Kamagra gibt es auch als Kautabletten, die sich schneller auflösen als normale Pillen. Manche Patienten empfinden das als angenehmer. Wer sich informieren will, findet Hinweise unter kamagra kautabletten.
Papers
Neurosurgery
Issue: Volume 36(6), June 1995, p 1112–1117
Copyright: Copyright by the Congress of Neurological Surgeons
Publication Type: [Technique and Application]
ISSN: 0148-396X
Accession: 00006123-199506000-00007
Keywords: Dyskinesia, Morbidity, Pallidotomy, Parkinson's disease, Stereotaxy, Surgery
[Technique and Application]
Ventroposterior Medial Pallidotomy in Patients with Advanced Parkinson's Disease
Sutton, James P. M.D.; Couldwell, William M.D., Ph.D.; Lew, Mark F. M.D.; Mallory, Lou B.A.; Grafton, Scott M.D.; DeGiorgio, Christopher M.D.; Welsh, Mickie R.N., D.N.S.; Apuzzo, Michael L.J. M.D.;Ahmadi, Jamshid M.D.; Waters, Cheryl H. M.D.
Departments of Neurology (JPS, MFL, LM, SG, CD, MW, CHW), Neurological Surgery (WC, MLJA, JA), and Radiology (SG, JA), University of Southern California Medical School, Los Angeles, California
Reprint requests: Cheryl H. Waters, M.D., F.R.C.P.(C.), F.A.C.P., Associate Professor of Neurology, Chief, Division of Movement Disorders, University of Southern California, 1510 San Pablo Street, Suite
615, Los Angeles, CA 90033.
Received, August 8, 1994. Accepted, January 9, 1995.
IN A PRELIMINARY study, the effects of ventroposterior medial pallidotomy were evaluated in five patients with advanced Parkinson's
disease in whom medical therapy had failed. The mean age was 67.0 ± 5.6 years, and the mean Hoehn and Yahr stage when "off" was 3.9± 1.3. Three patients received unilateral pallidotomies; two of these received another pallidotomy after 8 weeks. Two other patientsreceived staged bilateral pallidotomies. No significant differences in overall function could be seen before and after the first surgicalprocedure. All three patients with peak-dose dyskinesias or dystonia had marked contralateral reduction in these symptoms.
Ventroposterior medial pallidotomy can ameliorate peak-dose dyskinesias in patients with advanced Parkinson's disease. Overall functionalimprovement is not remarkable.
There has been a renewed interest in the surgical treatment of Parkinson's disease. Recent reports on the results of ventroposterior
medial pallidotomy suggest a role for this procedure in moderately severe Parkinson's disease Because of theseinitially promising reports in patients with moderately severe disease, we undertook a pilot study to see if similar benefits could beobtained in patients with advanced, medically refractory Parkinson's disease. We report here the preliminary results of this procedure.
PATIENTS AND METHODS
Patient selection
All patients (n = 5) had advanced Parkinson's disease with disabling symptoms; their mean age was 67.0 ± 5.6 years, the mean disease
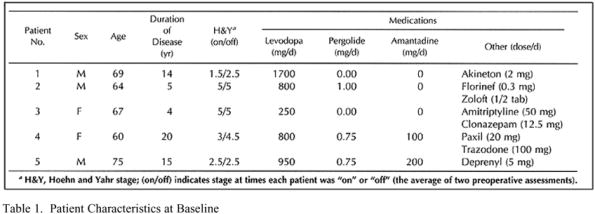
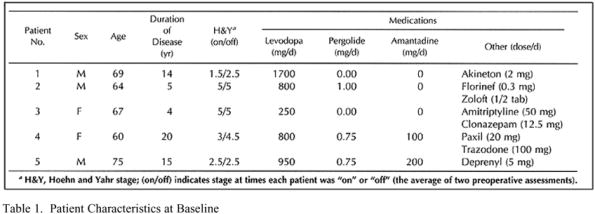
duration was 11.6 ± 6.9 years, and the mean Hoehn and Yahr stage when "off" was 3.9 ± 1.3 (the average of two preoperativeassessments). Previous medical therapy had failed in all patients, and most of the patients had severe motor fluctuations with peak-dosedyskinesias or dystonia. (See for baseline patient characteristics). All five patients had been treated by the investigators for atleast 6 months before enrollment in the study. The risks, the benefits, and the experimental nature of the procedure were outlined indetail for each patient, and their written informed consent was obtained according to the guidelines of our institutional review board.
Table 1. Patient Characteristics at Baseline
Patients were evaluated 2 weeks and 1 week before surgery, and 2, 4, and 8 weeks after each surgical procedure. On each test date,
the patients were first evaluated in a practically defined "off" state, with their last anti-parkinsonian medication taken at least 9 hoursbefore the assessment. Patients then took their usual morning dose of levodopa, dopamine agonists, and anticholinergic medications, andthey were again evaluated when "on." Assessments performed both on and off included a complete Unified Parkinson's Disease RatingScale (UPDRS) , Hoehn and Yahr staging , and the Schwab-England Activities of Daily Living scale (. Subscales were constructedfrom the individual items on the UPDRS to analyze akinesia, rigidity, and tremor, globally as well as on each side of the body. A FolsteinMini-Mental Status Examination and Hamilton Depression Inventory (were completed also at each visit.
Timed tasks
Timed tasks of motor performance were also performed in the off and on states, as described previously by Lindvall et al. (). These
included assessments of pronation-supination, hand opening and closing, fine finger movements, heel tapping, and gait.
Additional evaluations
Magnetic resonance imaging scans were obtained at baseline, within 1 week after surgery, and 4 weeks after each surgery.
Computerized visual fields were obtained before the first surgical procedure for three patients and after the last surgical procedure for allpatients. Patients were videotaped 1 week before and 4 weeks after all surgical procedures.
Surgical technique
Each patient underwent a unilateral pallidotomy as his or her initial surgical procedure. Patients 2 and 3 underwent repeated surgery
on the same side, because early improvement and subsequent relapse suggested that the initial lesions might have been too small in size.
Patients 1 and 4 had subsequent contralateral pallidotomies. Patient 5 had a single left pallidotomy.
For all procedures, target localizations were performed on the basis of the guidelines published by Laitinen et al. ( The
preoperative target was planned on thin-slice magnetic resonance imaging to choose the optimal lesion placement (medial globuspallidum). Each initial radiographic target was then chosen on intraoperative computed tomography (1-mm scan thickness), with the gantryparallel to the anterior commissural-posterior commissural (AC-PC) line. Targets were chosen 2 mm anterior, 19 to 22 mm lateral, and 5mm ventral to the AC-PC line. The Cosman-Roberts-Wells stereotactic instrument (Radionics, Inc., Burlington, MA) was used for theelectrode placement (). Patients received intravenous injections of propofol for sedation during the placement of the burr hole and thelesioning electrode. A single large burr hole was placed 2 cm lateral to the midline just posterior to the coronal suture, and the monopolarelectrode was inserted (Radionics, Inc.) (1.2-mm diameter tip with 2-mm uninsulated length). In each patient, ventriculography withIsovue M-200 dye helped to confirm the electrode placement. Several lesions were made for each procedure, inserting the electrodedeeper or withdrawing it by several millimeters; the final locations of the lesions depended on the patient's response to the electricalstimulation.
Intraoperative stimulation and lesioning protocol
For each potential lesion site, stimulation was first performed at low frequencies (23–5 Hz) and subsequently at higher frequencies
(typically 50 Hz), starting with low voltage and increasing the voltage slowly. We paid close attention to any indication that a patient hadvisual hallucinations of flashing lights, which suggested that the tip of the lesioning electrode was too close to the optic tract. We alsolooked for evidence of clonic, tonic, or dystonic movement of the extremities or face, and we assessed for possible changes in speech.
Then, a physiological, reversible "mock" lesion was made by heating the electrode tip to 42°C. In most cases, this accurately
predicted the response to the final anatomical lesion, and reversible improvement of contralateral rigidity and akinesia was noted.
A permanent anatomical lesion was made by heating the electrode tip to 72 to 80°C for up to 60 seconds. The electrode was moved in
2-mm increments, and the lesioning process was repeated to increase the overall lesion size. The total number of repetitions of thisprocess depended on the patient's clinical response.
In all cases, magnetic resonance imaging was used postoperatively to verify the size and location of the globus pallidum lesion. The
lesions were localized in three dimensions (x, y and z). Postoperative studies showed that all patients had lesions located between 17 and21 mm lateral to the midline (x) and that all but one patient had lesions between 1 and 3 mm anterior to the midpoint of the AC-PC line(y) (Patient 2's lesion was 5 mm anterior). The vertical extent of the lesions on postoperative studies (z) varied among patients, despitethe relatively uniform time of electrical lesioning among some patients in the group. The vertical extent of the lesions was specified as adistance, as the lesioning electrode was moved and multiple lesions were placed (mean, 15.2 mm). The vertical lesion lengths were asfollows: Patient 1, 4.5 mm, centered 4 mm below AC-PC line; Patient 2, 9.0 mm, centered 3 mm below the AC-PC line; Patient 3, 9 mm,centered 3 mm below the AC-PC line; Patient 4, 10.5 mm, centered 2 mm below the AC-PC line; and Patient 5, 4.5 mm, centered 3 mmbelow the AC-PC line. No significant differences were found between lesion location and outcome in these five patients.
CASE REPORTS
Patient 1
Patient 1, a 69-year-old, right-handed retired professor of political science, had first developed Parkinson's disease 14 years before
this surgery. His first symptoms consisted of gait difficulty and foot dystonia. He initially responded to levodopa, but, as his diseaseprogressed, he developed end-of-dose deterioration with bilateral foot dystonia, violent peak-dose dyskinesias, frequent falling caused byfreezing, and marked deterioration of his handwriting. Trials on pergolide and bromocriptine had failed; by the time of his first surgery,he was taking a total daily dose of 1700 mg levodopa.
The first surgery for Patient 1 was right-sided pallidotomy. During surgery and immediately after surgery, observers noted marked
improvement in left-sided foot dystonia, rigidity, and rapid alternating movements. No postoperative complications were noted during theweek after surgery, and he had improvement in akinesia, tremor, rigidity, and dystonia on the left side. He complained of worsenedspeech, but the results of the physical examination did not confirm this. Peak-dose dyskinesias were improved on the left; however, hisbalance worsened, and he continued to fall frequently. Because of this, he increased his levodopa dose to a total of 2100 mg daily. Onseveral occasions, he hit his head. Nine weeks after surgery a magnetic resonance imaging scan showed a substantial right convexitysubdural hematoma, which was drained without complication. Because his worsened balance seemed to be caused by persistent right-footdystonia and not to be a complication of his first surgery, he had a left-sided pallidotomy 11 weeks after the first pallidotomy and 2weeks after drainage of the subdural hematoma.
During the left-sided pallidotomy and immediately after that surgery, patient 1 showed marked improvement in contralateral
bradykinesia and motor tasks, and his voice was stronger. His gait did not improve significantly after the second surgery, although his rightfoot dystonia improved moderately. Speech was unequivocally improved; however, shortly after the second pallidotomy, he developed asevere clinical depression with suicidal ideation. His Hamilton Depression Inventory score rose from 8 before surgery to 17 after surgery.
Visual field testing 12 weeks after his second surgery revealed an incongruent left homonymous hemianopsis that had not been noted onroutine confrontation testing. He has increased his total daily dose of levodopa to 2500 mg and now finds it difficult to distinguish on andoff states. He falls frequently because of persistent, severe freezing.
Patient 3, a 67-year-old, left-handed former store manager, had had Parkinson's disease for 4 years. When she was receiving levodopa,
she developed peak-dose dystonic spasms of her left shoulder. By the time of surgery, she had profound left arm rigidity and haddeveloped a frozen left shoulder. She also had left arm resting tremor, marked global bradykinesia, and bilateral dystonic foot inversion;she could stand only with assistance.
First, a right-sided pallidotomy was performed. Immediately after surgery, there was a marked improvement in left arm akinesia and
rigidity. For the first 24 hours after surgery, a marked improvement in left arm mobility was observed; however, this early improvementdiminished by the second day and disappeared completely by the third day after surgery. Because of the clear, although temporary,benefit seen on the first day after surgery, a second procedure was planned to enlarge the original lesion and provide a more lastingresponse.
Eight weeks later, a second right-sided pallidotomy was performed. The first of four lesions produced marked improvement in left-
sided akinesia and rigidity, and subsequent lesions produced some additional incremental improvement. Finding that peak-dose dystonia ofthe left shoulder was drastically reduced over the next few months, the patient gradually increased her total daily levodopa dosage to1800 mg with a great subjective improvement in overall function. Objectively, there was a marked reduction in shoulder dystonia.
Patient 4, a 60-year-old, right-handed former secretary, had a 20-year history of Parkinson's disease and had been receiving levodopa
for most of that time. By the time of her surgery, she was having severe fluctuations with wearing-off and unpredictable off periods. Whenon, she would have disabling, violent peak-dose dyskinesias. Her Hoehn and Yahr off was Stage 4.5.
First, a right-sided pallidotomy was performed. Immediately after surgery, there was improved tone in the left arm and leg, with no
complications. Peak-dose dyskinesias were essentially abolished on the left side of her body. Her Hoehn and Yahr stage, when off,improved from her preoperative stage 4.5 to stage 3, her stage when on improved from her preoperative stage 3 to stage 2. By 4 weeksafter being discharged, she was doing much better. On time had increased, and off periods were shorter in duration and less frequent.
Pergolide was increased to 1.5 mg a day. Some akathisia persisted, however. By 8 weeks after surgery, persistent right-sided dyskinesiaswere throwing the patient off balance when on. Because of her excellent response to the initial pallidotomy, and because her residualright-sided dyskinesias appeared to be the main cause for her ongoing disability, she was scheduled for contralateral pallidotomy.
Second, a left-sided pallidotomy was performed. During surgery and immediately after surgery, there was a significant decrease in
tone in the right arm and leg. By the first postoperative day, there was a dramatic reduction in dyskinesia, and there appeared to beimprovement in speech. Transient blurred vision in the right eye was noted; subsequently, formal visual field testing revealed a newdeficit in the right superior quadrant. Depression was noted before she was discharged from the hospital, and, by 4 weeks after thesurgery, the patient's score on Item 3 of the UPDRS, an indication of depression, had worsened from a score of 1 to 4.
Parkinson Rating Scale (all patients)
No differences were seen between the preoperative and postoperative results in either the mean UPDRS scores, or any of the
traditional three subdivisions (mentation, activities of daily living [on or off], or motor examination [on or off]). Specific subscales wereconstructed to assess the following areas, both on and off: gait/posture, right-sided akinesia, left-sided akinesia, right-sided tremor, left-sided tremor, right-sided rigidity, and left-sided rigidity. Again, there were no differences between mean scores before and after surgery,either ipsilaterally or contralaterally. Timed tasks were normalized by taking the reciprocal of the time to complete a task, and additionalhemibody subscales were constructed. No significant differences were observed before or after surgery in any areas, nor were anydifferences seen in the mean Schwab and England disability scores (on or off), the mean Hoehn and Yahr stages (on or off), or the meanHamilton Depression Inventory scores (on or off) before and after unilateral pallidotomy.
Postoperative morbidity
Morbidity after unilateral ventroposterior medial pallidotomy included postoperative worsening of preexisting depression (n = 2), new
visual field defects detected only on formal testing (n = 2), increased gait freezing (n = 1), worsened speech (n = 1), possibly worsenedswallowing (n = 1), and transient facial weakness (n = 2). Both patients with depression had evidence of long-standing depression beforeany surgical intervention. Their depression may have been triggered by unmet expectations of surgery, rather than by any surgicallycreated structural lesion.
The improvement in dyskinesias in Patients 1 and 4 and the improvement in dystonia in Patient 3 are consistent with previous
reported experiences. Even in the years before levodopa was established as the standard treatment of Parkinson's disease, before theclinical syndrome of levodopa-induced peak-dose dyskinesias became endemic in the parkinsonian population, pallidotomy wasinvestigated in the treatment of other choreiform and hemiballistic movements, with documented efficacy ). More recently, otherinvestigations have confirmed the effectiveness of pallidotomy in ameliorating hyperkinetic choreiform movements (). Laitinen et al. (found a significant number of his patients had improvement in "dystonia/pain" and mentions that "pallidotomy had a very good effect oninvoluntary movement." More recently, others have confirmed the dramatic effect of pallidotomy on peak-dose dyskinesias ().
Microelectrode recording may allow better anatomical and physiological localization of the appropriate target, as well as more precise
definition of the boundary between the medial globus pallidus and the optic tract. Pallidotomy with microelectrode recording mighttherefore reduce the incidence of visual field deficits. Early reports from centers using this technique do not mention any field deficits,suggesting a possible advantage of this technique (). More significantly, a clearer definition of the boundaries between the medialglobus pallidus and either the optic tract or the internal capsule might allow a larger lesion to be created with a greater margin of safety,thus allowing for greater functional improvement.
Ventroposterolateral pallidotomy can reduce or abolish contralateral peak-dose dyskinesia or dystonia in selected patients with
Parkinson's disease. In at least one patient in the present study, we saw a dramatic improvement in the Hoehn and Yahr score, suggestingthat this procedure has great potential. However, the benefit varies among patients, and the risks include visual field deficits and possibledepression. The functional improvement in patients with advanced Parkinson's disease was not significant.
This project was supported in part by the National Parkinson Foundation (CW, JPS, MFL, LM, MW).
This research was presented in part at the 46th Annual Meeting of the American Academy of Neurology, Washington, DC, May 1994.
REFERENCES: ()
1. Baron M, Turner RS, Vitek JL, Kaneoke Y, Bakay RAE, DeLong MR: Lesions of the internal segment of the globus pallidus (GPi) in
parkinsonian patients improve motor performance bilaterally. Neurology 44[Suppl 2]:A304, 1994 (abstr).
3. Couldwell WT, Apuzzo MLJ: Initial experience related to the use of the Cosman-Roberts-Wells stereotactic instrument: Technical note. J
Neurosurg 72:145–148, 1990.
4. Fahn S, Elton RL, members of the UPDRS Development Committee: Unified Parkinson's Disease Rating Scale, in: Fahn S, Marsden CD,Calne DB, Goldstein M (eds): Recent Developments in Parkinson's Disease. Florham Park, Macmillan Health Care Information, 1987, vol 2,pp 153–164.
5. Fazzini E, Dogali M, Berich A, Eidelberg D, Gianutsos J, Stereo G, Perrine K, Loftus S, Chin L, Kolodny E: Unilateral ventral pallidotomy
in patients with Parkinson's disease: One-year follow-up. Neurology 44[Suppl 2]:A323, 1994 (abstr).
6. Folstein MF, Folstein SE, McHugh PR: Mini-Mental Status. A practical method for grading the cognitive state of patients for the clinician.
J Psychiatr Res 12:189–198, 1975.
7. Gioino GG, Dierssen G, Cooper IS: The effect of subcortical lesions on production and alleviation of hemiballic or hemichoreic
movements. J Neurol Sci 3:10–36, 1966.
9. Green J, Vitek JL, Baron M, Bakay RAE, DeLong MR: Neuropsychological sequelae of pallidotomy for treatment of Parkinson's disease
(PD). Neurology 44[Suppl 2]:A304, 1994 (abstr).
10. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62, 1960.
11. Hariz MI: Correlation between clinical outcome and size and site of the lesion in computed tomography guided thalamotomy and
pallidotomy. Stereotact Funct Neurosurg 54+55:172–185, 1990.
12. Hoehn MM, Yahr MD: Parkinsonism: Onset, progression, and mortality. Neurology 17:427–442, 1967.
13. Iacono RP, Lonser RR: Reversal of Parkinson's akinesia by pallidotomy. Lancet 343:418–419, 1994 (letter).
14. Laitinen LV, Bergenheim AT, Hariz MI: Leksell's posteroventral pallidotomy in the treatment of Parkinson's disease. J Neurosurg 76:53–
61, 1992.
15. Lindvall O, Widner H, Rehncrona S, Brundin P, Odin P, Gustavii B, Frackowiak R, Leenders KL, Sawle G, Rothwell JC, Björklund A,
Marsden CD: Transplantation of fetal dopamine neurons in Parkinson's disease: One-year clinical and neurophysiological observations in two
patients with putaminal implants. Ann Neurol 31:155–165, 1992.
16. Miyasaki JM, Lozano A, Duff J, Dostrovsky J, St. Cyr J, Lang AE: The role of posteroventral pallidotomy in advanced Parkinson's disease
(PD) and striatonigral degeneration (SND). Neurology 44[Suppl 2]:A322, 1994 (abstr).
17. Tsubokawa T, Moriyasu N: Lateral pallidotomy for relief of ballistic movements: Its basic evidences and clinical application. Confin
Neurol 37:10–15, 1975.
18. Vitek JL, Baron M, Kaneoke Y, Turner RS, Bakay RAE, DeLong MR: Microelectrode-guided pallidotomy is an effective treatment for
medically intractable Parkinson's disease. Neurology 44[Suppl 2]:A304, 1994 (abstr).
This article by Sutton et al. studies the effects of ventroposterior medial pallidotomy after nine procedures in patients with advanced
Parkinson's disease. The results of the procedure on many manifestations of the disease were not spectacular and were variable, as theauthors clearly show. In addition, patients with advanced Parkinson's disease do not do well with any type of ablative surgery.
Interestingly, the only objective improvement was on levodopa-induced dyskinesia.
Thalamotomy also decreases levodopa-induced dyskinesia, as has been established by the experience of many stereotactic surgeons.
However, one will not find much in the literature about this because the complications of thalamotomy in patients with advancedParkinson's disease are unacceptably high. In addition, bilateral thalamotomy procedures are unlikely to be considered in this group ofpatients because the risks for speech and gait abnormalities are unacceptable.
Ventroposterior medial pallidotomy may be more appropriate in less advanced bradykinetic patients who must take
levodopa/carbidopa for severe bradykinesia but are unable to do so because of severe, bilateral, drug-induced dyskinesia. The advantageof the pallidotomy procedure over thalamotomy is that complications for a staged bilateral pallidotomy are within acceptable levels. Theauthors, quite correctly, are distressed over the number of postoperative visual field deficits (usually an inferior quadranopsia, which canbe bothersome to a functional individual); I agree with the authors that incorporation of a microelectrode recording technique may reducethe incidence of this complication.
Patrick J. Kelly
New York, New York
The value of using ventroposterior medial pallidotomy for the relief of parkinsonian bradykinesia has grasped the imagination of the
neuroscientific community. Although the suggestion has been made that pallidotomy in a particular part of medial pallidum is particularlyeffective for the relief of bradykinesia, it seems to this observer that the lesions made are large enough to destroy most of the medialpallidum in the sagittal plane in which they are done. Such destruction would be at odds with the suggestion that the choice of aparticular portion of the medial pallidum in modern pallidotomy makes it more effective for the relief of bradykinesia than were standardpallidotomies done in the past. In fact, inspection of outcome data from the early years of stereotactic surgery suggests that there wasimprovement of a modest degree in bradykinetic features, improvement that would now be masked by levodopa therapy . Relief oflevodopa-induced dyskinesia by pallidotomy is, however, quite striking; such dyskinesia did not exist, of course, at the time thatpallidotomy was popular, and the degree of relief is clearly greater than that achieved by thalamotomy. It still remains to be determinedwhich features of parkinsonian bradykinesia are improved by pallidotomy and to what extent they are improved in the long term. Suchassessment may require a relatively large database because the degree of improvement is modest and possibly selective for certainaspects of bradykinesia.
Ronald R. Tasker
Toronto, Ontario, Canada
REFERENCES: ()
1. Riechert T: Long-term follow-up of results of stereotaxic treatment in extrapyramidal disorders. Confin Neurol 22:356–363, 1962.
The history of pallidotomy is replete with inconsistent results. The experience of Dr. Sutton et al. is typical of that of several centers
that have recently attempted posterior ventral pallidotomy. They have seen some improvements in parkinsonian symptoms but have givenup the procedure after inconsistent results and complications in a few patients.
In most instances, this repetition of history is a result of not being able to identify the optimal target, which appears to be the

sensorimotor segment of globus pallidus interna. Most of the time, the lesion is placed too anterior and is made too small. The transientimprovement from a too anterior lesion was first reported by Spiegel and Wycis (), who were able to improve their results by making asecond lesion more posteriorly. We use the same initial targeting procedure as the authors and are consistently off the ideal target (asdefined physiologically) by 2 mm in the x or y axis. We generally make two lesion tracts in the same parasagittal plane, 3 mm apart andequidistant from the optimal trajectory, in order to include all the adjacent sensorimotor area. In special cases, it may be necessary toinclude an additional lesion tract, either one more lateral for problems with the arm or one more medial for problems with the leg.
The use of microelectrodes can help in identifying the corticospinal tract and optic tract and theoretically could decrease the
complication rate. The sensorimotor area can be identified with true microelectrode recordings by virtue of the kinesthetic and tremor-associated neurons (). One additional aspect concerning the authors' lesions is the height of those lesions; the vertical extent of globuspallidus interna is between 4 and 7 mm. With the acute angle used by these authors, and the rather long vertical lesioning tracts, theglobus pallidus externa was undoubtedly included within the lesion. Experimental studies and our clinical investigations would suggest thatlesioning of globus pallidus externa might result in worsening of symptoms, especially if the lesion in the globus pallidus interna isincomplete. The lesion size, in part, is related to duration of heating; in several of these lesions, a time of 15, 20, or 30 seconds was used(personal communication), and this may be insufficient to produce a large enough lesion.
In order to maximize the symptomatic improvement by posterior ventral pallidotomy, our group believes that it is essential to define
completely the sensorimotor region of the globus pallidus interna and the lesion. Our results show significant improvement of all symptomsof Parkinson's disease, as well as of drug-induced dyskinesias. In no situation is this a cure, but the improvements in the activities of dailyliving can be substantial. Lesioning should be restricted to idiopathic Parkinson's as Parkinson-plus patients do not seem to be able to takeadvantage of the motoric improvement. A randomized clinical trial is under way at our institution to determine the effectiveness andsafety of posterior ventral pallidotomy.
Roy A.E. Bakay
Atlanta, Georgia
REFERENCES: ( 1. Spiegel EA, Wycis HT: Stereoencephalotomy. Part II: Clinical and Physiological Applications. New York, Grune & Stratton, 1962.
2. Vitek JL, Baron M, Kaneoke Y, Turner RS, Bakay RAE, DeLong MR: Microelectrode-guided pallidotomy is an effective treatment for
medically intractable Parkinson's disease. Neurology 44[Suppl 2]:A304, 1994 (abstr)
KEY WORDS: Dyskinesia; Morbidity; Pallidotomy; Parkinson's disease; Stereotaxy; Surgery
IMAGE GALLERY
Export Selected to PowerPoint
Copyright (c) 2000-2010
Version: OvidSP_UI03.03.01.103, SourceID 53860
Source: https://labs.psych.ucsb.edu/grafton/scott/Papers/Sutton1995Neurosurgery.pdf
Thermo Scientific Vanquish UHPLC System Revolutionize Your UHPLC Experience We feel that achieving better performance is not the same as spending more effort. We know that every breakthrough starts with a challenge. We want that challenge to be your science, not your instrument. Our mission is to let you find better answers, more answers, and get them faster. Make your life as a chromatographer easier by seeing what you couldn't see before and doing what you couldn't do before.
Indian Journal of Animal Reproduction 33 (1) : June 2012 REPRODUCTIVE PERFORMANCE DURING PARASITIC LOADS AND ITS CONTROL IN DOES DINESH MAHTO1, L.B.SINGH2, M.P.SINHA3, D.K.SINGH "DRON"4 AND D.K.JHA5 AICRP, on Black Bengal Goat, Department. of ABG, College of Veterinary Science and Animal Husbandry (BAU) Kanke, Ranchi-6 Jharkhand.(India)