimes apathetic, have mood swings, or experience declines in athletic or academic performance. But if these things persist, you should talk to the family and help the student receive an assessment.
"REACHING OUT" AN EXCELLENT TEACHING RESOURCE TO HELP STUDENTS LEARN ABOUT BRAIN FUNCTION AND MENTAL
ILLNESS. THE RESOURCE ALSO STRESSES THE IMPORTANCE OF GETTING HELP EARLY. SEE PAGE 43 FOR DETAILS.
British Columbia Schizophrenia Society
28
4. IF YOU HAVE A STUDENT WITH SCHIZOPHRENIA IN YOUR CLASS:
• Learn as much as you can about the illness so you can understand the
very real difficulties the person is experiencing
• Reduce stress by going slowly when introducing new situations
• Check the student's cognitive assessment, and help set realistic goals for
academic achievement and extra-curricular activities
• Establish regular meetings with the family for feedback on health and
progress. It may be necessary to modify objectives, curriculum content, teaching methodology, evaluation formats, etc.
• Encourage other students to be kind and to extend their friendship. Some
may wish to act as peer supports when illness occurs and some catch-up help is needed.
5. TEACHERS AND COUNSELLORS CAN ALSO HELP RAISE AWARENESS BY:
• Holding information sessions about mental illness at parents' meetings and
at student assemblies
• Setting up displays for special occasions (such as Mental Illness
Awareness Week) in the school library or counselling office
• Ordering up-to-date resource materials for your library, finding current
information on the internet, and discarding out-of-date literature.
"PARTNERSHIP" EDUCATION
The BC Schizophrenia Society's PARTNERSHIP EDUCATION
program is an
invaluable aid for helping students understand the nature and prevalence of chronic and severe mental illness. PARTNERSHIP EDUCATION brings together three individuals who work as a team to present the facts about schizophrenia. One person has a psychiatric diagnosis, one is a family member, and one is a mental health professional. They come into your classroom together, each to tell their personal story.
PARTNERSHIP EDUCATION
presentations elicit immediate and thoughtful
class participation. Mental illness is demystified. Students' questions are answered directly by people with first-hand knowledge and experience. The
PARTNERSHIP EDUCATION program helps fight ignorance, prejudice,
dusty old Hollywood myths, and hurtful stereotypes. It also provides vital facts about the physical nature of mental illness, and helps many individual students whose family members suffer from mental illness.
British Columbia Schizophrenia Society
29
MYTHS AND MISCONCEPTIONS
"The worst thing about having schizophrenia is the isolation and the loneliness."
— Dr. Phillip Long, psychiatrist
SOCIETY'S KNOWLEDGE OF MAJOR MENTAL ILLNESS LAGS WAY BEHIND THE FACTS.
People with schizophrenia are victims of this general ignorance. In truth, they are victims twice over. First, they have an incurable, chronic brain disease that they must learn to live with as best they can. Next, because of their illness, they are discriminated against.
WHAT IS THE BIGGEST PROBLEM FOR PEOPLE WITH MENTAL ILLNESS?
Most say it's that others do not accept them. Once they have learned to manage their symptoms, they still have to face overwhelming difficulties with friends, housing, and work. They feel the sting of discrimination in almost everything they do. Old friends and even some family members are uncomfortable in their presence. It is easy to become isolated, cut off from society. No wonder so many people with schizophrenia feel they don't belong; that they are "different"; that they are not respected or valued.
Widespread, hurtful ignorance leads to the terrible social isolation and loneliness that can become the most disabling feature of the illness.
WHY DO PEOPLE FIND MENTAL ILLNESS SO UNACCEPTABLE?
FEAR OF VIOLENCE
Some people fear that individuals who suffer from mental illness are violent. In reality, people with a mental illness are usually anxious, fearful of others, and passive. The myth of danger is largely based on inaccurate and outdated cultural myths that portrayed people with mental illness as aggressive and violent. Problems with aggression can arise for a small minority of people who (i) are not taking medication; (ii) habitually abuse drugs and/or alcohol; and (iii) have a history of violence towards themselves or others. Otherwise, statistics show that people with mental illness are
less violent than the general population, and tend rather to be the
victims of violence.
British Columbia Schizophrenia Society
30
FEAR OF CRIMINAL INTENTIONS
People with psychiatric disorders are no more likely to commit crimes than the general population. However, if mental illness is left untreated and allowed to become progressively more severe, people who are acutely ill may inadvertently end up in jail. Another common confusion has to do with the nature of involuntary hospitalization, which is sometimes necessary to treat and safeguard someone who is very ill.
Hospitalization for medical treatment to regain one's health should never be falsely equated with incarceration in the criminal justice system.
FEAR OF THE UNKNOWN
People often fear what they do not understand. And when they don't understand, they often make wild guesses. Some cultures believe mental illness is the work of evil spirits, while others believe it is caused by bad blood, poisons, or lack of moral integrity. As people nowadays understand more about the brain and the biological causes of brain disease, these harmful beliefs are quickly fading.
AVERSION TO ILLNESS
After hundreds of years, "mental illness" has finally been identified as a disease just like epilepsy, Parkinsonism, or diabetes. But this change from the realm of the witch doctor to the medical doctor doesn't erase all negative feeling—only lessens it somewhat. The public still has a very strong aversion to hospitals, disease, and doctors.
BETTER PUBLIC HEALTH EDUCATION PROGRAMS CAN HELP DO AWAY WITH OLD MYTHS AND MISUNDERSTANDINGS.
GIVING PATIENTS THE NECESSARY SUPPORTS TO LIVE WITH DIGNITY IN THEIR OWN COMMUNITIES ALSO HELPS OVERCOME
PREJUDICE AGAINST PEOPLE WITH MENTAL ILLNESS.
British Columbia Schizophrenia Society
31
BENEFITS OF RESEARCH
"Perhaps the one factor which holds back psychiatric research more than any other is the social stigma that remains attached to mental disease."
— Dr. Henry Friesen, Past President - Medical Research Council of
For many years, there was a lack of advocates to present the facts about schizophrenia. Funding for schizophrenia research lagged quite far behind funding for other illnesses. In his 1995 address to the Canadian Psychiatric Association, Medical Research Council President Dr. Henry Friesen praised the initiative shown by Nobel Laureate in Chemistry, the late Dr. Michael Smith
generously donated half his Nobel Prize money towards the promotion of research training in schizophrenia:
To me, it was an inspirational act for Dr. Smith to associate himself with the research field, thereby raising the profile of schizophrenia—and promoting the notion of schizophrenia as a disease worthy of academic investigation and support.
UNDERSTANDING BRINGS PROGRESS, HOPE
The goal of research is to eventually find a cure. Meanwhile, there are many great "trickle-down" benefits to funding research. Research, by its very nature, requires researchers to be up-to-date on everything of importance in their field. Researchers become mentors they teach at universities, thus informing a great many young students about the latest in schizophrenia research and ultimately enticing some of them to continue in this field. At the same time, the researchers are training doctors, psychiatrists and other health professionals to familiarize themselves with the most up-to-date treatment methods. This body of knowledge spreads, not only to students and health professionals, but also to family organizations, government, other support agencies, educators and counsellors and eventually to the general public. Finally, the old myths about schizophrenia and other serious mental illnesses begin to fade and disappear because of the knowledge being disseminated.
British Columbia Schizophrenia Society
32
COST OF SCHIZOPHRENIA
! Schizophrenia costs Canadians more than $2.3 billion in direct health care
funds and an additional $2 billion in support costs such as welfare, family benefits and community support services, for a total of $4.3 billion per
year. The cost in terms of human suffering is immeasurable…
! People with schizophrenia occupy more hospital beds than those with any
other illness. One out of every twelve hospital beds in Canada is occupied
by someone with schizophrenia.
! Given the high costs and the high relative prevalence
e of schizophrenia,
many more research dollars should be allocated for schizophrenia than is currently the case.
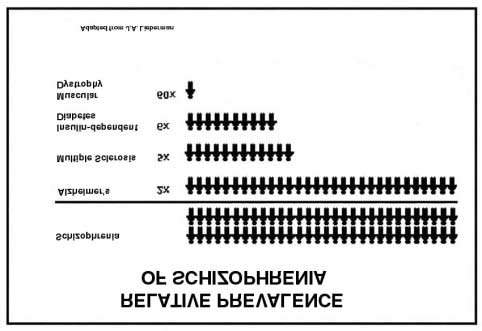
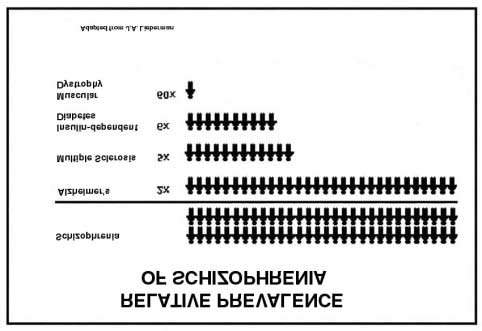
! For example, schizophrenia is twice as prevalent as Alzheimer's
disease, 5 times as prevalent as multiple sclerosis, 6 times as prevalent
as diabetes, and 60 times more prevalent than muscular dystrophy.
(See table, below.)
British Columbia Schizophrenia Society 33
BC SCHIZOPHRENIA SOCIETY (BCSS)
"We'd like to change your mind
We'd like to change your mind""
PROVINCIAL OFFICE 201 - 6011 Westminster Hwy Richmond, B.C. V7C 4V4 (604) 270-7841 or 1-888-888-0029 [email protected] www.bcss.org
MISSION STATEMENT: "To alleviate the suffering caused by schizophrenia" OBJECTIVES:
SUPPORT Support groups throughout the province for families and friends of
people with schizophrenia and other serious mental illness
EDUCATION Partnership and family education programs for increasing public
awareness and understanding about serious mental illness
ADVOCACY Advocating for improved legislation and better services for people
with schizophrenia and their families
RESEARCH Active fundraising for research into the causes and treatment of
The BC Schizophrenia Society has branches across the province. To reach the branch nearest you, check your local phone listings or contact us at (604) 270-7841 or toll free at 1-888-888-0029. Abbotsford
Surrey/White Rock
Vancouver/Richmond
Parksville/Qualicum
British Columbia Schizophrenia Society 34
BRITISH COLUMBIA SCHIZOPHRENIA SOCIETY (BCSS)
BCSS Family Coordinatorss
BCSS has Family Coordinators in most regions of British Columbia to help coordinate services, support, and education for family members of people suffering from:
• First episode psychosis
• Schizophrenia
• Bipolar disorder
• Other serious brain disorders.
BCSS Program Coordinators
BCSS Program Coordinators deliver the following BCSS programs:
• KIDS IN CONTROL Information, education and support for
children eight to thirteen years of age who have a parent with a mental illness
• RESPITE PROGRAM Respite services for family members
who are primary caregivers to people with serious mental illness
S A 14-week course focused on education and
recovery for people with mental illness.
BCSS Coordinators can be reached by contacting the BC Schizophrenia Society Provincial Office. 604-270-7841 BC toll free 1-888-888-0029
Or check out our website at
British Columbia Schizophrenia Society 35
Help for Families Outside British Columbia
Schizophrenia Society of Alberta
Assn. Québécoise de la Schizophrénie
(780) 429-7880 1-800-661-4644
Tel: (514) 251-4000 1-800-323-0474
MANITOBA
AMI Quebec (Anglophone Association)
Manitoba Schizophrenia Society
Tel: (514) 486-1448
(204) 786-1616 1-800-263-5545
[email protected]
NEW BRUNSWICK
SCHIZOPHRENIA SOCIETY OF CANADA
Schizophrenia Society of New Brunswick
50 Acadia Ave., Ste 205,
Markham, Ontario, M3C 2E9
(416) 415-2007 1-888-772-4673
NEWFOUNDLAND& LABRADOR
Schizophrenia Society of Newfoundland
and Labrador Tel: (709) 745-7765
WORLD FELLOWSHIP FOR SCHIZOPHRENIA
AND ALLIED DISORDERS
124 Merton Street, Suite 507
NOVA SCOTIA
Toronto, Ontario M4S 2Z2
Schizophrenia Society of Nova Scotia
T: (416) 961-2855 F: (416) 961-1948
Tel: (902) 465-2601 1-800-465-2601
[email protected]
Schizophrenia Society of Ontario
IN THE UNITED STATES - NAMI
(416) 449-6830 1-800-449-6367
(National Alliance for the Mentally Ill)
[email protected]
NAMI's toll-free helpline provides referrals
PRINCE EDWARD ISLAND
to local support groups and information
Schizophrenia Society of P.E.I.
1-800-950-NAMI http://www.nami.org
IN EUROPE: EUFAMI – Headquartered in
Belgium. Affiliated with 16 mental illness
Schizophrenia Society of Saskatchewan
support organizations throughout Europe.
(306) 584-2620 [email protected]
http://www.eufami.org
British Columbia Schizophrenia Society 36
RESOURCE MATERIALS ON SCHIZOPHRENIA
The BC Schizophrenia Society Provincial Office has a library of up-to-date pamphlets, books, and videos. For complete information on library resource materials, please contact us: #201 - 6011 Westminster Hwy, Richmond, BC V7C 4V4 Phone (604) 270-7841 1-888-888-0029 [email protected] www.bcss.org
SUGGESTED READING
The following books are highly recommended, and should be available through your local library or bookstore.
Adamec, Christine. How to Live with a Mentally Ill Person. John Wiley & Sons, 1996
Amador, Xavier. I am not Sick, I Don't Need Help! Vida Press, Peconic, NY 2000
Keefe, Richard & Harvey, D. Understanding Schizophrenia: A Guide to the New Research
on Causes and Treatment. The Free Press, Macmillan, Toronto, 1994
Lafond, Virginia. Grieving Mental Illness: A Guide for Patients and Their Caregivers.
University of Toronto Press, 1994
Marsh, D. and Dickens, R. How to Cope with Mental Illness in Your Family. Tarcher/
Putnam, NY, 1998
Mueser, Kim T. & Gingerich, Susan. Coping With Schizophrenia: A Guide for Families.
New Harbinger, Oakland, CA, 1994
Torrey, E. Fuller. Surviving Schizophrenia. 4th edition. HarperCollins Perennial (paperback).
New York, 2001 ∗
Woolis, Rebecca. When Someone You Love Has a Mental Illness: A Handbook for Family,
Friends,
Caregivers. Putnam's Sons, New York, 1992.
EARLY PSYCHOSIS EDUCATION RESOURCES 2003
"REACHING OUT: THE IMPORTANCE OF EARLY INTERVENTION"
The sooner someone with psychosis receives proper medical treatment, the better the outcome will be for their illness. Young people, parents, teachers, family physicians and others need to know that early intervention and treatment of psychosis can make a vital difference. All "Reaching Out" Early Psychosis Education Resources are designed to heighten awareness of the early signs and symptoms of psychosis and the need for appropriate and timely medical assessment.
EARLY PSYCHOSIS RESOURCE DETAILS AND ORDER FORM ON PAGES 42, 43.
∗ Particularly recommended as good starting point for family members, consumers, and service providers. It is clearly written and has an excellent reference section.
British Columbia Schizophrenia Society 37
GLOSSARY: UNDERSTANDING THE LANGUAGE OF MENTAL ILLNESS
People with mental illness, their relatives, teachers and friends may hear medical professionals using words they are not familiar with. Here's a short glossary of some of the most commonly used terms…
AFFECTIVE DISORDERS OR MOOD DISORDERS Mental illness characterized by greatly
exaggerated emotional reactions and mood swings from high elation to deep depression. Commonly used terms are bipolar disorder (formerly called manic depression) and depression—although some people experience only mania and others only depression. These extreme mood changes are unrelated to changes in the person's environment.
COGNITIVE DEFICITS, COGNITIVE TESTING Deficits in specific sorts of brain functioning.
For example, people with schizophrenia often have trouble performing "executive"
functions short-term memory, organizing, planning, prioritizing. Reliable, objective
testing is now available to pinpoint areas in which someone has difficulty, so they can
better identify their problems and find resources to help with day-to-day living. Cognitive
testing for people with schizophrenia also helps health authorities do more effective
service planning plan for people with schizophrenia.
DELUSION A fixed belief that has no basis in reality. People suffering from this type of
thought disorder are often convinced they are famous people, are being persecuted, or are capable of extraordinary accomplishments.
DIAGNOSIS Classification of a disease by studying its signs and symptoms.
Schizophrenia is one of many possible diagnostic categories used in psychiatry.
ELECTRO CONVULSIVE THERAPY (ECT) Used primarily for patients suffering from
extreme depression for long periods, who are suicidal, and who do not respond to medication or to changes in circumstances.
HALLUCINATION An abnormal experience in perception. Seeing, hearing, smelling,
tasting or feeling things that are not there.
INVOLUNTARY ADMISSION The process of entering a hospital is called admission.
Voluntary admission means the patient requests treatment, and is free to leave the hospital whenever he or she wishes. People who are very ill may be admitted to a mental health facility against their will, or involuntarily. There are two ways this can occur:
! Under medical admission certificate or renewal certificate ! Under special court order when the person has been charged or convicted
with a criminal offence. In this case, they may be held in a forensic facility.
British Columbia Schizophrenia Society 38
In British Columbia, before someone can be admitted involuntarily, a physician must certify that the person is:
! Suffering from a mental disorder and requiring care, protection and medical
treatment in hospital
! Unable to fully understand and make an informed decision regarding
treatment, care and supervision
! Likely to cause harm to self or others, or to suffer substantial mental or
physical deterioration if not hospitalized.
MEDICATIONS Medication is usually prescribed in either pill or injectable form. Several
different types of medications may be used, depending on the diagnosis. Ask your doctor or pharmacist to explain the names, dosages, and functions of all medications, and to separate generic names from brand names in order to reduce confusion.
1) ANTIPSYCHOTICS:: Brand Names—Modecate, Largactil, Stelazine, Haldol, Fluanxol, Pipartil, Clozaril, Risperdal, Zyprexa. Seroquel. Generic Names—fluphenazine, chlorpromazine, trifluoperazine, haloperidol, flupenthixol, pipotiazine, clozapine, risperidone, olanzapine, quetiapine. These reduce agitation, diminish hallucinations and destructive behaviour, and may bring about some correction of other thought disorders. Side effects include changes in the central nervous system affecting speech and movement, and reactions affecting the blood, skin, liver and eyes. Periodic monitoring of blood and liver functions is advisable.
2) ANTIDEPRESSANTS: Relatively slow-acting drugs—but if no improvement is
experienced after three weeks, they may not be effective at all. Some side effects may occur, but these are not as severe as side effects of antipsychotics.
3) MOOD NORMALIZERS: e.g., Lithium, Carbamazepine, Valproate. Used in manic
and manic-depressive states to help stabilize wide mood swings that are part of the condition. Regular blood checks are necessary to ensure proper medication levels. There may be some side effects such as thirst and burning sensations.
4) TRANQUILIZERS: Valium, Librium, Ativan, Xanax, Rivotril. Generally referred to
as benzodiazepines. These medications can help calm agitation and anxiety.
5) SIDE EFFECT MEDICATIONS:: Also called anticholinergics. Brand Names—
Cogentin, Kemadrin. Generic Names—benzotropine, procyclidine.
MENTAL HEALTH A balanced relationship between (a) the individual; (b) his or her
immediate social group family, friends, peers, colleagues and (c) the larger political, economic and social environment. "Mental health" includes psychological and social well-being, a sense of harmony, and environmental mastery.
MENTAL I LLNESS/ MENTAL DISORDER Physical abnormality and/or biochemical
irregularity in the brain causing substantial disorder of thought, mood, perception, orientation, or memory—grossly impairing judgement, behaviour, capacity to reason, or ability to meet the ordinary demands of life.
British Columbia Schizophrenia Society 39
MENTAL HEALTH ACT Provincial legislation for the medical care and protection of
people who have a mental illness. The Mental Health Act also ensures the rights of patients who are involuntarily admitted to hospital, and describes advocacy and review procedures.
PARANOIA A tendency toward unwarranted suspicions of people and situations.
People with paranoia may think others are ridiculing them or plotting against them. Paranoia falls within the category of delusional thinking, which is often based on hallucinatory experience.
PSYCHOSIS Hallucinations, delusions, and loss of contact with reality.
SCHIZOPHRENIA Severe and sometimes chronic brain disease. Common symptoms—
personality changes, withdrawal, severe thought and language difficulties, hallucinations, delusions, bizarre behaviour.
SIDE EFFECTS Side effects occur when there is drug reaction that goes beyond or is
unrelated to the drug's therapeutic effect. Some side effects are tolerable, but some are so disturbing that the medication must be stopped. Less severe side effects include dry mouth, restlessness, stiffness, and constipation. More severe side effects include blurred vision, excess salivation, involuntary body movements, nervousness, sleeplessness, tardive dyskinesia, and blood disorders. Some drugs are available to control side effects. Learning to recognize side effects is important because they are sometimes confused with symptoms of the illness. A doctor, pharmacist, or mental health professional can explain the difference between symptoms of the illness and side effects due to medication.
TREATMENT Refers to remedies or therapies designed to cure an illness or relieve
symptoms. In psychiatry, treatment is often a combination of medication, education about the illness, cognitive testing and cognitive therapy, counselling (advice), and recommended activities. Together, these make up the individual's treatment plan.
British Columbia Schizophrenia Society 40
Get the Facts:
THE MENTAL HEALTH ACT = THE RIGHT TO TREATMENT AND CARE
• Due to a chemical imbalance that affects the brain, many people who
become acutely ill with schizophrenia are unable to recognize their illness. That means they are unable to voluntarily exercise their right to available treatment—because of the very nature of their disability. The British Columbia Mental Health Act is about the care and protection of our citizens who are victims of such illnesses.
• Early treatment and stabilization on medication greatly improves the
prognosis for people with schizophrenia. Many people can now, with timely and adequate treatment and support, live satisfactory lives in the community.
• Involuntary hospitalization of people who are too ill to care for themselves
should never be falsely equated with incarceration in the criminal justice system. To do so not only adds to outmoded stigma and prejudice about people with mental illness—it also deprives them of their fundamental right to proper medical treatment and care. Unfortunately, such confusion is common. As a result, there are already far too many people with severe and chronic brain diseases such as schizophrenia who have "fallen through the cracks" of the system and are abandoned, because they are not well enough to seek treatment for themselves.
• It is a scandal that people who are severely ill and for whom effective
treatment is available are literally dying in our streets from neglect. Furthermore, suicide rates among this population are alarmingly high. For example, 50% of all people with schizophrenia will attempt to commit suicide—and 10 to 13% will succeed.
• If we do not advocate for the essential right to treatment under the Mental
Health Act, this situation will worsen.
The purpose of the BC Mental Health Act is to help people who are suffering receive the medical treatment and care they need and deserve so that they can regain their health.
British Columbia Schizophrenia Society 41
EARLY PSYCHOSIS
EDUCATION RESOURCES
"Reaching Out The Importance of Early Treatment"
"Outstanding educational resource to teach senior high school students about mental illness." Connie Easton - Vice President, British Columbia School Counsellors Association
"Accurate information, good emphasis on early treatment useful to professionals dealing with young people." Dr. Bill MacEwan – Director, Schizophrenia Program, University of British Columbia Department of Psychiatry
• "Reaching Out" High School Curriculum Resource Kit
This important new tool consists of • 22-minute video • Teacher/ Facilitator's
Guide • Lesson Plans, Overheads • Student Materials. The "Reaching Out"
resource is designed to heighten awareness of the early signs and symptoms
of psychosis, and the importance of early intervention and treatment.
A complete, stand-alone resource that can be used by instructors who have
little or no previous knowledge of schizophrenia or other serious mental
illnesses.
Cost: Contact the BC Schizophrenia Society
• "Reaching Out" Video 22 minutes
Video emphasizes the importance of getting help early for someone showing early psychosis symptoms. Dramatic storyline intercut with interviews of people with schizophrenia talking about their illness. (This video is included in complete "Reaching Out" curriculum resource kit, above.)
• "Reaching Out" Video 12 minutes
Early Psychosis Identification for Physicians and Mental Health Professionals. Developed by the BC Schizophrenia Society in conjunction with the University of British Columbia's Department of Psychiatry to help enhance clinical skills. People with schizophrenia talk about their personal experience; commentary by five noted psychiatrists.
• Booklet - Early Psychosis: What Families and Friends Need to Know
38-page detailed booklet includes information on different types of psychosis, early warning signs, treatment, how to find appropriate medical help, education, rehab and recovery.
RESOURCE/VIDEO ORDER FORM
"Reaching Out: The Importance of Early Treatment"
(Order prices include all taxes, shipping & handling)
• "Reaching Out" Complete Curriculum Resource Kit
(Includes 22-minute video, with 80-page instructor's guide)
Cost
(Order procedure changed- please check with BCSS Provincial Office)
• "Reaching Out" 22-minute Video only
Cost
• "Reaching Out" 12-minute Video, Physicians' Version
Cost
• Booklet - Early Psychosis: What Families and Friends Need to Know
Cost
Number
$ 3.50
TOTAL COST:
CREDIT CARD: VISA MasterCard Expires _
Credit Card #
Name
Address
City Code _Country
Signature _
Cheques payable to BC Schizophrenia Society. Mail order form to:
BCSS Provincial Office, #201- 6011Westminster Highway, Richmond, BC V7C 4V4
(Canada) FAX Orders to: (604) 270-9861
TO ORDER BY PHONE: 604-270-7841or 1-888-888-0029
and charge to your Visa or MasterCard
British Columbia Schizophrenia Society 43
Source: http://www.focalpoint.org.au/files/issues-schizophrenia.pdf
DeMISTifying Deidentification of PHI in Free-formatted Text March 2016 Approved for Public Release; Distribution Unlimited. Case Number 16-0670 © 2016 The MITRE Corporation. All rights reserved. Introduction Tool Rationale MITRE Identification Scrubber Toolkit (MIST) Use Case 1 – Deidentification Hiding in Plain Sight Use Case 2 – Identification of PHI in e-mail Privacy Risk Identification and Management
Plaquette n° 22 13/02/09 9:32 Page 1 matriciels en implantologie. ➢ Gérard SCORTECCI1 La stimulation périostée par « needling » (Goldman a/ Quelle est la nature requise du traumatisme et Cohen, 1968) puis, plus tard, la stimulation induit - son calibre, sa morphologie - sa durée - son endostée par fraisage (Bert et coll. 1989), ont mon-