Kamagra gibt es auch als Kautabletten, die sich schneller auflösen als normale Pillen. Manche Patienten empfinden das als angenehmer. Wer sich informieren will, findet Hinweise unter kamagra kautabletten.
Obgyn.med.wayne.edu
Management of Addiction Disorders in Pregnancy
Gary D. Helmbrecht, MD, FACOG, and Siva Thiagarajah, MD, FACOG
sion lead to fetal growth deficiencies, preterm labor, fetal
Abstract: In this article, we will review the prevalence of addiction
death in utero, and other pregnancy complications.
disorders in pregnancy and the impact that it has on perinatalmorbidity and mortality. We will then review effective screeningtechniques and propose a management scheme for achieving short-
HOW PREVALENT IS DRUG USE IN
term abstinence leading to the ultimate goal of long-term recovery.
The various medical and obstetric complications unique to this
Significant differences exist between men and women
patient population will be discussed as well as the specific adverse
who are affected by addiction disorders with respect to the
effects of substance abuse on placentation and the developing fetus.
emotional turmoil that leads to the substance abuse and the
Finally, medications proven efficacious in the treatment of addiction
psychologic factors that predispose them to become addicted.
disorders will be reviewed in the context of their use in the pregnant
Many women experience intolerable stress from lack of
social power.9 They are forced to conform to a stereotyped,
Key Words: pregnancy, pregnancy complications, fetus, newborn,
subordinate "sex role," which leads them to substance abuse.
addiction opiate dependence, substance dependence, alcohol depen-
These women receive the message in early life that they are
dence, cocaine, methamphetamine, human, review
less worthy because they are women. The women whosubsequently develop addiction disorders are then stigma-
(
J Addict Med 2008;2: 1–16)
tized more harshly by society because of their gender. Theyfrequently find themselves in abusive relationships and aremore likely than men to have been victims of childhood
Pregnancy presents unique challenges to the physician physical10 and sexual11,12 abuse. Kendler and colleagues12
caring for patients with addiction disorders. The negative
demonstrated in studies of female twins that a woman is 6
social stigma associated with addiction is amplified toward
times more likely to develop a drug addiction and 4 times
this population. As a consequence, pregnant women are
more likely to develop alcoholism if she was sexually abused
frequently demonized for abusing drugs. Indeed, many states
as a child. In twins discordant for sexual abuse, addiction
have criminalized this behavior, subjecting these patients to
disorders were consistently more prevalent in the abused
prosecution and incarceration without adequate treatment.1
sibling. Major depression seems to be a more frequent co-
Furthermore, obstetric care providers often lack the ability to
morbid antecedent diagnosis in women who develop addic-
effectively screen their patients for substance abuse,2,3 and
tion disorders than in men.13 The depression seems to be the
negative attitudes toward these patients frequently limit their
result of sex-specific genetic and environmental factors and
access to adequate prenatal care. Because of this negative
does not seem to arise from the same factors underlying
social stigma and the consequences thereof, many women
substance abuse disorders in men.
react with shame and attempt to conceal their drug use. The
Women also are more likely than men to abuse pre-
resultant perinatal morbidity and mortality rates are unaccept-
scription drugs.14,15 The most commonly abused medications
include benzodiazepines, hydrocodone bitartrate (Vicodin),
The role of illicit drug use in the transmission of human
and Fiorinal (Butalbitol, caffeine, and aspirin). Doctor shop-
immunodeficiency virus (HIV) is undisputed. The pregnant
ping is common and the abuse of medications is generally for
woman engaging in illicit drug use also is at risk for increased
self-treatment of comorbid conditions. This form of chemical
morbidity and mortality associated with other parallel high-
coping16 includes the use of prescription stimulants for
risk behaviors, including violence,8 transmission of hepatitis
weight control and opiates to overcome depression or other
B and hepatitis C viruses, and other sexually transmitted
forms of emotional pain.17
infections. Nutritional deficiencies, repeated episodes of
In the United States, men are more likely to use, abuse,
withdrawal, and direct drug effects on utero-placental perfu-
and be dependent on alcohol or illicit drugs than women.18 In2003, approximately 4% of married women aged 18 to 49
From the Prenatal Diagnosis Center, Charlottesville, VA.
years were dependent on or abusing alcohol or an illicit drug
Received July 17, 2007; accepted August 28, 2007.
compared with 11% of those who were divorced or separated
Send correspondence and reprint requests to Gary D. Helmbrecht, MD,
and 16% who had never been married. Among men in the
FACOG, Prenatal Diagnosis Center, 600 Peter Jefferson Parkway, Suite
same age range, 10% of those who were married were
190, Charlottesville, VA 22911. e-mail:
[email protected].
dependent on or abusing alcohol or an illicit drug compared
Copyright 2008 American Society of Addiction MedicineISSN: 1921-0629/08/0201-0001
with 23% of divorced or separated and 24% who had never
J Addict Med • Volume 2, Number 1, March 2008
Helmbrecht and Thiagarajah
J Addict Med • Volume 2, Number 1, March 2008
been married. However, comparable rates of alcohol, to-
have estimated that the prevalence of illicit drug use during
bacco, marijuana, cocaine, and heroin use are seen among
pregnancy varies from 0.4% to 27%.22–25
adolescents.19 These results are of particular concern in light
The NSDUH update on substance abuse showed a
of the finding by Greenfield and colleagues20 that women
decline in use of illicit drugs, alcohol, and tobacco during
have a heightened vulnerability to the physical, mental, and
pregnancy (Fig. 2). This finding suggests that although
social consequences of substance use.
women did not discontinue their dependence completely
Currently, women have an estimated lifetime preva-
during pregnancy, this may be an invaluable opportunity to
lence of 17.9% and a 12-month prevalence of 6.6% for any
screen, educate, and refer these patients for treatment.
substance abuse disorder (excluding nicotine dependence).19Epidemiologic studies on the prevalence of specific drug use in
SCREENING FOR SUBSTANCE ABUSE
pregnancy are lacking; however, some studies have reported on
DISORDERS IN PREGNANT WOMEN
the overall frequency of illicit drug use in pregnancy. The
Most obstetric care providers fail to adequately screen
National Study on Drug Use and Health (NSDUH) is a
their patients for substance abuse disorders.2 This stems from
continuation of the National Household Survey on Drug
a multitude of reasons, the most prevalent of which include:
Abuse. The update for 2002 and 2003 on substance abuse in
1) refusal to accept addiction as a disease; 2) lack of knowl-
pregnancy21 demonstrated that 4.3% of pregnant women aged
edge of treatment options; 3) disbelief that substance abuse
15 to 44 years had used an illicit drug during the past month
disorders are prevalent among their patients; 4) reservations
compared with 10.4% of nonpregnant women in the same age
about the efficacy of treatment programs; and 5) concern
category (Fig. 1). The prevalence of substance abuse was
about liability should a substance abuse disorder be identi-
highest among nonpregnant white women. Among the preg-
fied. This last reason is a major obstacle. An act of omission
nant women, past month illicit drug use was greatest in the
(failure to refer for appropriate treatment) may be cause for
African American population. Substance abuse was lowest in
civil legal action should the pregnancy outcome be less than
both pregnant and nonpregnant Hispanic women.
perfect. Furthermore, many states have mandatory reporting
In women who had delivered within the previous 12
requirements when a substance abuse disorder is identified.
months, the rates of past month illicit drug use was lower than
Failure to comply can result in penalties ranging from mon-
among the other nonpregnant women (8.4% vs. 10.6%). It
etary fines to disciplinary action against their medical license.
remained higher than in the pregnant group (4.3%). Although
It is the physician's responsibility to be aware of the reporting
this was a cross-sectional study, these data at least suggest
requirements in his/her respective state and remain in com-
that reproductive-aged women tend to increase their sub-
pliance with the law. In Virginia, no specific law requires
stance use during the year after giving birth. In this study,
reporting a pregnant woman with a substance abuse disorder;
younger pregnant women, those aged 15 to 25 years, were
however, all licensed practitioners must, as a routine compo-
more likely to have used an illicit drug during the past month
nent of prenatal care, establish and implement a medical
than older women, aged 26 to 44 years. Other studies utilizing
history protocol to
screen all pregnant patients for substance
various methods, including neonatal meconium testing, urine
abuse to determine the need for further evaluation. To pre-
toxicology at the initial prenatal visit, and patient interviews,
serve the trust between patient and physician, the results of
FIGURE 1.
Percentages of past-month illicit drug use
FIGURE 2.
Percentages among women aged 15 to 44
among women aged 15 to 44 years by pregnancy status,
years who reported past-month substance use by pregnancy
age, and race/ethnicity. From the Office of Applied Studies,
and recent motherhood status: 2002 and 2003. From the
Office of Applied Studies.
2008 American Society of Addiction Medicine
J Addict Med • Volume 2, Number 1, March 2008
Addiction Disorders in Pregnancy
the medical history screen and/or substance abuse evaluation
Thus, a clinical profile can be developed identifying
may not be admissible in any criminal proceeding (§54.1-
those at highest risk for substance abuse during pregnancy.
2403.1 of the Code of Virginia). Unfortunately, this statute is
The clinical characteristics and the associated relative risk for
largely unenforceable and most obstetric care providers are
substance abuse are shown in Table 1. Those women deemed
unaware of the law. The reporting requirements are more
at high risk for substance abuse should then be referred for a
stringent for the pediatric care providers. Section §63.2-1509
comprehensive assessment by a multidisciplinary team
of the Code of Virginia requires that attending physicians
trained to identify substance abuse disorders. This should be
report to local social services departments, or the Child
done as a second-level procedure outside the primary or
Abuse and Neglect Agency, all newborns medically diag-
obstetric care provider's facility and include an in-depth
nosed for exposure to alcohol or nonprescription drugs during
evaluation addressing not only the substance abuse but the
pregnancy. Failure to report could result in criminal liability
personal and psychosocial issues that would otherwise com-
punishable as a misdemeanor with an imposed fine. One of the
plicate the pregnancy. It is unrealistic to assume successful
roles of addiction medicine physicians is to educate the health
intervention for substance abuse without having adequate
care providers in their local communities on the disease model
services to assist the patient in dealing with the legal, finan-
of addiction, reporting requirements, and the various screening
cial, and psychosocial consequences of drug use. Such pro-
grams are available in most communities through the depart-
For screening to be effective, the procedure should be
ments of social services but are underutilized by obstetric
brief and simple to incorporate into daily clinical practice.
care providers. It is incumbent upon the addiction specialist,
The attitude of the interviewer is more important than the
therefore, to assist in the identification of these patients and
specific questions being asked. A woman with an addiction
make the appropriate referrals. Admission to residential or
disorder will immediately take note of any judgmental tone or
intensive outpatient treatment has been demonstrated to be
affect in the health care provider, and her guilt and shame
cost-effective and result in improved outcomes for the mother
regarding drug or alcohol use will cause her to deny or refuse
and fetus. Svikis and colleagues29 demonstrated higher birth
to disclose her history. Also, it is best to begin the process
weights and higher gestational age at delivery and reduced
with questions perceived to be less threatening to the patient,
rates neonatal ICU admissions in women who were engaged
such as questions about family history of substance abuse.
in a multidisciplinary treatment program at the time of deliv-
The more pointed questions should be reserved for later in the
ery compared with those who were not in treatment. They
interview after a rapport has been developed with the patient.
also showed an overall cost savings of $4644 per mother–infant pair. Finally, as with any chronic disease, a long-term,
Patients who have multiple risk factors for substance abuse
evidence-based, medical management model is needed to
should draw particular attention. Studies have identified sev-
ensure the highest likelihood for sustained recovery.
eral risk factors associated with perinatal substance abuse.
These include depression,13,26 childhood sexual abuse,11,12homelessness,26,27 family history of substance abuse,28 inad-
equate social support,26 past use of alcohol and tobacco,3 and
Both the use of illicit drugs during pregnancy and the
age.21 Chasnoff and collegues25 applied this technique in their
associated high-risk behaviors contribute to medical compli-
study of 2002 pregnant women from 9 prenatal clinics in
cations. Table 2 lists the complications seen with increased
South Carolina and Washington state. They found that
frequency in gravidas with addiction disorders.
women who drank in the month before pregnancy were
Anemia is common to all pregnancies. As part of the
approximately 41 times more likely to currently use drugs or
normal physiologic response to pregnancy, blood volume
alcohol or both than women who had never drank alcohol.
increases by 50%, whereas red cell mass increases by only
They also were approximately 5 times more likely to cur-
30%. Therefore, a mild anemia with normal red cell indices
rently use drugs or alcohol or both than women who did not
is expected and is referred to as "dilutional" anemia. This, of
use alcohol in the month before pregnancy but who had used
course, requires no further evaluation. Severe anemia (Hgb
alcohol in the past. Similarly, women who smoked in the
⬍ 9, Hct ⬍28) with abnormal red cell indices does require a
month before pregnancy were approximately 9 times more
workup. Microcytic anemia may be nutritional (iron-defi-
likely to currently use drugs or alcohol or both than women
ciency) in nature or may indicate the presence of an hemo-
who had never smoked. They were approximately 2 times
globinopathy. Macrocytic indices suggest a B
more likely to currently use drugs or alcohol or both than
women who did not smoke in the month before pregnancy but
It should be noted that in patients who are HIV-
who had smoked in the past. They found that the majority of
positive, anemia has a significant impact on the clinical
current substance abusers could be identified by asking 3
outcomes of quality of life and overall prognosis.30 In these
simple questions at the prenatal visit:
patients, anemia has been shown to be a statistically signifi-cant predictor of progression to the acquired immunodefi-
1. Have you ever drank alcohol?
ciency syndrome and is independently associated with an
2. How much alcohol did you drink in the month before
increased risk of death. Treatment of anemia with epoetin-
alpha31 has resulted in a significant reduction in the numbers
3. How many cigarettes did you smoke in the month
of patients requiring transfusions and the mean number of
before your pregnancy?
units of blood transfused. Resolution of anemia has resulted
2008 American Society of Addiction Medicine
Helmbrecht and Thiagarajah
J Addict Med • Volume 2, Number 1, March 2008
Factors Correlated with Alcohol or Drug Use During Pregnancy
Adjusted Odds Ratio
Alcohol or Drug Use
Drug Use Only
Ever smoked cigarettes
Ever drank alcohol
Ever drank alcohol and ever smoked cigarettes
Smoked cigarettes during month before
Drank alcohol during month before pregnancy
Another adult in household uses illicit drugs or
substantial alcohol
Another adult in household has been in
treatment for drug or alcohol abuse
Moderate or severe depression
Occasionally has crying spells (during past
Occasionally felt blue (during past week)
Has a child who lives in another household
Lives alone or with small children
Homeless during past 3 years
No usual source of health care
Worried about pregnancy
Sample size is 1949.
*Significantly different from 1 at
P ⫽ 0.01 level, 2-tailed test.
†Significantly different from 1 at
P ⫽ 0.05 level, 2-tailed test.
Reprinted with permission from
Am J Obstet Gynecol. 2001;184:752–758.
in improved quality of life, physical functioning, energy,
about an increased risk of congenital cardiac malformations
and fatigue in individuals with HIV.30 More recently, the
(atrial and ventricular septal defects) associated with first
use of highly active antiretroviral therapy (HAART) has
trimester exposure to the SSRI paroxetine (Paxil).38 The U.S.
been associated with a significant increase in hemoglobin
Food and Drug Administration in 2005 issued a public health
concentrations and a decrease in the prevalence of anemia.32
advisory regarding the use of paroxetine during pregnancy,
Combination therapy, including (HAART), seems to be safe
and the manufacturer changed paroxetine's pregnancy cate-
to use at any time during pregnancy.33 Pregnancy per se has
gory from C to D.39 Late-term use of SSRIs has been
no detrimental influence on the progression of HIV nor does
associated with neonatal abstinence syndrome (NAS).40,41
it affect the response to treatment.
Other pregnancy complications include low birth weight,
There is a strong relationship between depression and
fetal death, neonatal seizures, preterm birth,35 and persistent
substance abuse. Therefore, it is not surprising that one might
pulmonary hypertension.42 Although these adverse outcomes
encounter depression with increased frequency when caring
have been reported in association with a wide variety of SSRIs,
for pregnancies complicated by addiction disorders. Indeed,
the relationship seems to be strongest with paroxetine.41,42
substance abuse, violence, and depression are so closely
The American College of Obstetricians and Gynecolo-
interrelated in this population that the prenatal patient who
gists have published a Committee Opinion43 recommending
gives a history of any one of these should be carefully
that treatment with all SSRIs or selective norepinephrine
evaluated for the presence of the other two.34
reuptake inhibitors or both during pregnancy be individual-
Since the introduction of selective serotonin reuptake
ized and, if possible, paroxetine use among pregnant women
inhibitors (SSRI) into clinical practice, their use has become
or women planning to become pregnant be avoided. Any
widespread in pregnant women. Recently, concern regarding
woman exposed to paroxitine during the first trimester should
the safety of these agents has arisen. Although several inves-
be referred for a fetal echocardiogram. Initiation or continuation
tigators have failed to find an increased risk of major con-
of an SSRI during pregnancy should be done only after carefully
genital malformations associated with the use of SSRIs dur-
weighing the risks and benefits and with well-documented,
ing pregnancy,35–37 GlaxoSmithKline described 2 recent
informed consent. Given the high risk for relapse in gravidas
unpublished reports from a Swedish national registry and a
with addiction disorders and comorbid depression, the use of
U.S. insurance claims database that have raised concerns
an SSRI may well be justified. Although data are lacking at
2008 American Society of Addiction Medicine
J Addict Med • Volume 2, Number 1, March 2008
Addiction Disorders in Pregnancy
randomized trials are needed before elective cesarean deliv-
Medical Complications Common to Pregnancy
ery can be advocated to prevent vertical transmission of
and Substance Abuse
HCV. However, all published reports to date indicate there is
no evidence to suggest that breastfeeding is a mode of
transmission. The American Academy of Pediatricians and
the Centers for Disease Control support breastfeeding in these
women; however, it may be prudent for mothers who are
HCV-infected and who choose to breastfeed to consider abstain-
Gestational diabetes
ing from breastfeeding if their nipples are cracked and bleeding.
Hepatitis (chronic and acute)
Obstetric complications seen as a consequence of con-
tinued illicit drug use can occur slowly over time, as in the
Gingivitis/poor oral hygiene
development of fetal growth restriction, or can be abrupt in
Sexually transmitted diseases
onset, quite spectacular, and immediately life-threatening, as
with severe placental abruptions or acute myocardial infarc-
tions resulting from cocaine abuse. In some cases, the effects
Condyloma accuminata
on the fetus are not seen until early childhood when devel-
opmental and cognitive delays are noticed as a potential
consequence of benzodiazepine exposure.52 Prevention of
these complications requires close communication between
the addiction medicine physician, the obstetric care provider,
and the maternal-fetal medicine consultant. Lack of compli-
ance or relapse should be reported by the addictionist and thepatient should be brought in for fetal testing. It is our practiceat the same time to immediately increase the treatment level
this time, one should consider weaning the SSRI late in the
in these patients. We also report normal fetal testing and
third trimester in an attempt to mitigate the severity of NAS.
continued compliance to all care providers. Jones and col-
Because the medication is excreted in breast milk, breastfeed-
leagues53 have shown that compliance in treatment is im-
ing may contribute to a decrease in the observed NAS.44 The
proved by providing positive reinforcement in the form of an
highest risk of reemergence of depression occurs during the
escalating voucher system. We also use positive reinforce-
immediate postpartum period. If the SSRI was discontinued
ment as a technique to maintain compliance.
during the pregnancy, it should be restarted on the first
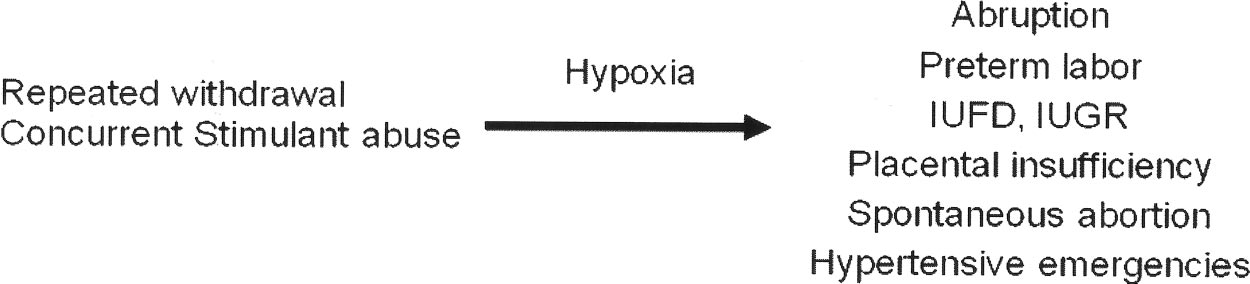
The major obstetric complications addressed are listed
postpartum day. All patients should be closely followed in the
in Table 3. They can be further subdivided by 1 of 2
weeks after delivery and adjunctive therapy added if and
antecedent pathophysiologic events: hypoxia or inflammation
when necessary.
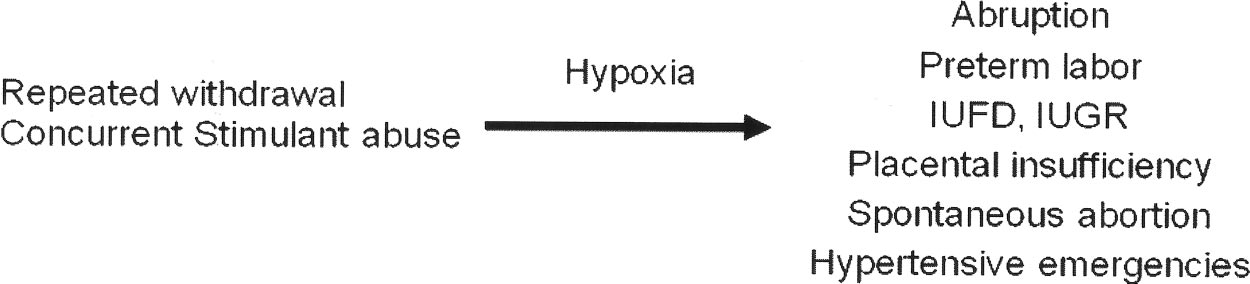
(Figs. 3 and 4). Events leading to hypoxia within the uterine
The infectious complications encountered in pregnancy
environment are those that adversely affect perfusion of the
are largely the result of parallel high-risk behaviors and can
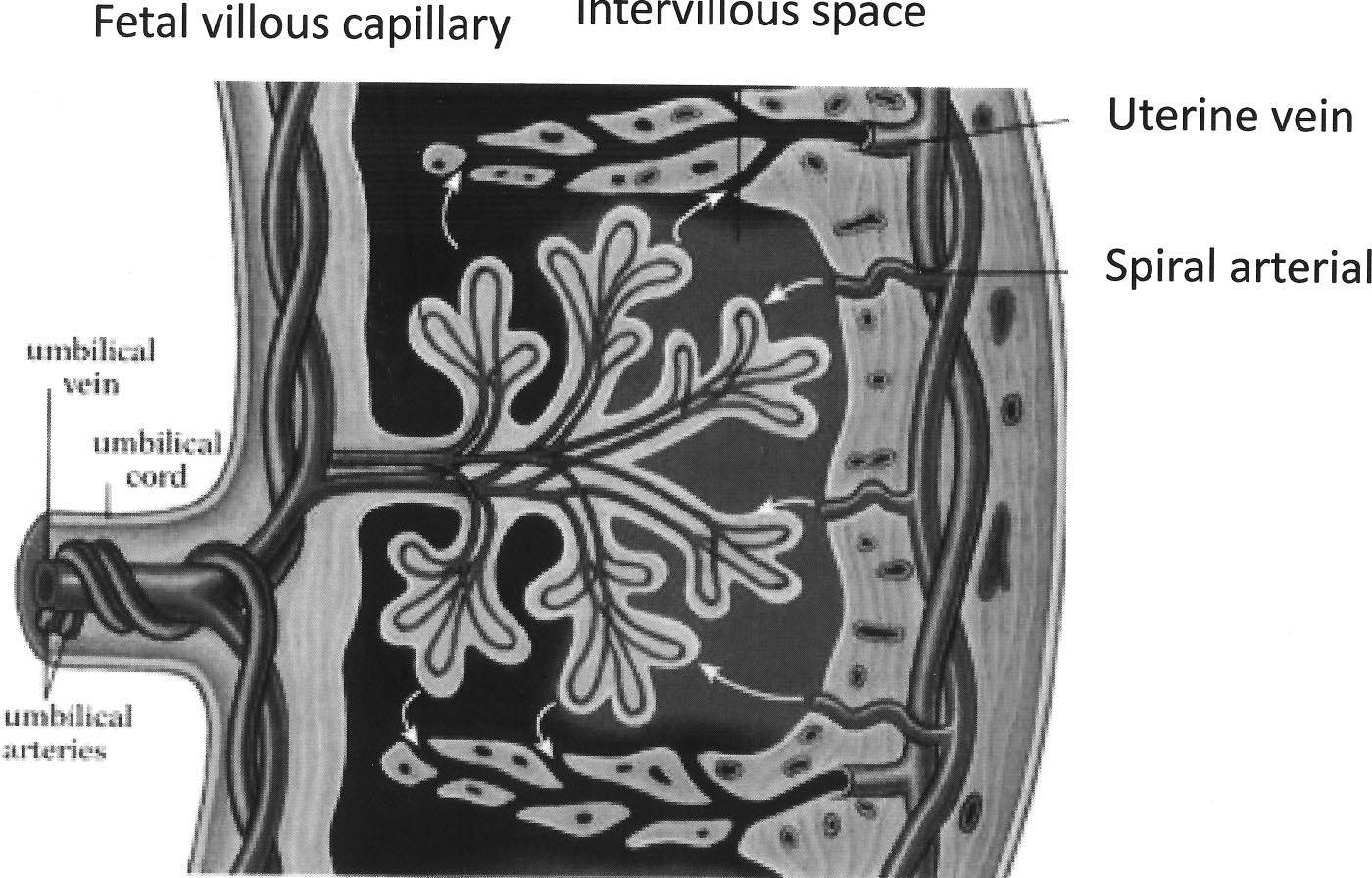
placenta by the uterine artery. Figure 5 is a schematic repre-
be minimized by control of the addiction and intense psycho-
sentation of a placental unit. Oxygenated, nutrient-rich blood
social support. Sexually transmitted diseases are common
enters the intervillous space through the spiral arterioles
because the women prostitute themselves for drugs or other-
branching off the uterine artery. Oxygen and nutrients diffuse
wise engage in sex with multiple partners. Intravenous drugusers are at particularly high risk for hepatitis and HIV. Theaddiction specialist needs to know that, although obstetric
Obstetric Complications in Gravidas with
care providers routinely test for hepatitis B, HCV is not a part
Addiction Disorders
of a routine prenatal laboratory panel. All patients with
Placental abruption
addiction disorders should be tested for HCV as well. If
positive, referral to a hepatologist is indicated. However,
Placental insufficiency
treatment should be deferred until after pregnancy because
Intrauterine growth restriction
liver biopsy is potentially hazardous during gestation and the
Hypoxic/ischemic brain injury
medical treatments are contraindicated during the pregnancy.
Liver function tests should be followed closely.
Neonatal abstinence syndrome
Vertical transmission of HCV to the fetus is relatively
Spontaneous abortion
inefficient (2.4-7%)45–47 but is significantly enhanced in
Intrauterine fetal death
women coinfected with HIV.46 Cesarean delivery does not
Premature labor and delivery
seem to be protective47,48; however, disagreement is seen in
Preterm, premature rupture of membranes
the contemporary literature.49,50 A recent review in the Co-
Postpartum hemorrhage
chrane Database51 suggests that the available data are insuf-
ficient to comment on this issue. In short, more prospective,
2008 American Society of Addiction Medicine
Helmbrecht and Thiagarajah
J Addict Med • Volume 2, Number 1, March 2008
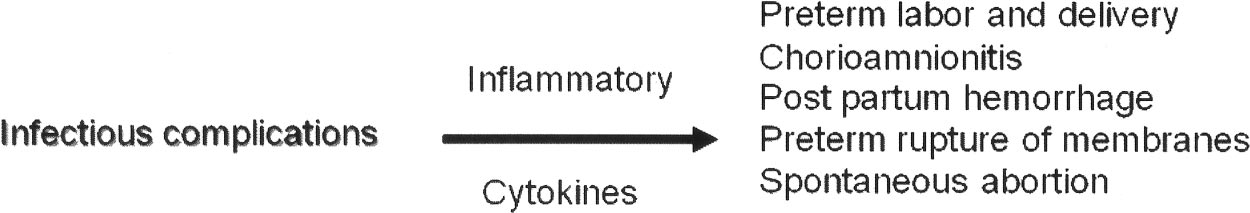
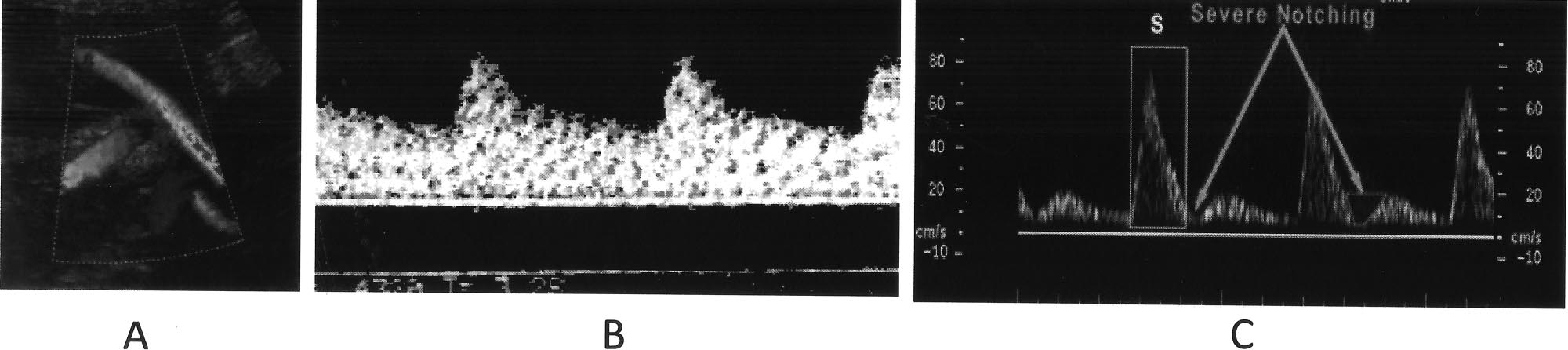
FIGURE 3.
Hypoxia-mediated pregnancy complications.
across the villous membrane into the villous capillaries and
ized rats, this effect seemed to be unrelated to the hemody-
travel to the fetus. Metabolic and respiratory waste is passed
namic response or pharmacokinetic profile of cocaine. Fur-
in the opposite direction into the maternal circulation. When
thermore, in vitro studies of human myometrial cells have
maternal perfusion of the uterus is interrupted or severely
demonstrated that cocaine increases myometrial contractions
curtailed, portions of the placenta can undergo separation
by both adrenergic and nonadrenergic mechanisms.60,61
from the uterus (abruption) or hypoxic death (infarction).
The increased autonomic response to withdrawal from
These are demonstrated in Figures 6 and 7, respectively.
opiates,62 benzodiazepines, and alcohol63 has long been
Placental abruption has many causes and complicates
known. Using Doppler velocimetry, maternal cigarette smok-
approximately 1% of pregnancies.54 Risk factors for abrup-
ing has been demonstrated to cause chronically increased
tion include previous abruption, smoking, trauma, cocaine
resistances in the maternal uterine, umbilical, and fetal mid-
use, multifetal gestation, hypertension, preeclampsia, throm-
dle cerebral arteries.64,65 In an earlier study by Koss and
bophilias, advanced maternal age, preterm premature rupture
colleagues,66 patients in the second and third trimesters of
of the membranes, and polyhydramnios. The strongest asso-
pregnancy had their uterine artery blood flow measured by
ciations have been demonstrated in patients with chronic
Doppler before, during, and for several minutes after the
hypertension and superimposed preeclampsia (odds ratio
smoking of a standard cigarette. During smoking, there was a
[OR],55 2.8 –3.8), cocaine or other stimulant use (OR,
velocity reduction within the uterine artery in all subjects.
5–10),56 and tobacco use (OR, 1.6 –2.1).57 An abruption can
The degree and duration of the reduction in blood flow
result in massive hemorrhage with fetal and/or maternal
varied. In most subjects the velocities were approximately
death. Lesser degrees of abruption can be less spectacular but
50% of baseline, but a reduction to almost zero was seen in
render significant portions of the placenta nonfunctional for
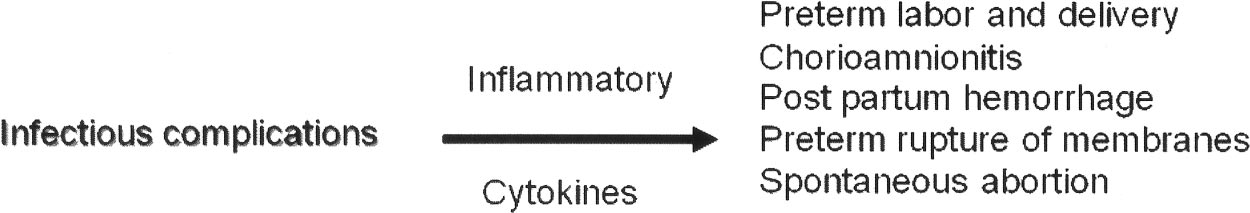
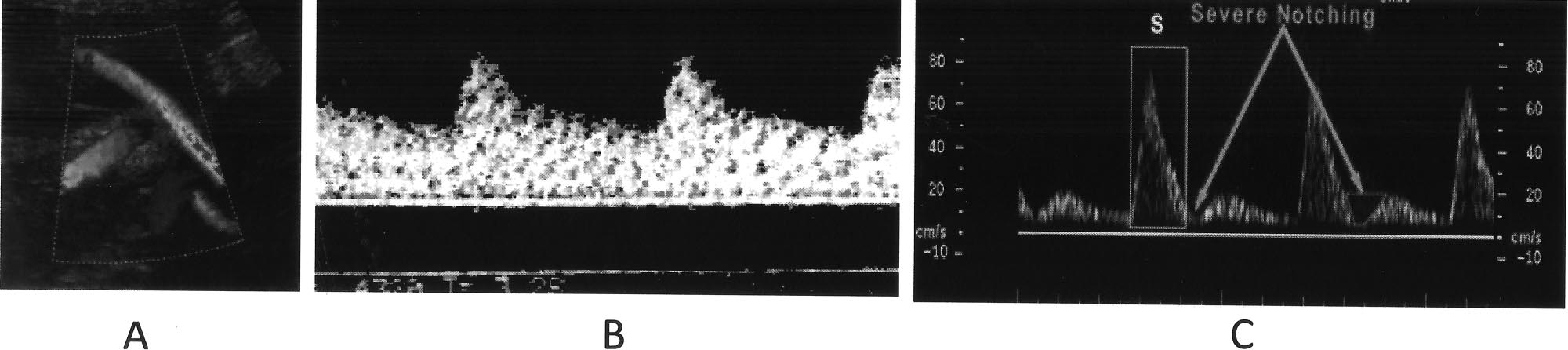
several subjects. Figure 8 shows sample uterine artery Dopp-
the remainder of the pregnancy, thereby limiting fetal access
ler flow wave forms from a normal pregnancy (A) at 32
to oxygen and nutrients. Similarly, placental infarctions can
weeks and an opiate-dependent patient (C) at 34 weeks in
result in fetal demise when ⬎50% of the placental mass is
moderate withdrawal. This latter patient was noncompliant
lost or be clinically insignificant when ⬍ 10% of the placental
with treatment and experienced multiple episodes of with-
mass is involved. Any sublethal insult to the placenta—
drawal throughout the pregnancy. She delivered a growth-
abruption or infarction—that limits nutrient and oxygen de-
restricted fetus, and the placental pathology confirmed mul-
livery to the fetus has the potential to limit the fetus' growth.
tiple infarctions throughout the parenchyma.
Furthermore, in an environment of chronic hypoxemia, brain
Many of the infectious complications of pregnancy in
development can be compromised, leading to hypoxic-isch-
addicted gravidas lead to inflammatory changes within the
emic brain injury.
uterine decidual tissue and amniotic fluid, which cause in-
Although the precise mechanism by which hypoxia can
creased amounts of interleukin-8, interleukin-6,67,68 tumor
occur in the uteroplacental environment is not known, one
necrosis factor ␣,69 and other inflammatory cytokines. These
possible way is via direct or catecholamine-induced uterine
activate production of prostaglandins, metalloprotease, and
artery spasm. Although the direct effects of stimulants on
collagenase enzymes, all of which contribute to premature
uterine artery flow in pregnancy have not been studied,
uterine contractions and digestion of the fetal membranes.
cocaine and methamphetamine are strongly catecolaminergic
Alternatively, the cytokines and prostaglandins produced
agents and side effects of use include hypertension and
in the decudual cells can cause preterm contractions and
tachycardia. Studies on the effects of cocaine on the gravid
cervical effacement with premature labor as the result. Fi-
myometrial cell have demonstrated inhibition of neuronal
nally, decidual enzyme production may dominate the process,
catecholamine reuptake in the gravid uterus.58 In an animal
resulting in membrane digestion and amniorrhexis. Once
model, cocaine has been shown to have a direct effect on
bacteria gain access to the decidual tissue, a transmembrane
enhancing myometrial contractility.59 In chronically catheter-
migration of the organisms will result in chorioamnionitis.
FIGURE 4.
Inflammatory cytokine-mediated pregnancy complications.
2008 American Society of Addiction Medicine
J Addict Med • Volume 2, Number 1, March 2008
Addiction Disorders in Pregnancy
FIGURE 5.
Schematic drawing of placental circulation.
These patients will present with fever, uterine tenderness, and
There must be sound scientific evidence to support its use.
contractions. If not promptly treated with antibiotics and
Evidence of widespread use and support from another qual-
delivery, the infection will progress to sepsis and septic shock
ified clinician are methods of justifying off-label prescribing.
and death may ensue.
An informed consent discussion must be conducted, notifying
Evidence that drugs of abuse acting through multiple
the patient of the potential risks, anticipated benefits, and
mechanisms (direct, hypoxemia, and inflammatory) result in
alternatives to treatment. Finally, legible documentation of
uterine contractions, cervical dilation, and membrane diges-
these discussions in the medical records is important.
tion is supported by the observation that these patients presentwith advanced cervical dilatation at admission and a shorter
latency period to labor and delivery.70 Further investigations
Alcohol is a known teratogen that causes a constellation
of potential indirect mechanisms of action of drugs of abuse
of malformations, including microcephaly, growth defi-
are needed, including altered prostaglandin production, inhi-
ciency, central nervous system dysfunction, including mental
bition of beta-adrenergic response, and direct effects on
retardation and behavioral abnormalities, and craniofacial
intracellular calcium mobilization for a more complete un-
abnormalities.72 Children born with the Fetal Alcohol Spec-
derstanding of the clinical ramifications of drug use during
trum Disorder will have lifelong, serious disability. Whether
medical treatment during pregnancy can prevent this devas-tating outcome remains to be proven. It is incumbent upon the
MEDICAL TREATMENT OF ADDICTION
physician caring for these patients to carefully weigh the risks
of the medication intended to maintain abstinence against the
In recent years, major advances have been made with
likelihood of continued alcohol use. The decision of whether
respect to medical treatment of addiction disorders. The
to treat is based on the risk benefit analysis.
numbers of medications being made available is unprece-
Benzodiazepines remain the treatment of choice for
dented. Still, obstacles to delivery of these medications to
detoxification during pregnancy. These agents interact with
reproductive-age women exist, not the least of which is the
the gamma-aminobutyric acid-A (GABA) receptor, which
reluctance of the pharmaceutical industry to perform clinical
mediates an increase in inhibitory neurotransmission that
trials on this population. The little information that is avail-
counteracts the excitatory state of the brain in alcohol with-
able on the use of these agents in pregnancy is in the form of
drawal. There is some evidence that women may have a
case reports or small case series. Taken with the liability
greater response to benzodiazepines than men,73 allowing for
issues, women who may become pregnant or those who are
reduced dosages. Carbamazepine has been used extensively
pregnant often are denied treatment despite the "greater
in Europe for detoxification from alcohol. Several small
harm" of continued drug or alcohol use on the developing
studies have demonstrated that this agent is most likely as
fetus. There are currently no medications approved by the
safe and efficacious as the benzodiazepines.74,75 It has the
FDA for treatment of addiction disorders during pregnancy.
advantage of having no abuse potential, and it has been
This does not prevent the practitioner from using a medica-
widely used in pregnancy for seizure disorders.
tion "off label" but certain requirements must be met.71 The
However, both agents have been associated with ad-
patient must meet the diagnostic criteria for dependence.
verse pregnancy outcomes. Despite early reports of facial
2008 American Society of Addiction Medicine
Helmbrecht and Thiagarajah
J Addict Med • Volume 2, Number 1, March 2008
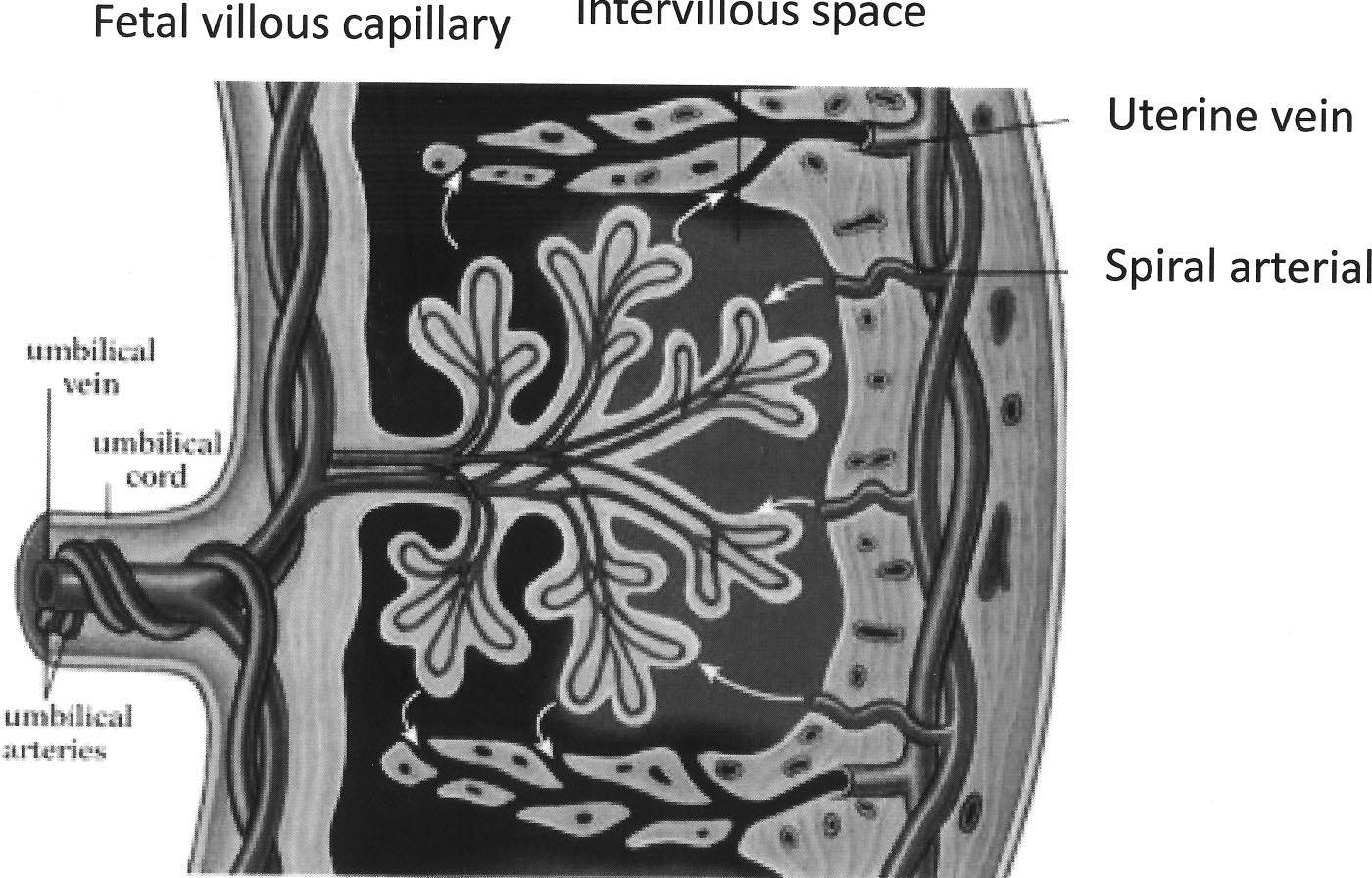
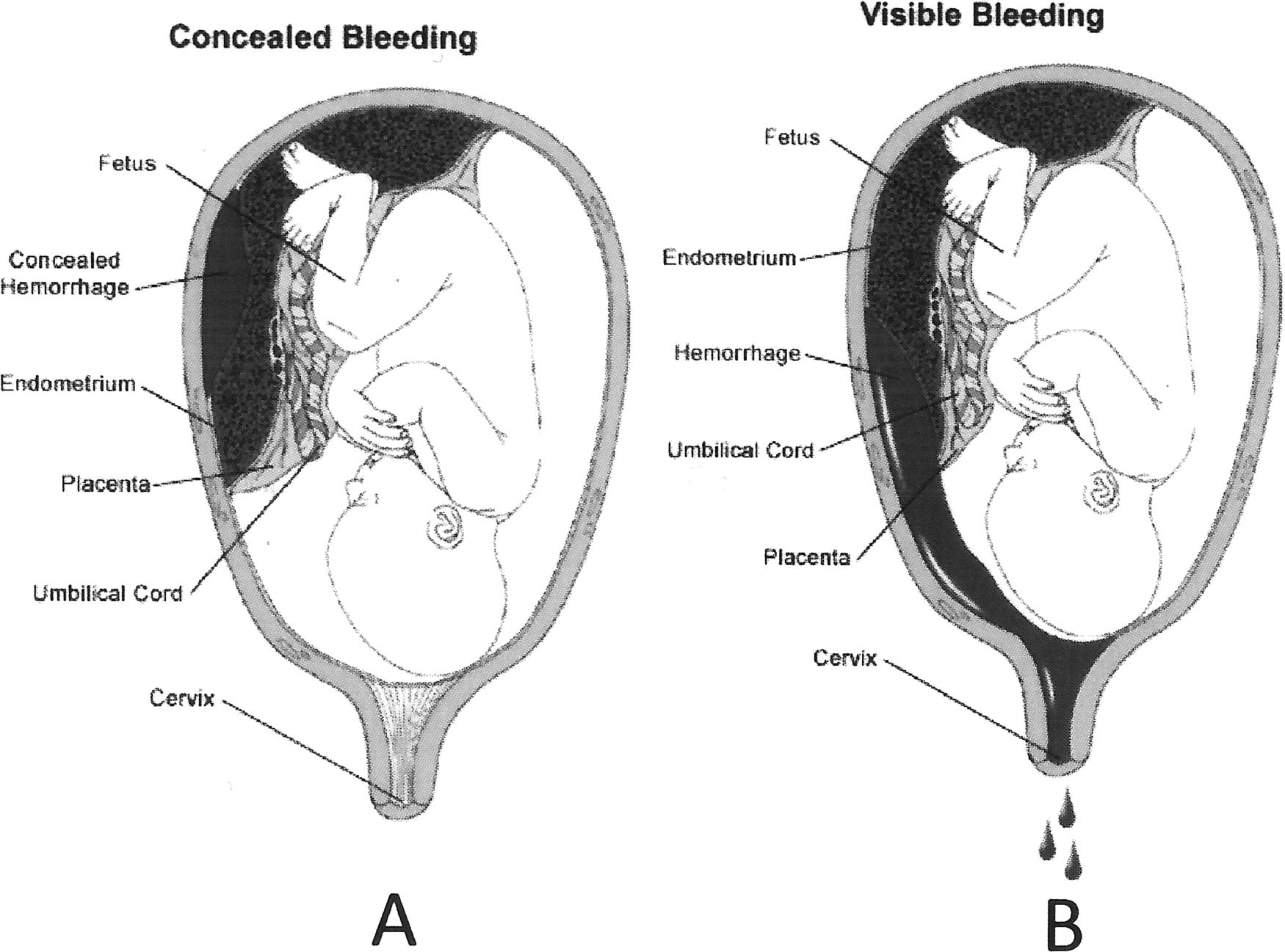
FIGURE 6.
Types of abruption. (A) Concealed abruption. Blood collects behind the placenta. There is no vaginal bleeding
and therefore no overt evidence of the abruption. (B) Clinically apparent abruption. Blood tracks between the membranes
and escapes through the vagina and cervix. The bleeding can range from scant to massive depending on the extent of the
abruption. Figure used by permission from the University of Utah Health Care (http://uuhsc.utah.edu/healthinfo/pediatric/
hrpregnant/bleed.htm).
clefts and other fetal anomalies after benzodiazepine expo-
the study. Their records showed heavy general use of health
sure, a large study of women whose deliveries were regis-
care, frequent alcohol and substance abuse, and other disor-
tered by the Medicaid system challenged this position.76 The
ders that could confound any effect of the benzodiazepines.
investigators identified 80 pregnant women who had received
Thus, the high rate of teratogenicity after heavy maternal
10 or more benzodiazepine prescriptions during the 4 years of
benzodiazepine use occurs when there is multiple alcohol andsubstance exposure and is not likely the result of benzodiaz-epine exposure. This finding has been confirmed by otherinvestigators.77 Benzodiazepines require albumin for serumtransport. In the fetus, serum albumin levels are quite lowuntil the third trimester when levels exceed maternal values.
Therefore, fetal benzodiazepine levels will remain low duringthe first and second trimester and increase to those greaterthan maternal levels during the third trimester. Accordingly,there exists evidence of impaired intrauterine growth, intox-ication, and neonatal abstinence syndrome in third-trimesterexposed fetuses.78 Significant differences also were seen inthe frequency of perinatal neurobehavior in benzodiazepine-exposed infants compared with controls. First-trimester ex-posure to Carbamazapine has been associated with an approx-imately 1-percent risk of neural tube defects.79 Because thisdefect may be prevented with maternal administration of folic
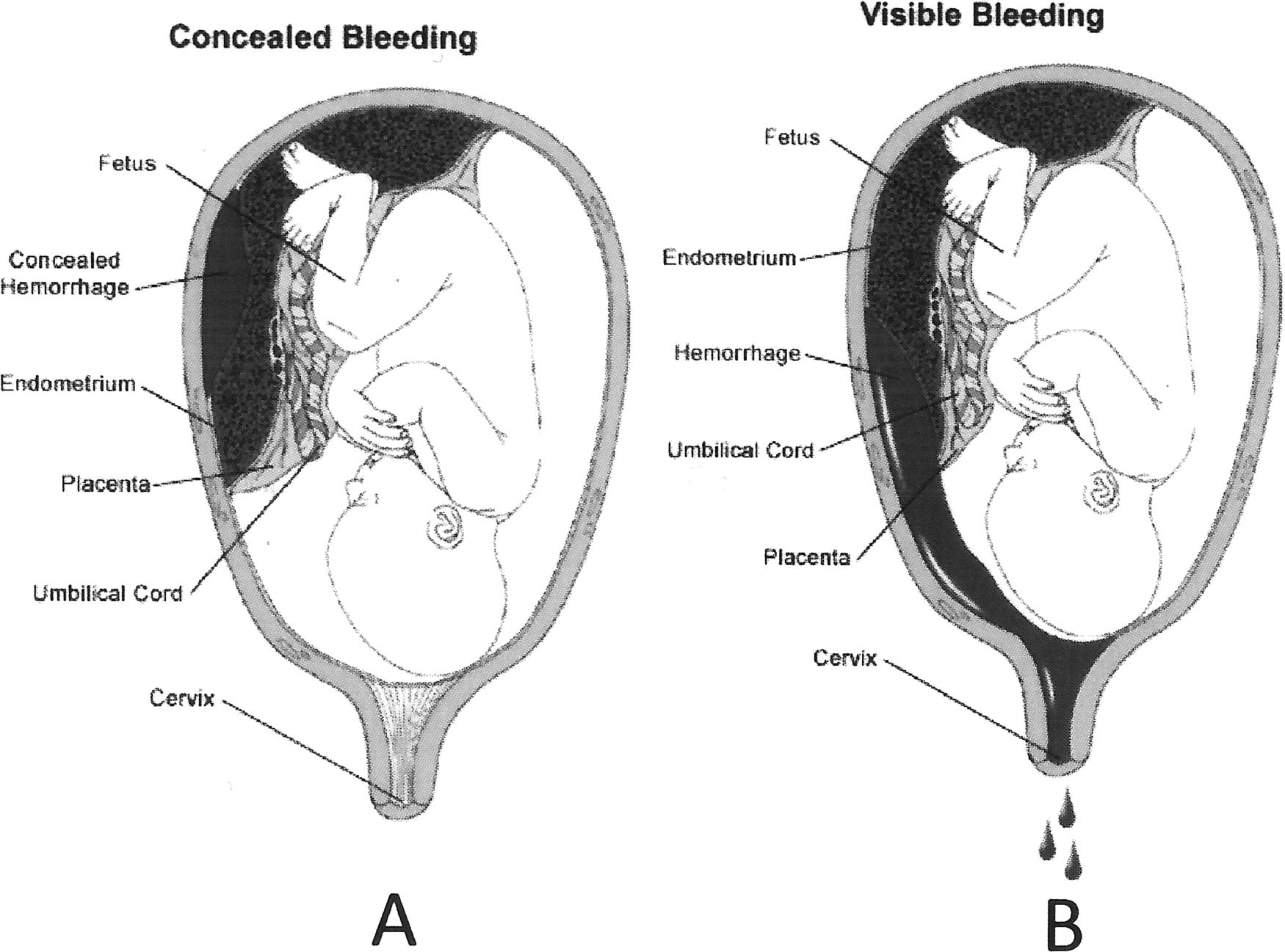
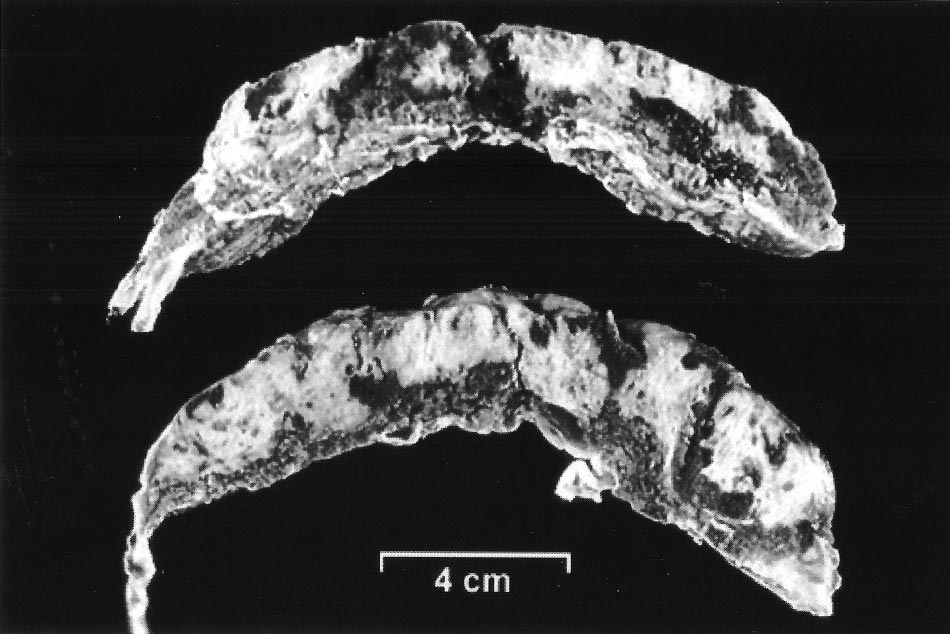
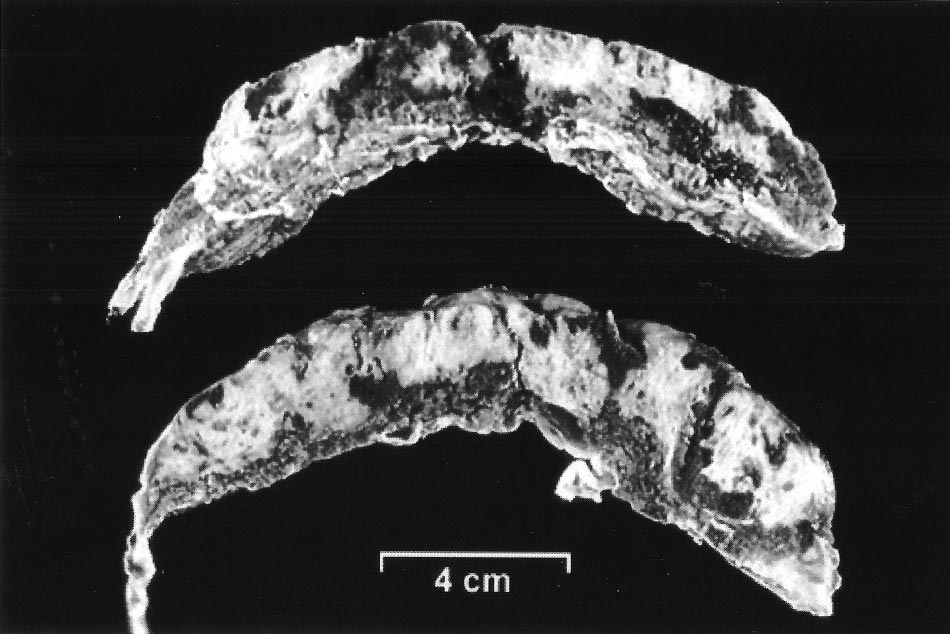
FIGURE 7.
Multiple placental infarcts. Gross sections
through the central placenta demonstrate infarction of
acid, it is recommended that all pregnant women receiving
⬎50% of the placental mass.
carbamazapine also receive folate supplementation.80 The
2008 American Society of Addiction Medicine
J Addict Med • Volume 2, Number 1, March 2008
Addiction Disorders in Pregnancy
FIGURE 8.
Maternal uterine artery Doppler flow studies. (A) Maternal uterine artery imaged on color flow mapping as it
crosses the internal iliac vessels. (B) Normal wave form pattern at 32 weeks. Note the soft systolic peaks and high level of for-
ward diastolic flow. This is consistent with a low resistance, high flow circuit. (C) Abnormal wave form from an opiate-depen-
dent patient in moderate withdrawal. Note the high, sharp systolic peak early diastolic notching and low level of diastolic
flow. This is consistent with a low flow, high resistance circuit.
efficacy of folic acid in preventing neural tube defects in this
particular setting, however, has not been proven. Conversely,
As mentioned earlier, opiates are not associated with
studies on adverse neurodevelopment as a consequence of
fetal malformations and the observed adverse pregnancy
carbamazapine exposure have been reassuring.81 Given this
outcomes are secondary to withdrawal and parallel high-risk
information, it may be reasonable to use a benzodiazepine for
behaviors. We now have more than 3 decades of experience
detoxification during the first trimester, reserving Carbamaza-
with the use of methadone for opiate detoxification and
pine for second and third trimester use.
agonist treatment. Long-term abstinence after detoxification
Disulfiram was approved by the FDA in 1952 for use as
is unusual in opiate addiction, and the best results have been
a deterrent to relapse in alcohol addiction. It acts by inhibiting
demonstrated with continued use of opiate agonist therapy.88
aldehyde dehydrogenase, which leads to accumulation of
Detoxification during pregnancy has been avoided
acetaldehyde when alcohol is ingested. The resulting symp-
since the 1970s, when there were several reports of associated
toms of the disulfiram-alcohol reaction include facial flush-
untoward outcomes. Rementeria and Nunag89 reported a
ing, tachycardia, hypotension, nausea, vomiting, and general
stillbirth occurring after acute narcotic withdrawal in a term
malaise. Although fetal anomalies have been reported in
pregnancy. Zuspan et al90 found increased amniotic fluid
pregnancies exposed to disulfiram, no specific pattern of
epinephrine levels in a woman undergoing a methadone
malformations exists. Furthermore, in all reported pregnan-
dosage taper. Catecholamine levels stabilized after the dosage
cies, exposure to other drugs of abuse, including cocaine,
was increased. In 1977, these authors recommended avoiding
opiates, and alcohol, were noted.82,83 In the only report to date
detoxification "unless a scientific means is available to mon-
of isolated disulfiram exposure during the first trimester,
itor fetal homeostasis." On the basis of reports such as these,
Helmbrecht and Abassi84 observed no anomalies nor were
physicians are reluctant to detoxify pregnant women, and
developmental disabilities noted.
Naltrexone and Acamprosate also are available as ad-
methadone maintenance has become standard practice. More
juncts to abstinence in patients with alcohol addiction. Nal-
recently, however, Dasche and colleagues used sonography
trexone was approved by the FDA for treatment of alcohol-
and fetal heart rate monitoring to assess the safety of detox-
ism in 1994. It is an opiate antagonist and has demonstrated
ification from methadone in 34 otherwise uncomplicated mid
efficacy in reducing alcohol consumption and craving
trimester pregnancies.91 Under carefully monitored inpatient
through its blocking of opiate receptor-mediated activation by
conditions, the authors performed a gradual methadone taper.
alcohol of dopaminergic pathways in the brain that are
The median maximum dose of methadone was 20 (range,
thought to be critical to reward. Limited data on exposure in
10 – 85) mg per day, and the median time to detoxification
humans has not indicated any association with anomalies or
was 12 (range, 3–39) days. Overall, 20 women (59%) suc-
developmental problems.85,86 Acamprosate has proven effi-
cessfully underwent detoxification and did not relapse, 10
cacy in decreasing drinking frequency and reducing relapse
(29%) relapsed to opiate use before delivery, and 4 (12%) did
drinking in abstinent alcoholics. The mechanism of action of
not complete detoxification and opted for methadone main-
acamprosate is obscure, although there is some evidence that
tenance. There was no evidence of fetal distress during
it modulates the function of NMDA receptors in brain.87
detoxification, no fetal death, and no preterm deliveries. Two
Currently, there are no data available on the use of Acam-
fetuses developed intrauterine growth restriction confirmed
prosate in pregnancy. If a medication is necessary to enhance
after delivery with birth weights less than the fifth percentile.
abstinence during pregnancy, one must weigh the risks of
Both infants were born of mothers in the relapse group.
continued alcohol use against the potential teratogenic risks
Interestingly, 3 of 20 neonates born to mothers who were
of the medication. Given the available data, Disulfiram or
successfully weaned from methadone required treatment for
Naltrexone would be the most appropriate choices.
neonatal abstinence syndrome.
2008 American Society of Addiction Medicine
Helmbrecht and Thiagarajah
J Addict Med • Volume 2, Number 1, March 2008
Although detoxification seems to be safe in the second
vulnerability in these children that then makes them more
trimester of pregnancy under carefully monitored conditions,
susceptible to impoverished environments. Therefore, pre-
relapse to opiate use seems to overshadow any potential
ventive interventions that focus both on enriching the early
benefits. Maas et al92 described pregnancy outcomes of 75
experiences of such children and improving the quality of the
gravid opiate users, 58 of whom participated in detoxification
home environment are likely to be particularly effective.
with methadone. Fifty-six percent of these women relapsed to
Controversy exists among methadone providers regard-
opiate use after detoxification. Neonatal abstinence syndrome
ing dosing regimens. Concern regarding the occurrence of
is reported in 15% to 55% of women who undergo successful
neonatal abstinence has resulted in a lowering of methadone
detoxification in the mid trimester. Despite an ability to
dose during pregnancy in many clinics. Dashe and col-
detoxify patients during pregnancy, this does not seem to
leagues,97 in a retrospective cohort study, demonstrated a
be a practical course to follow except under extraordinary
dose-dependent relationship with the incidence and severity
of NAS. The doses of methadone used in this population
Although methadone is not a teratogen, Rosen and
(20 – 40 mg per day) were below blocking levels. This has
Johnson93 have raised concern regarding neurodevelopmental
been associated with poor compliance with treatment, high
delay in methadone-exposed children. They followed a co-
rates of IUGR and prematurity, and correspondingly, a high
hort of methadone exposed neonates through 18 months of
incidence of polysubstance abuse.98 McCarthy and col-
age. Compared with unexposed controls, the methadone
leagues99 subsequently published on high- versus low-dose
group showed a significantly higher incidence of otitis media,
methadone maintenance therapy. In this report, high doses of
head circumferences below the third percentile, developmen-
methadone (⬎100 mg) were not associated with increased
tal delays, and poor fine motor coordination. These children
risks of neonatal abstinence symptoms but had a beneficial
also had significantly lower scores on the Bayley mental and
effect on maternal drug abuse. Thus, the dose of methadone
motor developmental indices. In a more recent prospective,
used should be individually assessed based on the presence of
longitudinal-matched cohort study, van Baar and colleagues94
symptoms of withdrawal and craving. Reducing the dose
assessed the neurobehavioral development of 35 infants of
during pregnancy will only increase the likelihood of relapse,
drug-dependent mothers with the development of 37 nonex-
thereby increasing the probability of adverse pregnancy
posed control infants. Significantly more infants of drug-
events. To the contrary, because methadone has a wide
dependent mothers than control children had electroencepha-
volume of distribution, significant dose increases are ex-
lograms rated as suspect or abnormal. By the end of the first
pected as the body mass and fluid volume increases during
month, the infants of drug-dependent mothers tended to be
the second and third trimesters. Given the rapid decline in
more active, and they had worse scores than the controls on
intravascular volume after delivery, our practice is to de-
the neonatal behavioral assessment scale. The results of these
crease the dose by 20% to 40% during the immediate post-
and other studies suggest that even after treatment for the
partum period.
neonatal abstinence syndrome, infants of drug-dependent
Methadone dosing is frequently split based on little
mothers seem to differ from comparison children, which
evidence of improved outcome. Data exist demonstrating a
could indicate later developmental problems. It is difficult,
higher elimination rate constant (k) and lower half-life com-
however, to establish what effects are directly attributable to
pared with nonpregnant controls;100 however, there are no
methadone, because many methadone patients in these stud-
studies that demonstrate that splitting the dose actually im-
ies used other drugs and had socioeconomic characteristics
proves pregnancy outcome. DePetrillo and Rice101 have
that are associated with poor neonatal outcome. Lifschitz and
shown an improvement in program compliance with split
colleagues95 published conflicting results. They found no
dosing, however. Splitting the methadone dose is, there-
significant effect of maternal heroin and methadone use on
fore, reasonable provided that the patient is not at risk for
head growth and neurodevelopmental performance in pre-
school-aged children. Their data did show an increased inci-
Fetuses exposed to methadone during the third trimes-
dence of low-average and mildly retarded intellectual perfor-
ter will have a higher rate of abnormal fetal testing. The
mance in the drug-exposed children. However, regression
challenge to the obstetric care provider is to determine which
analyses demonstrated that amount of prenatal care, prenatal
of the abnormal tests represent false-positive results and
risk score, and home environment were most predictive of
which deserve intervention. The most common test of fetal
intellectual performance and that the degree of maternal
well being used in the third trimester is the non-stress test
narcotic use was not a significant factor. In a particularly
(NST). Methadone causes a higher false-positive or nonreac-
insightful study of the neurodevelopmental consequences of
tive rate in the NST particularly if performed 1 to 3 hours
methadone exposure, Hans96 showed that methadone-ex-
after a dose.92–104 In these instances, a biophysical profile
posed infants reared in extremely poor environmental circum-
should be performed as a follow-up or primary test. It should
stances showed much delayed mental development. Indeed,
be noted that fetal breathing movements also will be de-
they seemed to function more poorly than nonexposed infants
creased as a consequence of methadone.105
reared in similar environments and more poorly than metha-
Doppler studies of the umbilical artery and middle
done-exposed infants reared in more adequate environments.
cerebral artery are helpful adjuncts to tests of fetal well-
These findings suggest that in the cognitive domain, metha-
being. The former will indicate the degree of placental vas-
done may not cause a behavioral deficit but instead create a
cular resistance caused by previous infarction or intervillous
2008 American Society of Addiction Medicine
J Addict Med • Volume 2, Number 1, March 2008
Addiction Disorders in Pregnancy
space thrombosis, and the latter will provide valuable infor-
alternatives to methadone for the treatment of opioid addic-
mation regarding the placenta's ability to deliver adequate
tion in the general population.
oxygen to the fetus. In cases of sublethal placental injury, the
Well-controlled studies of the safety and efficacy of
systolic:diastolic ratio and pulsitility index measured in the
Buprenorphine in pregnancy are lacking. From the limited
umbilical artery will increase as resistance to flow within the
data available, it does not seem to be teratogenic in humans116
placental vasculature increases. With more severe placental
or animals.117 Administered in monotherapy form as Subutex,
dysfunction, diastolic blood flow will decrease or disappear
it has been used successfully in opioid-dependent pregnant
altogether, thus increasing these values. In the end stage,
women as a maintenance replacement opioid.118–124 A 2003
preterminal condition, reversal of diastolic flow is seen. As
review of the available clinical studies has been published
fetal oxygenation declines with declining placental function,
covering approximately 300 pregnancies.125 Compared with
the fetus responds by shifting cardiac output to favor cerebral
methadone, a lower incidence of NAS has been reported in
flow at the expense of decreasing flow to the splanchnic bed,
buprenorphine-exposed neonates. The severity of NAS is
including bowel and kidneys. Thus, a trend of increasing
reduced as assessed by total opiate required to treat and
resistance in the umbilical artery, decreasing resistance in the
length of hospital stays. Some data suggest that the placental
middle cerebral artery, and declining amniotic fluid volume
transfer of this opioid may be limited in comparison with
provides compelling evidence of declining placental function
others, such as methadone, thereby limiting fetal exposure
and identifies the fetus that will require closer testing and may
and the development of dependency.126 Deshmukh and col-
need early delivery to prevent hypoxic-ischemic brain injury.
leagues127 have demonstrated that a large proportion of bu-
Whether to encourage breastfeeding in methadone-
prenorphine is metabolized to Norbuprenorphine, the only
treated mothers varies significantly by institution. Methadone
metabolite formed as determined by high-performance liquid
is transferred to breast milk.106,107 Some investigators have
chromatography and mass spectrometry, by placental aro-
reported the quantities to be sufficient to prevent or amelio-
matase (CYP 19) within the microsomal fraction of the
rate withdrawal symptoms in symptomatic infants,107–109 but
based on a more detailed analysis of the methadone levels in
There is a paucity of information available on breast-
breast milk, other investigators have questioned this conclu-
feeding. Small amounts of buprenorphine are excreted inbreast milk. In one study, the estimated daily dose of this
sion.110,111 Milk:plasma ratios ranging from 0.83112 to values
agent to the newborn of a mother taking 4 mg per day was 3.3
as low as 0.24111 have been reported. One estimate of the
g per day.128 Because buprenorphine is not active if swal-
relative infant dose of methadone (with consideration of the
lowed, it would not be anticipated to have any adverse effects
50-50 mixture of R and S isomers normally in methadone)
on the neonate. It probably has little pharmacologic effect
was 2.8% of the maternal dose.111 The American Academy of
because no withdrawal signs have been noted when maternal
Pediatrics and the WHO Working Group on Human Lactation
feeding is later abruptly interrupted.128 Specific studies be-
classified methadone as compatible with breastfeeding.113,114
yond case reports on this agent are lacking. Breastfeeding can
Given the overwhelming benefit of breastfeeding in promot-
and should be encouraged in this group of patients with
ing the mother-infant bond, we believe that breastfeeding
appropriate informed consent.
should be strongly encouraged in these at-risk parents pro-
Despite its potential advantages over methadone, bu-
vided no other contraindication, such as maternal HIV infec-
prenorphine is not approved by the FDA for use in pregnancy
tion exists. As a precaution, all mothers should be warned
and any such use is considered "off label." It should be noted
to seek medical advice if their exposed infant appears
that there are no studies that evaluate possible long-term
effects on the behavior and neurodevelopment of exposed
Buprenorphine is an opioid analgesic similar to mor-
human infants. Methadone, therefore, remains the "gold stan-
phine but with greater potency and with agonist-antagonist
dard" for maintenance therapy during pregnancy. Subutex
properties. It is marketed in IV form as Buprenex and in an
should only be used after obtaining and carefully document-
orally administered formulation as Subutex. Suboxone is a
ing informed consent.
combination drug containing buprenorphine and naloxone.
Naloxone is not active if taken orally or sublingually but willprecipitate a withdrawal state if injected intravenously. This
property along with the "ceiling effects" on euphoria and
Cocaine is a local anesthetic and a potent, short-
respiratory suppression contributes to the safety profile lim-
acting stimulant of the central nervous system. Illicit
ited abuse potential of the drug. Indeed, it antagonizes the
cocaine use is by inhalation of powder or intravenous
respiratory depression produced by anesthetic doses of fent-
injection. Other derivatives of cocaine, such as its pelleted
anyl about as well as does naloxone without completely
free base ("crack"), are smoked, sometimes after mixing
reversing other opioid effects, such as analgesia.115 Com-
with tobacco or marijuana.
pared with methadone, the abuse potential is markedly lower,
Whether cocaine causes human malformations is con-
which allows for its use in an outpatient office setting.
troversial. Several studies of the offspring of women who
Because buprenorphine has an extremely high binding affin-
abused cocaine during pregnancy have described an increased
ity for the mu receptor, only limited euphoric effects result
incidence of cranial defects, including exencephaly, enceph-
when a patient relapses to an illicit opiate. As expected,
alocele, and parietal bone defects, limb reduction defects,
Subutex and Suboxone have well-documented efficacy as
urogenital abnormalities, and intestinal perforation, obstruc-
2008 American Society of Addiction Medicine
Helmbrecht and Thiagarajah
J Addict Med • Volume 2, Number 1, March 2008
tion, or atresia.129–131 Other studies have found no association
relaxant and antispasmodic and has been used in pregnancy
between antenatal cocaine use and fetal malformations. Neer-
for the treatment of spasticity in patients with pregnancies
hof and colleagues132 failed to find a significant increase in
complicated by multiple sclerosis or spinal cord disease. The
anomalies among 138 children born to women with positive
most common use during pregnancy is in spinal cord injury
screens for cocaine at the time of labor. Cocaine use in this
patients. Baclofen is effective, given via an intrathecal cath-
report was, however, associated with an increase in preterm
eter, in preventing the enormous spastic symptoms and sec-
birth, intrauterine growth retardation, and placental abrup-
ondary autonomic dysregulation induced by uterine contrac-
tion. The mechanism by which cocaine may induce placental
tions.141 Intrathecal delivery of the drug requires only
abruption is via intense transient hypertension and vasocon-
approximately 1% of the dose necessary for oral administra-
striction produced by the drug. Extensive study of the hemo-
tion. Placental transfer is sufficient enough that, when taken
dynamic effects of cocaine on the pregnant ewe and fetus
orally throughout pregnancy, a neonatal abstinence syndrome
have confirmed this hypertensive response as well as a
is observed, manifest largely by neonatal seizures.142
corresponding decrease in uterine blood flow that lasts ap-
Assuming equal efficacy in the management of cocaine
proximately 15 minutes after initial administration.133
addiction, topiramate seems to be the safer of the 2 agents
Topiramate, an anticonvulsant, raises cerebral GABA
with respect to fetal effects. At this time, however, there is
levels, facilitates GABAergic neurotransmission, and inhibits
insufficient data to support the widespread use of either agent
glutamatergic activity at AMPA/kainite receptors.134 Because
in the nonpregnant population. Further confirmatory studies
both GABAergic and glutamatergic neurons seem to be
are necessary to justify adoption into routine clinical practice.
important modulators of the brain reward system, one may
Use in pregnancy should be considered experimental and
anticipate that Topiramate would be beneficial in treating
limited to use on protocol with well-documented informed
cocaine addiction. Kampman and colleagues recently per-
consent. Given the promising preliminary reports of the
formed a pilot study of Topiramate in cocaine-addicted sub-
therapeutic effects of both agents, optimism with respect to
jects.135 In a double-blind, placebo-controlled trial of 40 such
their future use seems justified.
subjects during 13 weeks, they showed that after week 8,when the dose titration was completed, topiramate-treated
subjects were more likely to be abstinent from cocaine
Amphetamines are centrally acting stimulants that may
compared with placebo-treated subjects. Topiramate-treated
have some efficacy in the treatment of narcolepsy but that are
subjects also were more likely to attain 3 weeks of continuous
largely ineffective in the treatment of obesity. Methylpheni-
abstinence from cocaine.
date has largely replaced methamphetamine in the manage-
Currently, there are no studies on the potential benefits
ment of narcolepsy during pregnancy. The abuse of metham-
of topiramate for cocaine addiction during pregnancy; how-
phetamine leads to the ingestion of large and uncontrolled
ever, this medication is commonly used in pregnancy for
doses during pregnancy. When methamphetamine use has
treatment of seizure disorders. In the few cases in which fetal
been studied among addicted mothers, the specific adverse
malformations are reported,136,137 the constellation of malfor-
effects of the drug is difficult to discern because of the
mations (growth deficiency, a third fontanelle, short nose
confounding effects of other drugs used in combination (eg,
with anteverted nares, blunt distal phalanges, and generalized
ethanol) as well as poor maternal nutrition, hygiene, and
blunting of the nails with fifth nail hypoplasia) is consistent
attendance at prenatal visits.143–145 Like cocaine, the prepon-
with anomalies found in infants exposed prenatally to other
derance of available data would suggest little or no effect of
anticonvulsants as well. Topiramate use during pregnancy for
amphetamines on organogenesis. A recent, prospective eval-
cocaine addiction may be justified, depending on the severity
uation of 228 amphetamine-exposed pregnancies by Jones
of the addiction and the physician's assessment of the risk to
and colleagues146 did not show any increase in spontaneous
the fetus from ongoing cocaine use.
abortion, major, or minor malformations. The effects of
Baclofen is a GABA B receptor agonist that has drawn
amphetamines on the gravid uterus and fetus are similar to
recent interest in the treatment of cocaine addiction. Several
those seen with cocaine. Stek and colleagues147 have devel-
studies in laboratory animals have demonstrated attenuation
oped a model in pregnant ewes. Placental transfer of the drug
of cocaine-seeking and a decrease in the selective molecular
is rapid and because the fetus has a longer elimination
and behavioral effects of cocaine.138,139 In a recent placebo-
half-life than the mother, total exposure of the fetus is high.
controlled, randomized trial of Baclofen,140 70 subjects were
Maternal ingestion is associated with an elevation in both
randomly assigned to Baclofen (20 mg t.i.d.) or placebo
maternal and fetal blood pressure, and a decrease in fetal
during a 16-week period. Primary outcome measures were
oxyhemoglobin saturation and pH. A transient increase in
retention in treatment, cocaine use, cocaine craving, and
umbilical vascular resistance and a decrease in uterine blood
adverse events. Participants assigned to receive Baclofen
flow accompanied these changes.147,148
demonstrated significant and stepwise increases in the prob-
At least 2 medications have been tested for the treat-
ability of providing negative urine toxicology screens for
ment of amphetamine addiction. Galloway and colleagues149
benzoylecgonine. Participants assigned to placebo demon-
conducted a randomized, clinical trial of imipramine in the
strated no such association. There was no statistical signifi-
treatment of methamphetamine dependence. Thirty-two pa-
cance observed for retention in treatment, cocaine craving, or
tients were randomized to receive 10 or 150 mg of imipramine
incidence of reported adverse events. Baclofen is a muscle
per day for 180 days. Retention in treatment was significantly
2008 American Society of Addiction Medicine
J Addict Med • Volume 2, Number 1, March 2008
Addiction Disorders in Pregnancy
longer for subjects who were treated with 150 mg of imipramine
occur during pregnancy, addiction treatment during preg-
compared with control. There was, however, no difference noted
nancy can be improved greatly with a cooperative team
between the 2 groups of subjects in stimulant craving, self-report
of time since last use of stimulants, or percent of urinalysespositive for stimulants. Vigabatrin (gamma vinyl-GABA), an
irreversible inhibitor of GABA aminotransferase, also has been
1. Platrow LM. Punishing women for their behavior during pregnancy: an
tested in patients with amphetamine dependence.150 In that
approach that undermines the health of women and children. In:
study, 16 of 18 patients tested negative for methamphetamine
Wetherington CL, Roman AB, eds. Drug Addiction Research and the
and cocaine during the last 6 weeks of the trial. GVG did not
Health of Women. Bethesda, MD: National Institute on Drug Abuse;
produce any visual field defects or alterations in visual acuity.
2. Diekman ST, Floyd RL, De'Coufle P, et al. A survey of obstetrician-
Furthermore, it did not produce changes in vital signs even
gynecologists on their patients' alcohol use during pregnancy. Obstet
with continued use of methamphetamine and cocaine. Expe-
rience with Vigabatrin during pregnancy is limited, consist-
3. Roche AM, Richard GP. Doctors' willingness to intervene in patients'
ing only of case reports. There is insufficient data to comment
drug and alcohol problems. Soc Sci Med. 1991;33:1053–1061.
4. March of Dimes. Cocaine use during pregnancy (Quick reference: Fact
on its safety.
sheet. December 2002). Available at: http//www.marchofdimes.com/
In summary, pregnant women with addiction disorders
professionals/14332_1169. asp. Accessed March 4, 2005.
represent both a unique challenge and an opportunity for the
5. March of Dimes. Drinking alcohol during pregnancy (Quick reference:
health care provider. Although not as prevalent as in men,
Fact sheet. August 2002). Available at: http://www.marchofdimes.com/professionals/14332_1170. asp. Accessed March 4, 2005.
women with substance abuse disorders differ significantly
6. Funkhouser AW, Butz AM, Feng TI, et al. Prenatal care and drug use
from men in patterns of use, agents they abuse, family history
in pregnant women. Drug Alcohol Depend. 1993;33:1–9.
and predisposing factors. The observed co-occurring psychi-
7. Fox K, Merrill JF, Chang HM, et al. Estimating the costs of substance
atric disorders also differ from those of men. The added
abuse to the Medicaid hospital care program. Am J Public Health.
shame and guilt associated with the presence of the fetus will
8. Martin SL, English KT, Clark KA, et al. Violence and substance use
frequently add to break down the denial and allow opportu-
among North Carolina pregnant women. Am J Public Health. 1996;86:
nity for more effective intervention. Medical and obstetric
complications from substance abuse and parallel high-risk
9. Kauffman E. Diagnosis and treatment of drug and alcohol abuse in
behaviors represent a significant contribution to perinatal
women. Am J Obstet Gynecol. 1995;174:21–27.
10. Westermeyer J, Wahmanholm K, Thuras P. Effects of childhood
morbidity and mortality and can be reduced with aggressive
physical abuse on course and severity of substance abuse. Am J Addict.
screening and intervention. Currently, obstetric care provid-
ers in general lack sufficient skill to identify the addicted
11. McCauley J, Kern DE, Kolodner K, et al. Clinical characteristics of
pregnant woman and refer for treatment. A goal of the
women with a history of childhood abuse: unhealed wounds. JAMA.
1997;277:1362–1368.
addiction medicine community should be to provide this
12. Kendler KS, Bulik CM, Silberg J, et al. Childhood sexual abuse and
education where appropriate.
adult psychiatric and substance use disorders in women: an epidemio-
New and highly efficacious medications are becoming
logical and cotwin control analysis. Arch Gen Psychiatry. 2000;57:
available at a pace never seen before in the field. The
13. Prescott CA, Aggen SH, Kendler KS. Sex-specific genetic influences
availability of Buprenorphine has moved opiate addiction
on the comorbidity of alcoholism and major depression in a population-
from the methadone clinic to the physician's office. This has
based sample of U.S. twins. Arch Gen Psychiatry. 2000;57:803–811.
gone a long way to destigmatize the disease and has increased
14. Baumann M, Pommier J, Deschamps JP. Prescription medicale et
access to treatment to many who would not have otherwise
consommation de psychotropes: quelques interrogations sur les differ-ences entre hommes et femmes. Cah Sociol Demogr Med. 1996;36:
had the opportunity. GABA-modulating agents show great
promise as effective adjuncts to treatment of alcohol and
15. Bardel A, Wallander MA, Svardsudd K. Reported current use of
cocaine addictions. With the exception of the currently on-
prescription drugs and some of its determinants among 35- to 65-year-
going Agonist Treatment of Opioid-Addicted Pregnant
old women in mid-Sweden: a population-based study. J Clin Epide-miol. 2000;53:637–643.
Women trial, few of the new agents have been tested in the
16. Weaver M, Schnoll S. Addiction issues in prescribing opioids for
gravid population. Clearly, more studies specifically directed
chronic nonmalignant pain. J Addict Med. 2007;1:1–10.
at this special population are needed. This does not necessar-
17. Bodkin JA, Zornberg GL, Lukas SE, et al. Buprenorphine treatment for
ily exclude pregnant women from access to treatment be-
refractory depression. J Clin Psychopharmacol. 1995;15:49–57.
18. Office of Applied Studies. Department of Health and Human Services.
cause, as with most other medications, off-label prescribing
Results from the 2003 National Survey on Drug Use and Health:
may still be appropriate provided certain criteria apply.
national findings. DHHS Publication no. SMA 04-3964, NSDUH
Proper communication between the obstetric care provider
Series H-25. Rockville, MD: Substance Abuse and Mental Health
and the addiction treatment team will ensure that medications
Services Administration; 2004.
will be selected to provide the best potential efficacy while
19. Office of Applied Studies. Department of Health and Human Services.
Summary of findings from the 2000 National Household Survey on
minimizing risk to the fetus. In addition to identification of
Drug Abuse. DHHS Publication no. SMA 01-3549, NHS DA Series.
medications that might be reasonably safe and effective in
Rockville, MD: Substance Abuse and Mental Health Services Admin-
maintaining abstinence, these lines of communication will
provide for the development of more rational antepartum
20. Greenfied SF, Manwani SG, Nargiso JE. Epidemiology of substance
use disorders in women. Obstet Gynecol Clin N Am. 2003;30:413–446.
testing schedules designed to meet the needs of the individual
21. Office of Applied Studies. Department of Health and Human Services.
patient. As with many other complex medical problems that
National Survey on Drug Use and Health Report: substance use during
2008 American Society of Addiction Medicine
Helmbrecht and Thiagarajah
J Addict Med • Volume 2, Number 1, March 2008
pregnancy: 2002 and 2003 update. June, 2005; Available at: http://
results of a large prospective study in pregnant women. Hepatogastro-
www.oas.samhsa.gov. Accessed July 27, 2007.
22. Bachi K, Varner M, Chase R. The prevalence of substance abuse
46. Polis CB, Shah SN, Johnson KE, et al. Impact of maternal HIV
among pregnant women in Utah. Am J Obstet Gynecol. 1993;81:239–
coinfection on the vertical transmission of hepatitis C virus: a meta-
analysis. Clin Infect Dis. 2007;44:1123–1131.
23. Chasnoff I, Landress H, Barrett M. The prevalence of illicit drug and
47. European Paediatric Hepatitis C Virus Network. A significant sex– but
alcohol use during pregnancy and discrepancies in mandatory reporting
not elective cesarean section– effect on mother-to-child transmission of
in Pinellas County, Florida. N Engl J Med. 1990;322:1202–1206.
hepatitis C virus infection. J Infect Dis 2005;192:1872–1879.
24. Hollinshead WH, Brin JF, Scot HD, et al. Current statewide prevalence
48. European Paediatric Hepatitis C Virus Network. Effects of mode of
of illicit drug use by pregnant women: Rhode Island. MMWR Morb
delivery and infant feeding on the risk of mother- to-child transmission
Mortal Wkly Rep. 1990;39:225–227.
of hepatitis C virus. BJOG. 2001;108:371–377.
25. Chasnoff IJ, Neuman MA, Thornton C, et al. Screening for substance
49. Gibb DM, Goodall RL, Dunn DT, et al. Mother-to-child transmission
abuse in pregnancy: a practical approach for the primary care physi-
of hepatitis C virus: evidence for preventable peripartum transmission.
cian. Am J Obstet Gynecol. 2001;184:752–758.
26. Hutchins E, Dipietro J. Psychological risk factors associated with
50. Mast EE, Hwang LY, Seto DS, et al. Risk factors for perinatal
cocaine use during pregnancy: a case-control study. Obstet Gynecol.
transmission of hepatitis C virus (HCV) and the natural history of HCV
infection acquired in infancy. J Infect Dis. 2005;192:1880–1889.
27. Fischer PJ, Breakey R. The epidemiology of alcohol, drugs, and mental
51. McIntyre PG, Tosh K, McGuire W. Caesarean section versus vaginal
disorders among homeless persons. Am Psychol. 1991;46:1115–1128.
delivery for preventing mother to infant hepatitis C virus transmission.
28. Chavkin W, Paone D, Friedmann P, et al. Psychiatric histories of drug
Cochrane Database Syst Rev. 2006:CD005546.
using mothers: treatment implications. J Subst Abuse Treat. 1993;10:
52. Mortensen JT, Olsen J, Larsen H, et al. Psychomotor development in
children exposed in utero to benzodiazepines, antidepressants, neuro-
29. Svikis DS, Golden AS, Huggins GR, et al. Cost-effectiveness of
leptics, and anti-epileptics. Eur J Epidemiol. 2003;18:769–771.
treatment for drug-abusing pregnant women. Drug Alcohol Depend.
53. Jones HE, Haug N, Silverman K, et al. The effectiveness of incentives
in enhancing treatment attendance and drug abstinence in methadone-
30. Belperio PS, Rhew DC. Prevalence and outcomes of anemia in indi-
maintained pregnant women. Drug Alcohol Depend. 2001;61:297–306.
viduals with human immunodeficiency virus: a systematic review of
54. Ananth CV, Berkowitz GS, Savitz DA. Placental abruption and adverse
the literature. Am J Med 2004;116 (Suppl 7A):27S–43S.
perinatal outcomes. JAMA. 1999;282:1646–1651.
31. Volberding PA, Levine AM, Dieterich D, et al. Anemia in HIV
55. Ananth CV, Savitz DA, Bowes WA, et al. Influence of hypertensive
infection: clinical impact and evidence-based management strategies.
disorders and cigarette smoking on placental abruption and uterine
Clin Infect Dis. 2004;38:1454–1463.
bleeding during pregnancy. Br J Obstet Gynaecol. 1997;104:572–578.
32. Moyle G. Anaemia in persons with HIV infection: prognostic marker
56. Handler A, Kistin N, Davis F, et al. Cocaine use during pregnancy:
and contributor to morbidity. AIDS Rev. 2002;4:13–20.
perinatal outcomes Am J Epidemiol. 1991;133:818–825.
33. Townsend CL, Tookey PA, Cortina-Borja M, et al. Antiretroviral
57. Ananth CV, Smulian JC, Vintzileos AM. Incidence of placental abrup-
therapy and congenital abnormalities in infants born to HIV-1-infected
tion in relation to cigarette smoking and hypertensive disorders during
women in the United Kingdom and Ireland, 1990 to 2003. J Acquir
pregnancy: a meta-analysis of observational studies. Obstet Gynecol.
Immune Defic Syndr. 2006;42:91–94.
34. Horrigan TJ, Schroeder AV, Schaffer RM. The triad of substance
58. Homayoun A, Dombrowski MP, Leach KC, et al. Characterization of
abuse, violence, and depression are interrelated in pregnancy. J Subst
the effect of cocaine on catecholamine uptake by pregnant myome-
Abuse Treat. 2000;18:55–58.
trium. Obstet Gynecol. 1995;85:93–96.
35. Wen SW, Yang Q, Garner P, et al. Selective serotonin reuptake
59. Hurd WW, Betz AL, Dombrowski MP, et al. Cocaine augments
inhibitors and adverse pregnancy outcomes. Am J Obstet Gynecol.
contractility of the pregnant human uterus by both adrenergic and
nonadrenergic mechanisms. Am J Obstet Gynecol. 1998;178:1077–
36. Malm H, Klaukka T, Neuvonen PJ. Risks associated with selective
serotonin reuptake inhibitors in pregnancy. Obstet Gynecol. 2005;106:
60. Nakahara K, Iso A, Chao CR, et al. Pregnancy enhances cocaine-
induced stimulation of uterine contractions in the chronically instru-
37. Einarson TR, Einarson A. Newer antidepressants in pregnancy and
mented rat. Am J Obstet Gynecol. 1996;175:188–193.
rates of major malformations: a meta-analysis of prospective compar-
61. Hurd WW, Robertson PA, Riemer RK, et al. Cocaine directly augments
ative studies. Pharmacoepidemiol Drug Saf. 2005;14:823–827.
the alpha-adrenergic contractile response of the pregnant rabbit uterus.
38. GlaxoSmithKline. Use of Paxil CR or Paxil during pregnancy. Avail-
Am J Obstet Gynecol. 1991;164:182–187.
able at: http://www.gskus.com/news/paroxetine/paxil_letter_e3.pdf. Ac-
62. Dixon WR, Chang AP. Effect of phentolamine on blood pressure, heart
cessed July 27, 2007.
rate and plasma catecholamine levels in conscious, unrestrained mor-
39. US Food and Drug Administration. Paroxetine (Paxil) use during
phine dependent rats during naloxone precipitated autonomic with-
pregnancy. Available at: http://www.fda.gov/cder/drug/advisory/
drawal responses. Proc West Pharmacol Soc. 1988;31:117–119.
paroxetine200512.htm. Accessed July 27, 2007.
63. Clark LT, Friedman HS. Hypertension associated with alcohol with-
40. Levinson-Castiel R, Merlob P, Linder N., et al. Neonatal abstinence
drawal: assessment of mechanisms and complications. Alcohol Clin
syndrome after in utero exposure to selective serotonin reuptake inhib-
Exp Res. 1985;9:125–130.
itors in term infants. Arch Pediatr Adolesc Med. 2006;160:173–176.
64. Albuquerque CA, Smith KR, Johnson C, et al. Influence of maternal
41. Sanz EJ, De-las-Cuevas C, Kiuru A, et al. Selective serotonin reuptake
tobacco smoking during pregnancy on uterine, umbilical and fetal
inhibitors in pregnant women and neonatal withdrawal syndrome: a
cerebral artery blood flows. Early Hum Dev 2004;80:31–42.
database analysis. Lancet. 2005;365:482–487.
65. Breslau N, Paneth N, Lucia VC, et al. Maternal smoking during
42. Chambers CD, Hernandez-Diaz S, Van Marter LJ., et al. Selective
pregnancy and offspring IQ. Int J Epidemiol. 2005;34:1047–1053.
serotonin-reuptake inhibitors and risk of persistent pulmonary hyper-
66. Koss KS, Nesheim B-i, Wesche J. Effect of smoking on blood veloc-
tension of the newborn. N Engl J Med 2006;354:579–587.
ities in the uterine artery of pregnant women and in the radial artery.
43. ACOG Committee Opinion No. 354. Treatment with selective seroto-
Acta Obstet Gynecol Scand Suppl. 1980;93:36.
nin reuptake inhibitors during pregnancy. Obstet Gynecol. 2006;108:
67. Jacobsson B, Mattsby-Baltzer I, Andersch B, et al. Microbial invasion
and cytokine response in amniotic fluid in a Swedish population of
44. Koren G, Moretti M, Kapur B. Can venlafaxine in breast milk attenuate
women with preterm prelabor rupture of membranes. Acta Obstet
the norepinephrine and serotonin reuptake neonatal withdrawal syn-
Gynecol Scand 2003;82:423–431.
drome. J Obstet Gynaecol Can. 2006;28:299–302.
68. Witt A, Berger A, Gruber CJ, et al. IL-8 concentrations in maternal
45. Saez A, Losa M, Lo Iacono O, et al. Diagnostic and prognostic value
serum, amniotic fluid and cord blood in relation to different pathogens
of virologic tests in vertical transmission of hepatitis C virus infection:
within the amniotic cavity. J Perinat Med. 2005;33:22–26
2008 American Society of Addiction Medicine
J Addict Med • Volume 2, Number 1, March 2008
Addiction Disorders in Pregnancy
69. Dinsmoor MJ, Irons SJ, Christmas JT. Preterm rupture of the mem-
97. Dashe JS, Sheffield JS, Olscher DA, et al. Relationship between
branes associated with recent cocaine use. Am J Obstet Gynecol.
maternal methadone dosage and neonatal withdrawal. Obstet Gynecol.
70. Rayburn WF. A physician's prerogative to prescribe drugs for off-label
98. Kashiwagi M, Arlettaz R, Lauper U, et al. Methadone maintenance
uses during pregnancy. Obstet Gynecol. 1993;81:1052–1055.
program in a Swiss perinatal center: I. Management and outcome of 89
71. Floyd RL, O'Connor MJ, Sokol RJ, et al. Recognition and prevention
pregnancies. Acta Obstet Gynecol Scand. 2005:140–144.
of fetal alcohol syndrome. Obstet Gynecol. 2005;106:1059 –1064.
99. McCarthy JJ, Leamon MH, Parr MS, et al. High-dose methadone
72. Park KH, Yoon BH, Shim SS, et al. Amniotic fluid tumor necrosis
maintenance in pregnancy: maternal and neonatal outcomes. Am J
factor-alpha is a marker for the prediction of early-onset neonatal sepsis
Obstet Gynecol. 2005;193:606–610.
in preterm labor. Gynecol Obstet Invest. 2004;58:84–90.
100. Jarvis MA, Wu-Pong S, Kniseley JS, et al. Alterations in methadone
73. Yonkers KA, Kando JC, Cole JO, et al. Gender differences in phar-
metabolism during late pregnancy. J Addict Dis. 1999;18:51–61.
maco/kinetics and pharmacodynamics of psychotropic medication. Am
101. DePetrillo PB, Rice JM. Methadone dosing and pregnancy: impact on
J Psychiatry. 1992;149:587–595.
program compliance. Int J Addict. 1995;30:207–217.
74. Mueller TI, Stout RL, Rudden S, et al. A double-blind, placebo-
102. Archie CL, Lee MI, Sokol RJ, et al. The effects of methadone treatment
controlled pilot study of carbamazepine for the treatment of alcohol
on the reactivity of the nonstress test. Obstet Gynecol. 1989;74:254–
dependence. Alcohol Clin Exp Res. 1997;21:86–92.
75. Malcolm R, Ballenger JC, Sturgis ET, et al. Double-blind controlled
103. Levine AB, Rebarber A. Methadone maintenance treatment and the
trial comparing carbamazepine to oxazepam treatment of alcohol with-
nonstress test. J Perinatol. 1995;15:229–231.
drawal. Am J Psychiatry. 1989;146:617–621.
104. Anyaegbunam A, Tran T, Jadali D, et al. Assessment of fetal well-
76. Bergman U, Rosa FW, Baum C, et al. Effects of exposure to benzo-
being in methadone-maintained pregnancies: abnormal nonstress tests.
diazepine during fetal life. Lancet. 1992;340:694–696.
Gynecol Obstet Invest. 1997;43:25–28.
77. Rosenberg L, Mitchell AA, Parsells JL, et al. Lack of relation of oral
105. Cejtin HE, Mills A, Swift EL. Effect of methadone on the biophysical
clefts to diazepam use duringpregnancy. N Engl J Med. 1983;309:
profile. J Reprod Med. 1996;41:819–822.
106. McCarthy JJ, Posey BL. Methadone levels in human milk. J Hum Lact.
78. Laegreid L, Hagberg G, Lundberg A. The effect of benzodiazepines on
the fetus and the newborn. Neuropediatrics. 1992;23:18–23.
107. Wojnar-Horton RE, Kristensen JH, Yapp P, et al. Methadone distribu-
79. Matalon S, Schechtman S, Goldzweig G, et al. The teratogenic effect of
tion and excretion into breast milk of clients in a methadone mainte-
carbamazepine: a meta-analysis of 1255 exposures. Reprod Toxicol.
nance programme. Br J Clin Pharmacol. 1997;44:543–547.
108. Ballard JL. Treatment of neonatal abstinence syndrome with breast
80. Quality Standards Subcommittee of the American Academy of Neu-
milk containing methadone. J Perinat Neonatal Nurs. 2002;15:76–85.
rology. Practice parameter: management issues for women with epi-
109. Ballard JL, D'Apolito K. Shortened length of stay for neonatal absti-
lepsy. Neurology 1998;51:944–948.
nence syndrome from methadone using mother's milk as therapy.
81. Scolnik D, Nulman I, Rovet J, et al. Neurodevelopment of children
Pediatr Res 2001;49:354A.
exposed in utero to phenytoin and carbamazepine monotherapy. JAMA.
110. Wojnar-Horton RE, Kristensen JH, Yapp P, et al. Methadone distribu-
tion and excretion into breast milk of clients in a methadone mainte-
82. Reitnauer PJ, Callanan NP, Farber RA, et al. Prenatal exposure to
nance programme. Br J Clin Pharmacol. 1997;44:543–547.
disulfiram implicated in the cause of malformations in discordant
111. Begg EJ, Malpas TJ, Hackett LP, et al. Distribution of R- and S-
monozygotic twins. Teratology. 1997;56:358–362.
methadone into human milk during multiple, medium to high oral
83. Nora AH, Nora JJ, Blu J. Limb-reduction anomalies in infants born to
dosing. Br J Clin Pharmacol. 2001;52:681–685.
disulfiram-treated alcoholic mothers. Lancet. 1977;2:664.
112. Blinick G, Inturrisi CE, Jerez E, et al. Methadone assays in pregnant
84. Helmbrecht GD, Hoskins IA. First trimester disulfiram exposure: report
women and progeny. Am J Obstet Gynecol. 1975;121:617–621.
of two cases. Am J Perinatol. 1993;10:5–7.
113. Committee on Drugs, American Academy of Pediatrics. The transfer of
85. Hulse G, O'Neil G. Using naltrexone implants in the management of
drugs and other chemicals into human breast milk. Pediatrics 2001;
the pregnant heroin user. Aust N Z J Obstet Gynaecol. 2002;42:569–
114. The WHO Working Group, Bennet PN, ed. Monographs on individual
86. Hulse GK, O'Neill G, Pereira C, et al. Obstetric and neonatal outcomes
drugs (WHO Working Group). In: Drugs and Human Lactation. Am-
associated with maternal naltrexone exposure. Aust N Z J Obstet
sterdam: Elsevier; 1988:319–320.
115. Boysen K, Hertel S, Chraemmer-Jorgensen B, et al. Buprenorphine
87. Johnson BA, Ait-Daoud N. Neuropharmacological treatments for al-
antagonism of ventilatory depression following fentanyl anesthesia.
coholism: scientific basis and clinical findings. Psychopharmacology
Acta Anaesthesiol Scand. 1988;32:490–492.
116. Jernite M, Viville B, Escande B, et al. [Buprenorphine and pregnancy.
88. Maura S, Resemble A. Leaving methadone treatment: lessons learned,
Analysis of 24 cases]. Arch Pediatr. 1999;6:1179–1185.
lessons forgotten, lessons ignored. Mt Sinai J Med. 2001;68:62–74.
117. Robinson SE, Wallace MJ. Effect of perinatal buprenorphine exposure
89. Rementeria JL, Nunag NN. Narcotic withdrawal in pregnancy: still-
on development in the rat. J Pharmacol Exp Ther. 2001;298:797–804.
birth incidence with a case report. Am J Obstet Gynecol. 1973;116:
118. Johnson RE, Jones HE, Fischer G. Use of buprenorphine in pregnancy:
patient management and effects on the neonate. Drug Alcohol Depend.
90. Zuspan FP, Gumpel JA, Mejia-Zelaya A, et al. Fetal stress from
2003;70 (2 Suppl):S87–S101.
methadone withdrawal. Am J Obstet Gynecol. 1975;122:43–46.
119. Loustauneau A, Auriacombe M, Daulouede JP, et al. Is buprenorphine
91. Dashe JS, Jackson GL, Olscher DA, et al. Opioid detoxification in
a potential alternative to methadone for treating pregnant drug users?
pregnancy. Obstet Gynecol. 1998 92:854–858.
Inventory of clinical data in the literature [in French]. Ann Med Interne
92. Maas U, Kattner E, Weingart-Jesse B, et al. Infrequent neonatal opioid
(Paris). 2002;153 (7 Suppl):2S31–2S36.
withdrawal following maternal methadone detoxification during preg-
120. Schindler SD, Eder H, Ortner R, et al. Neonatal outcome following
nancy. J Perinat Med. 1990;18:111–118.
buprenorphine maintenance during conception and throughout preg-
93. Rosen TS, Johnson HL. Children of methadone-maintained mothers:
nancy. Addiction. 2003;98:103–110.
follow-up to 18 months of age. J Pediatr. 1982;101:192–196.
121. Lejeune C, Aubisson S, Simmat-Durand L, et al. Withdrawal syn-
94. van Baar AL, Fleury P, Soepatmi S, et al. Neonatal behavior after drug
dromes of newborns of pregnant drug abusers maintained under meth-
dependent pregnancy. Arch Dis Child. 1989;64:235–240.
adone or high-dose buprenorphine: 246 cases [in French]. Ann Med
95. Lifschitz MH, Wilson GS, Smith EO, et al. Factors affecting head
Interne (Paris). 2001;152 (Suppl 7):21–27.
growth and intellectual function in children of drug addicts. Pediatrics
122. Eder H, Rupp I, Peternell A, et al. [Buprenorphine in pregnancy].
Psychiatr Prax. 2001;28:267–269.
96. Hans SL. Developmental consequences of prenatal exposure to meth-
123. Annitto WJ. Detoxification with buprenorphine of a pregnant heroin
adone. Ann N Y Acad Sci. 1989;562:195–207.
addict. Am J Addict. 2000;9:92–93.
2008 American Society of Addiction Medicine
Helmbrecht and Thiagarajah
J Addict Med • Volume 2, Number 1, March 2008
124. Johnson RE, Jones HE, Jasinski DR, et al. Buprenorphine treatment of
seeking by GABA B receptor agonists baclofen and CGP44532 but not
pregnant opioid– dependent women: maternal and neonatal outcomes.
the GABA reuptake inhibitor tiagabine in baboons. Drug Alcohol
Drug Alcohol Depend. 2001;63:97–103.
125. Johnson RE, Jones HE, Fischer G. Use of buprenorphine in pregnancy:
139. Lhuillier L, Mombereau C, Cryan JF, et al. GABA(B) receptor-positive
patient management and effects on the neonate. Drug Alcohol Depend.
modulation decreases selective molecular and behavioral effects of
2003;70 (2 Suppl):S87–S101.
126. Nanovskaya T, Deshmukh S, Brooks M, et al. Transplacental transfer
140. Shoptaw S, Yang X, Rotheram-Fuller EJ, et al. Randomized placebo-
and metabolism of buprenorphine. J Pharmacol Exp Ther. 2002;300:
controlled trial of baclofen for cocaine dependence: preliminary effects
for individuals with chronic patterns of cocaine use. J Clin Psychiatry.
127. Deshmukh SV, Nanovskaya TN, Ahmed MS. Aromatase is the major
enzyme metabolizing buprenorphine in human placenta. J Pharmacol
141. Delhaas EM, Verhagen J. Pregnancy in a quadriplegic patient treated
Exp Ther. 2003;306:1099–1105.
with continuous intrathecal baclofen infusion to manage her severe
128. Marquet P, Chevrel J, Lavignasse P, et al. Buprenorphine withdrawal
spasticity. Case report. Paraplegia. 1992;30:527–528.
syndrome in a newborn. Clin Pharmacol Ther. 1997;62:569–571.
142. Czeizel AE, Tomcsik M, Timar L. Teratologic evaluation of 178
129. Viscarello RR, Ferguson DD, Nores J, et al. Limb-body wall complex
infants born to mothers who attempted suicide by drugs during preg-
associated with cocaine abuse: further evidence of cocaine's teratoge-
nancy. Obstet Gynecol. 1997;90:195–201.
nicity. Obstet Gynecol. 1992;80:523–526.
143. Eriksson M, Zetterstro¨m R. Amphetamine addiction and pregnancy II.
130. Chavez GF, Mulinare J, Cordero JF. Maternal cocaine use and the risk
Pregnancy, delivery and the neonatal period. Socio-medical aspects.
for genitourinary tract defects: an epidemiologic approach. Am J
Acta Obstet Gynecol Scand. 1981;60:253–259.
Human Genetics. 1988;43:A43.
144. Eriksson M, Zetterstrom R. Amphetamine addiction during pregnancy:
131. Hoyme HE, Jones KL, Dixon SD, et al. Prenatal cocaine exposure and
10-year follow-up. Acta Paediatr Suppl. 1994;404:27–31.
fetal vascular disruption. Pediatrics. 1990;85:743–747.
145. Cernerud L, Eriksson M, Jonsson B, et al. Amphetamine addiction
132. Neerhof MG, MacGregor SN, Retzky SS, et al. Cocaine abuse during
during pregnancy: 14-year follow-up of growth and school perfor-
pregnancy: peripartum prevalence and perinatal outcome. Am J ObstetGynecol. 1989;161:633–638.
mance. Acta Paediatr. 1996;85:204–208.
133. Woods JR Jr, Plessinger MA. Effect of cocaine on uterine blood flow
146. Jones KL, Johnson KA, Dick LM. Pregnancy outcomes after first
and fetal oxygenation. JAMA. 1987;257:957–961.
trimester exposure to phentermine/fenfluramine. Teratology. 2002;65:
134. Johnson BA. Recent advances in the development of treatments for
alcohol and cocaine dependence: focus on topiramate and other mod-
147. Stek AM, Fisher BK, Baker RS, et al. Maternal and fetal cardiovascular
ulators of GABA or glutamate function. CNS Drugs. 2005;19:873–896.
responses to methamphetamine in the pregnant sheep. Am J Obstet
135. Kampman KM, Pettinati H, Lynch KG, et al. A pilot trial of topiramate
for the treatment of cocaine dependence. Drug Alcohol Depend. 2004;
148. Stek AM, Baker RS, Fisher BK, et al. Fetal responses to maternal and
fetal methamphetamine administration in sheep. Am J Obstet Gynecol.
136. Hoyme HE, Hauck L, Quinn D. Minor anomalies accompanying
prenatal exposure to topiramate. J Investig Med. 1998;46:119A.
149. Galloway GP, Newmeyer J, Knapp T, et al. A controlled trial of
137. Morrow J, Russell A, Guthrie E, et al. Malformation risks of antiepi-
imipramine for the treatment of methamphetamine dependence. J Subst
leptic drugs in pregnancy: a prospective study from the UK epilepsy
Abuse Treat. 1996;13:493–497.
and pregnancy register. J Neurol Neurosurg Psychiatry. 2006;77:193–
150. Brodie JD, Figueroa E, Laska EM, et al. Safety and efficacy of
gamma-vinyl GABA (GVG) for the treatment of methamphetamine
138. Weerts EM, Froestl W, Kaminski BJ, et al. Attenuation of cocaine-
and/or cocaine addiction. Synapse 2005;55:122–125.
2008 American Society of Addiction Medicine
Source: http://obgyn.med.wayne.edu/pdf/helmbrecht_addiction_pregnancy.pdf
Inlacin® Therapy in Patients with Type-2 Diabetes Mellitus (The Prospective Surabaya-Inlacin® Study) Askandar Tjokroprawiro Sri Murtiwi Surabaya Diabetes and Nutrition Center – Dr. Soetomo Teaching Hospital Faculty of Medicine Airlangga University, Surabaya Prospective study on DLBS3233 (Inlacin®) which is called Surabaya-Inlacin® Study (SIS) has been per-
Managing Drug Interactions in the Treatment of National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention Division of Tuberculosis Elimination Managing Drug Interactions in the Treatment of Centers for Disease Control and Prevention Office of Infectious Diseases National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention Division of Tuberculosis Elimination