Kamagra gibt es auch als Kautabletten, die sich schneller auflösen als normale Pillen. Manche Patienten empfinden das als angenehmer. Wer sich informieren will, findet Hinweise unter kamagra kautabletten.
Salivary testosterone, cortisol, and progesterone: two-week stability, interhormone correlations, and effects of time of day, menstrual cycle, and oral contraceptive use on steroid hormone levels

Physiology & Behavior 99 (2010) 8–16
Contents lists available at
Physiology & Behavior
Salivary testosterone, cortisol, and progesterone: Two-week stability, interhormonecorrelations, and effects of time of day, menstrual cycle, and oral contraceptive useon steroid hormone
Scott H. Liening ,Steven J. Stanton Ekjyot K. Saini Oliver C. Schultheiss a Department of Psychology, University of Texas at Austin, 1 University Station A8000, Austin, TX 78705, USAb Duke University, USAc University of Michigan, Ann Arbor, USAd Friedrich-Alexander University, Erlangen, Germany
With salivary assessment of steroid hormones increasing, more work is needed to address fundamental
Received 24 June 2009
properties of steroid hormone levels in humans. Using a test–retest design and radioimmunoassay
Received in revised form 19 September 2009
assessment of salivary steroids, we tested the reliability of testosterone, cortisol, and progesterone levels
Accepted 2 October 2009
across two weeks, as well as the effects of oral contraceptives, menstrual cycle phase, and time of day onsteroid hormone levels. Testosterone and cortisol were found to be highly reliable in both sexes.
Progesterone was found to be reliable after collapsing across sex. Oral contraceptive use was associated with
lower levels of testosterone, but did not affect cortisol. Contrary to expectations, oral contraceptives also did
not affect progesterone. Menstrual cycle was found to affect levels of progesterone, but not testosterone or
cortisol. Time of day had an effect on cortisol, on progesterone only at one testing time, and no effect on
testosterone. We explored the interhormone correlations among testosterone, progesterone, and cortisol. All
three hormones were positively correlated with one another in men. In women, progesterone was positively
correlated with testosterone and cortisol, but testosterone and cortisol were uncorrelated.
2009 Elsevier Inc. All rights reserved.
Oral contraceptivesMenstrual cycleTime of day
what they are interpreted as representing (e.g. baseline measure-ments are reliable and relatively stable, individual differences in basal
The ability to obtain valid measures of bioactive steroid hormones
levels are reasonably static, etc.).
from human saliva has led to an increase in the use of hormones in
Currently, there is a dearth of research on the stability of steroid
psychological research. This increased attention on salivary hormones
hormone levels in human populations. In order for psychologists to
has raised issues heretofore not thoroughly addressed in the human
use salivary steroid hormones as a trustworthy assessment, research
literature, specifically the stability of basal hormone levels over time.
into the reliability of these assessments is essential. Just as self-report
The influence of interhormone relationships circadian rhythms
questionnaires are subject to thorough psychometric testing
menstrual cycle , and the use of oral contraceptives on
(e.g. ), salivary assessments of hormones must be subject to
endogenous salivary hormone levels have all been researched on their
the same scrutiny if they are to be used as markers of stable properties
own, but their impact on the stability of basal steroid levels has been
of individuals' endocrine systems. To date, only two studies have
mostly neglected. With the increased use of salivary steroid hormones
specifically addressed the stability of salivary testosterone in an adult
in psychological research, more basic research is needed to assure
population . Both studies found testosterone to be highly
researchers that salivary assessments of hormones actually represent
reliable over a variety of time periods, but neither took intoconsideration important factors that could potentially influencesteroid hormone levels. While Dabbs examined the stability of
☆ "Stability" here refers to the consistency of basal levels of endogenous hormones
testosterone levels over a variety of time periods, oral contraceptive
over time. Other fields may refer to this same effect as "reproducibility," but in the
use was not considered, and reliability was calculated after collapsing
context of the current study we use "stability" to refer to the consistency of hormone
across sex, which is problematic given the large differences between
levels across assessment periods over time.
men and women's testosterone levels Sellers et al. tested the
⁎ Corresponding author. Tel.: +1 512 471 0691; fax: +1 512 471 6175.
E-mail address: (S.H. Liening).
stability of testosterone without consideration of time of day,
0031-9384/$ – see front matter 2009 Elsevier Inc. All rights reserved.
doi:
S.H. Liening et al. / Physiology & Behavior 99 (2010) 8–16
menstrual cycle, or oral contraceptive use. Both studies examined
were recruited via flyers posted in campus buildings, and contacted
testosterone in isolation, without measuring any other steroid
the experimenters through an email address provided on the flyer.
hormones, such as cortisol or progesterone.
The experimenters scheduled two sessions for the participants to
The primary use of cortisol in psychological research has been as a
come to the lab to participate in the study. The session dates were
biomarker of the stress response and most research on the
scheduled exactly 14 days apart with each data collection session
stability of cortisol has focused on the reliability of cortisol levels in
taking place at the exact same time of day, though time of day of
the morning (e.g. and the reliability of its diurnal pattern
participation varied between participants. The study had received
Though the morning reliability of cortisol and its response to
approval from the Institutional Review Board at the University of
stressors has been thoroughly studied, there is very little research on
Michigan prior to data collection, and all participants provided
the stability of salivary cortisol levels in an adult population, and the
informed consent at the time of participation.
little research that has been conducted has generally focused on
From the initial pool of participants, ten did not return for the second
methodological sources of variability in cortisol levels . This
part of the study and two participants' data were lost due to a
limited previous research has found cortisol to be somewhat less
programming error. All were dropped from analysis. To account for
stable than other steroid hormones. For instance, Pearson correlation
daily fluctuations in hormone levels due to circadian rhythms nine
coefficients ranging from 0.20 to 0.25 were found when testing
participants whose second session was completed at a different time of
cortisol levels over a six week time span .
day (range: 9:30 am to 4:00 pm) were dropped from the analysis. An
Unlike testosterone and cortisol, progesterone is a generally under-
additional 22 participants' data were not included in the analysis due to
studied steroid hormone in the context of human social behavior,
unavailability of hormone data (e.g. insufficient or contaminated saliva
though recent work has started to explore its role in affiliation
sample). Of the remaining 79 participants constituting the final
motivation and social closeness (e.g. The majority of research
participant pool, 55 were women and 24 were men, with a mean age
on the fundamentals of salivary progesterone levels has been conducted
of 19.7 years, and 60.8% self-identified as Caucasian, 29.1% Asian, 3.8%
in children, and focused almost solely on circadian rhythms, not the
African-American, 2.5% Pacific Islander, and 3.8% other or mixed ethnic
stability of progesterone over varying time periods There is some
groups. From this pool, a few participants were not included in all
research on the relationship between progesterone and behavior, but no
analyses due to the unavailability of hormone data for each of the three
tests of the basic stability of basal progesterone levels in an adult
hormones (e.g. insufficient saliva sample for all assays). The progesterone
population. Thus, all three steroid hormones that we have discussed are
analyses included 74 participants (53 women and 21 men), the
used in psychological research, but all three lack sufficient research to
testosterone analyses included 75 participants (52 women and 23
establish that they are stable enough to warrant their use as dispositional
men), and the cortisol analyses included 76 participants (53 women and
Above and beyond a need to document the stability of steroid
hormones, a more nuanced understanding of key contributing factors
2.2. Procedure and design
to variations in hormone levels, as well as how levels of salivaryhormones are interrelated, is critical. Previous research has shown
The study had a test–retest design, with two data collection
that among female research participants, factors such as phase of
sessions spaced 14 days apart. At both testing sessions, participants
menstrual cycle, use of oral contraceptives, and relationship status can
came into the lab to complete a battery of measures assessing
all affect steroid hormone levels and their relationship with
participants' mood, personality and cognitive functioning, and to
psychological constructs . Previous research has also shown
provide saliva samples for hormone analysis (see for a report on
that there is a complex and dynamic relationship between endocrine
the findings related to personality). Participants also completed a
axes. The antagonistic relationship between the hypothalamic–
demographic questionnaire regarding age, sex, ethnicity, and infor-
pituitary–adrenal (HPA) and hypothalamic–pituitary–gonadal (HPG)
mation that could impact the viability of the saliva sample (e.g.
axes, responsible for the situational release of cortisol and testoster-
whether he/she smokes, how long since he/she brushed his/her teeth,
one, respectively, has been well-established , but the nature of
how long since he/she consumed caffeine). Female participants also
interhormonal dynamics in humans requires more research. These
provided information regarding the date of the onset of their most
dynamics are especially poorly understood outside of the cortisol–
recent menstrual cycle, the average length of their menstrual cycle,
testosterone relationship. For instance, very few studies have
and whether or not they were currently using oral contraceptives.
examined the relationship between salivary cortisol and progesterone
Participants completed personality measurements, questionnaires,
, and we are unaware of any studies reporting the relationship
and provided samples using computerized instruction, though an
between salivary testosterone and progesterone.
experimenter was present to oversee data collection.
The purpose of the present study was to provide foundational
knowledge regarding the stability of three steroid hormones in both
2.3. Salivary sampling
sexes over a two-week time span. We measured and tested thestability of testosterone, cortisol, and progesterone over a two-week
For each of the saliva samples, participants used a stick of sugar-free
time period, as well as examined the effects of the menstrual cycle and
chewing gum to stimulate saliva flow and collected up to 7.5 mL of saliva
oral contraceptive use, which were expected to affect progesterone
in a sterile polypropylene vial. They discarded the chewing gum after
levels in particular, on female participants' salivary levels of all three
each saliva collection . Participants' collection vials were sealed
hormones. Finally, intercorrelations between the three hormones
immediately after each collection and placed in frozen storage in
were explored in an attempt to further understand the hormones'
accordance with previous research on sample storage . Samples
relationships to one another.
were freed from mucopolysaccarides and other residuals by threefreeze–thaw cycles followed by centrifugation.
2.4. Assay procedure
2.1. Participants
Salivary hormone levels were assessed with solid-phase Coat-A-
One hundred and twenty two students enrolled at the University
Count125I radioimmunoassays for testosterone (TKTT), cortisol
of Michigan, Ann Arbor participated in the two-session study, with
(TKCO), and progesterone (TKPG) provided by Diagnostic Products
data collection sessions spaced exactly 14 days apart. Participants
Corporation (Los Angeles, CA). To determine salivary hormone
S.H. Liening et al. / Physiology & Behavior 99 (2010) 8–16
Table 1Assay characteristics for testosterone, cortisol, and progesterone assays.
Control levels (RCs)
Inter-assay CV (%)
Analytical sensitivity
90 pg/mL (97.39%)
152 pg/mL (94.91%)
1.5 ng/mL (114.89%)
3.5 ng/mL (109/26%)
27 pg/mL (101.19%)
101 pg/mL (100.89%)
Note: Inter-assay CVs based on control samples; Intra-assay CVs based on participant samples; RC = recovery coefficient; CV=coefficient of variation; Analytical Sensitivy=B0−3SD.
concentrations, we prepared water-based dilutions of all standards
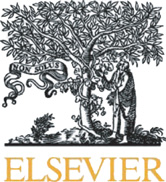
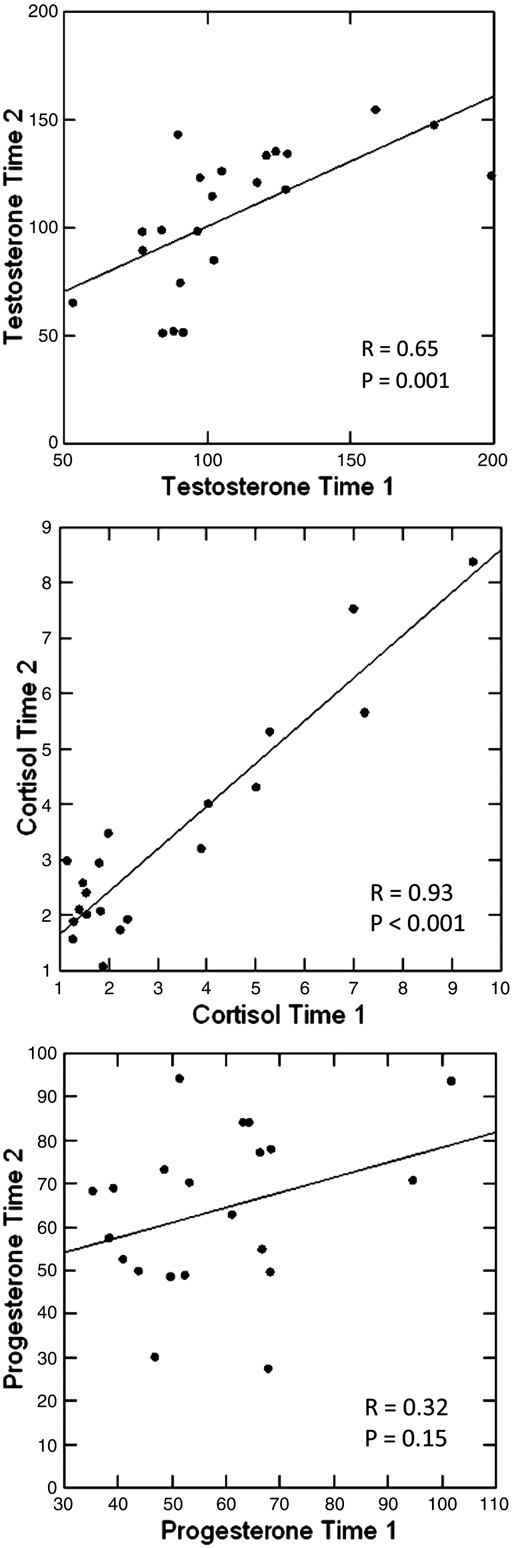
whereas the stability coefficient for progesterone, although positive,
and controls. 400 μL of the saliva samples, standards, and controls
failed to reach significance (P = 0.15; see We found that the
were pipetted into antibody-coated tubes. For progesterone, 1 mL
raw cortisol and progesterone levels were slightly skewed for men, so
radio-labeled tracer was added to each tube at this point. All tubes
we also transformed men's raw cortisol and progesterone scores and
were allowed to incubate overnight. For testosterone and cortisol,
reran the regressions of Time 2 on Time 1. A regression of Time 2 log-
1 mL radio-labeled tracer was added to each tube following overnight
transformed cortisol on Time 1 log-transformed cortisol revealed a
incubation, and then all tubes were again incubated overnight. Finally,
highly significant positive correlation (R = 0.75, P < 0.001). A regres-
tubes were aspirated and counted for 3 min . Assay reliability
sion of Time 2 squareroot-transformed progesterone on Time 1
was evaluated by including control samples with known hormone
squareroot-transformed progesterone failed to reveal a significant
concentrations in each assay (Bio-Rad Lyphochecks from Bio-Rad
relationship (R = 0.29, P = 0.22). reports the correlations
Laboratories, Hercules, CA).
between all hormones at both collection times for men.
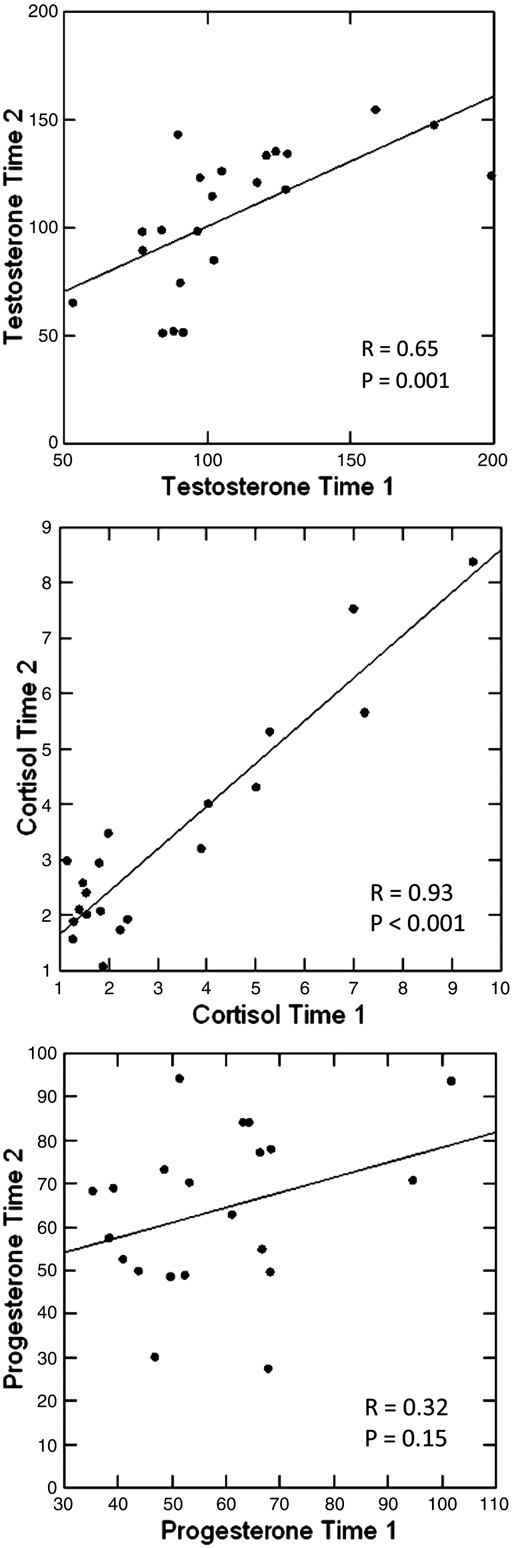
3.3. Reliability — women
Information regarding effective ranges, controls, CVs, and analytical
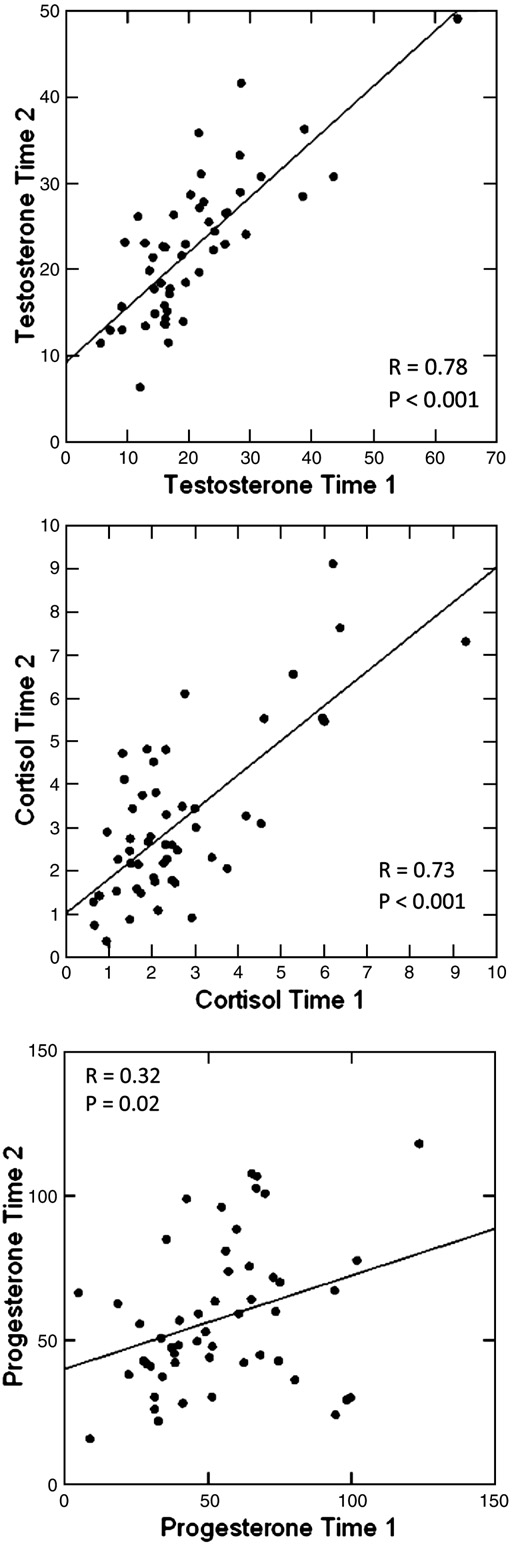
shows scatterplots depicting female subjects' steroid hormone
sensitivity for assays performed on the present study's saliva samples is
levels at Time 2 as a function of Time 1. Similar to the findings in men,
provided in . Sample characteristics for salivary testosterone,
stability coefficients for testosterone and cortisol were high and
progesterone and cortisol are listed in . reports the means
significant. The stability coefficient for progesterone was lower but
and standard deviations of each hormone for both normally-cycling
reached significance among female participants (see ). We found
women and women taking oral contraceptives.
that the raw cortisol and progesterone were slightly skewed for women,so we also transformed women's raw cortisol and progesterone scores
3.1. Statistical analysis
and reran the regressions of Time 2 on Time 1. A regression of Time 2log-transformed cortisol on Time 1 log-transformed cortisol revealed a
Reliability was tested using linear regressions. For each regression
highly significant positive correlation (R=0.67, P<0.001). A regression
conducted, Pearson's correlation coefficient (R) is reported as a
of Time 2 squareroot-transformed progesterone on Time 1 squareroot-
measure of effect size, and is referred to as a "stability coefficient"
transformed progesterone revealed a significant positive correlation
when discussing the reliability of hormone levels. Regression analysis
(R = 0.32, P = 0.02). reports the correlations between all
was also used to test the effects of menstrual cycle and time of day.
hormones at both collection times for women.
Again, Pearson's correlation coefficient (R) is reported as a measure ofeffect size. ANOVAs were used to compare hormone levels between
3.4. Progesterone reliability
sexes and between normally-cycling women and women using oralcontraceptives, and corresponding Fs are reported.
We suspected that the lack of progesterone stability among males
was due to low statistical power. After checking to make sure there
3.2. Reliability — men
was not a significant difference in progesterone levels between thesexes at either time point (both Fs < 1.0), we collapsed across sex to
shows scatterplots depicting male subjects' steroid hormone
retest progesterone reliability. A regression of Time 2 progesterone on
levels at Time 2 as a function of Time 1 hormone levels. Stability
Time 1 progesterone revealed a highly significant positive correlation
coefficients for testosterone and cortisol were high and significant,
(R = 0.33, P = 0.005). A regression of Time 2 squareroot-transformed
Salivary progesterone (pg/mL), testosterone (pg/mL), cortisol (ng/mL) concentrations
Salivary progesterone (pg/mL), testosterone (pg/mL), cortisol (ng/mL) concentrations
at collection days 1 and 2 for women taking oral contraceptives and normally-cycling
at collection days 1 and 2 for men and women.
Oral Contraceptives
S.H. Liening et al. / Physiology & Behavior 99 (2010) 8–16
Table 4Correlations between progesterone (pg/mL), testosterone (pg/mL), cortisol (ng/mL)concentrations at collection days 1 and 2 for women (below the diagonal) and men(above the diagonal).
⁎ P≤0.10.
⁎⁎ P≤0.05.
⁎⁎⁎ P≤0.01.
either Time 1 (F(1, 50) = 0.26, P = ns) or Time 2 (F(1, 49) = 0.24,P = ns). Progesterone was also not significantly different at Time 1(F(1,50) = 1.34, P = ns) or Time 2 (F(1,50) = 0.79, P = ns). Thoughthe differences in progesterone were nonsignificant, they were in thepredicted direction (i.e. normally-cycling women had higher levels ofprogesterone than women taking oral contraceptives).
It is reasonable to expect the differences in hormone levels
attributable to oral contraceptive use to change over the course of themenstrual cycle (e.g. the difference in progesterone levels will be greaterduring progesterone surge experienced by normally-cycling womenduring the luteal phase). The interaction of day of menstrual cycle andoral contraceptive use was entered into a multiple regression predictinghormone levels. The interaction was nonsignificant for all threehormones at both time points (all ts < 1.5, Ps = ns), indicating that theeffect of oral contraceptive use on hormone levels did not change as afunction of the menstrual cycle.
When adding oral contraceptive use into the regression model to test
if stability changed as a function of oral contraceptive use, the effect oforal contraceptives on stability was nonsignificant for both testosteroneand progesterone (both F-Changes < 0.1). Oral contraceptive use wasfound to significantly affect cortisol (F-Change=6.92, P=0.01), suchthat women using oral contraceptives had a higher stability coefficient(R = 0.81, P < 0.01) than normally-cycling women (R = 0.75, P < 0.01).
But when the analysis was rerun using log-transformed cortisol, it wasno longer significant (F-Change=2.52, P=0.14).
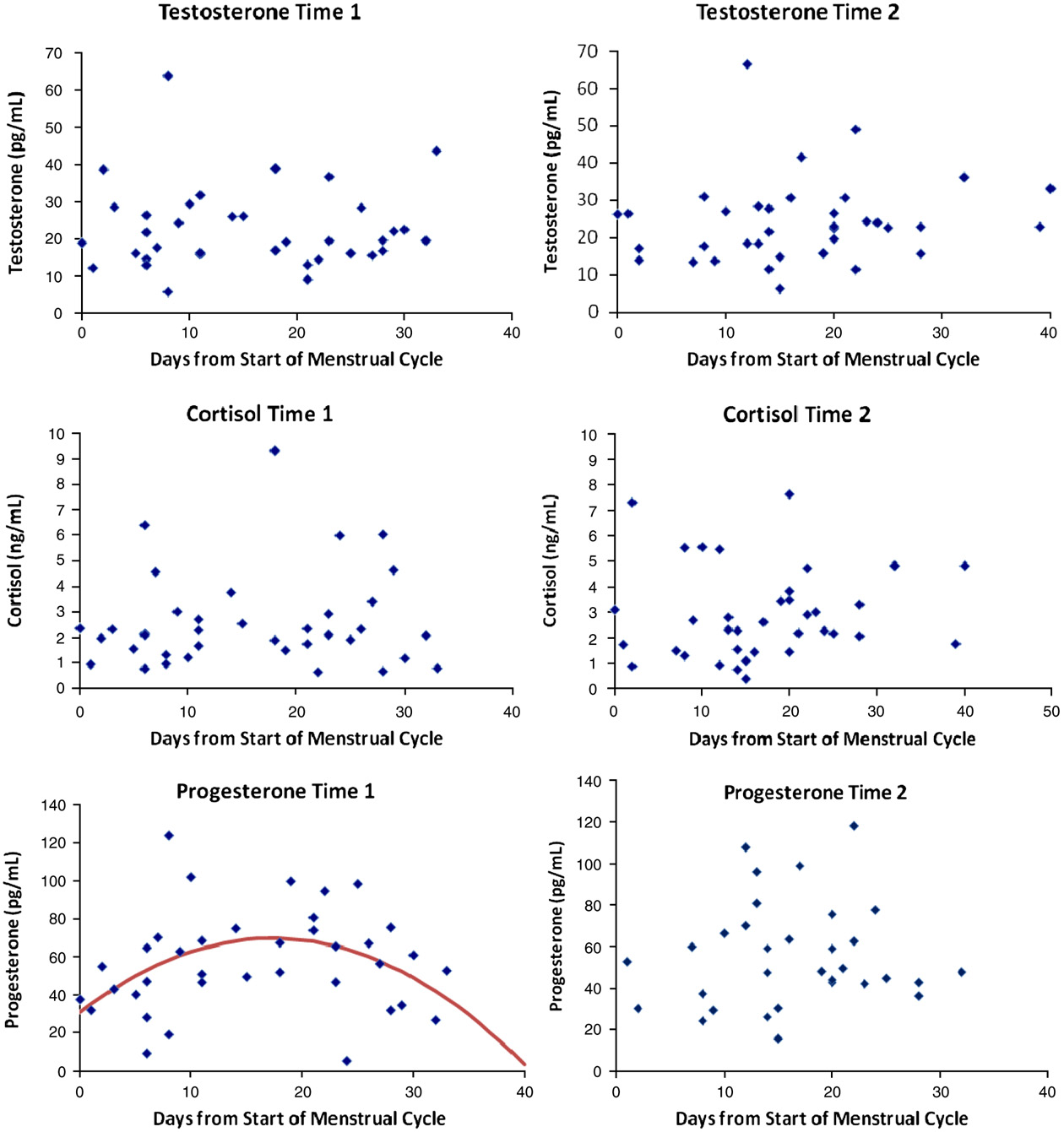
3.6. Effects of day of menstrual cycle on hormone levels fornormally-cycling women
Estimated day of menstrual cycle was calculated from the
information that female participants provided on the demographicquestionnaire. The self-reported date of menstrual cycle onset wassubtracted from the date of participation to determine the day ofmenstrual cycle when the first saliva sample was obtained. Day of
Fig. 1. Reliability between collection day 1 and day 2 for men's testosterone (pg/mL),
menstrual cycle at Time 2 was calculated by adding 14 days to the day
cortisol (ng/mL), and progesterone (pg/mL).
of menstrual cycle at Time 1, using self-reported average cycle lengthto account for those participants who had begun a new cycle between
progesterone on Time 1 squareroot-transformed progesterone
the two collection dates.
yielded a similar result (R = 0.32, P = 0.006).
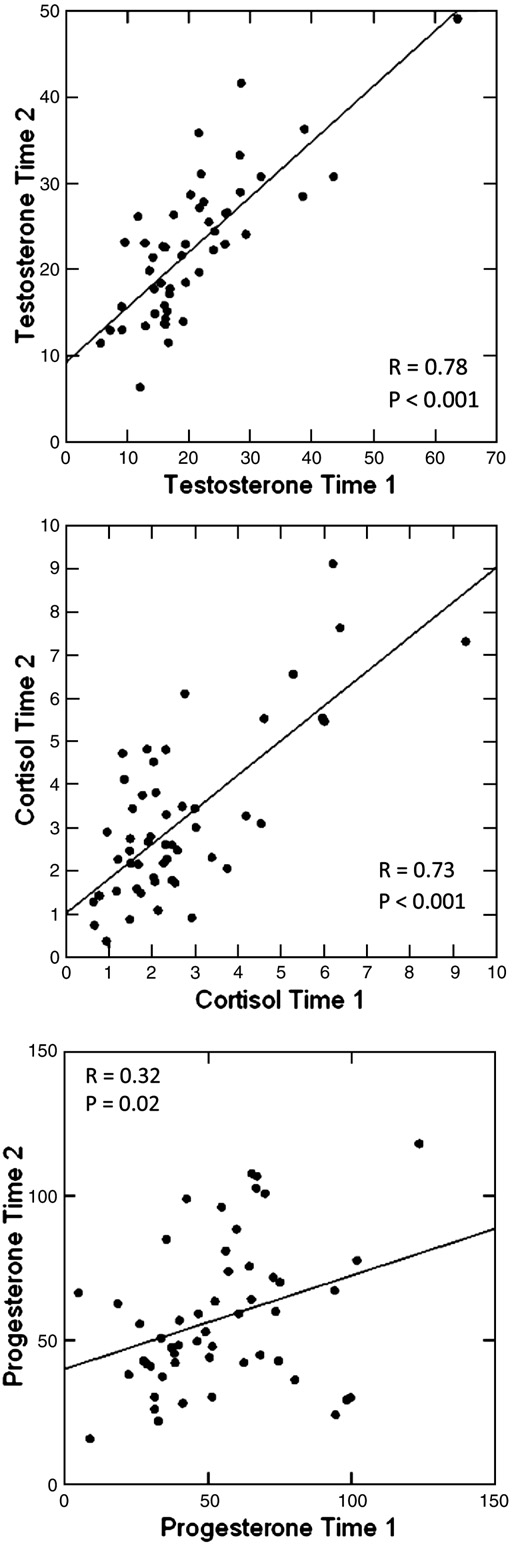
A quadratic regression model testing the effect of menstrual cycle on
progesterone levels among normally-cycling women was significant at
3.5. Effects of oral contraceptive use on salivary steroids in women
Time 1 (R = 0.40, P = 0.02). Due to Time 2 menstrual cycle estimatesbeing derived from calculations based on Time 1 measurements rather
Women taking oral contraceptives had significantly lower levels of
than actual Time 2 measurements, three data points that appear to be
endogenous testosterone at Time 1 (F(1, 48) = 5.34, P = 0.03), but not
part of an abnormally long cycle length (i.e. over 39 days) were dropped
at Time 2 (F(1, 48) = 1.24, P = ns). Women taking oral contraceptives
from the analysis. A quadratic model testing the effect of menstrual cycle
did not have significantly different levels of endogenous cortisol at
on progesterone levels was not significant at Time 2 (R=0.14, P=ns). A
S.H. Liening et al. / Physiology & Behavior 99 (2010) 8–16
terone and cortisol (both F-Changes < 1.0). There was a significanteffect of menstrual cycle on progesterone among normally-cyclingwomen (F-Change = 3.93, P = 0.06). This effect appeared to be drivenby a single outlier. When that data point was removed, the effectdropped to nonsignificance (F-Change = 1.65, P = 0.21).
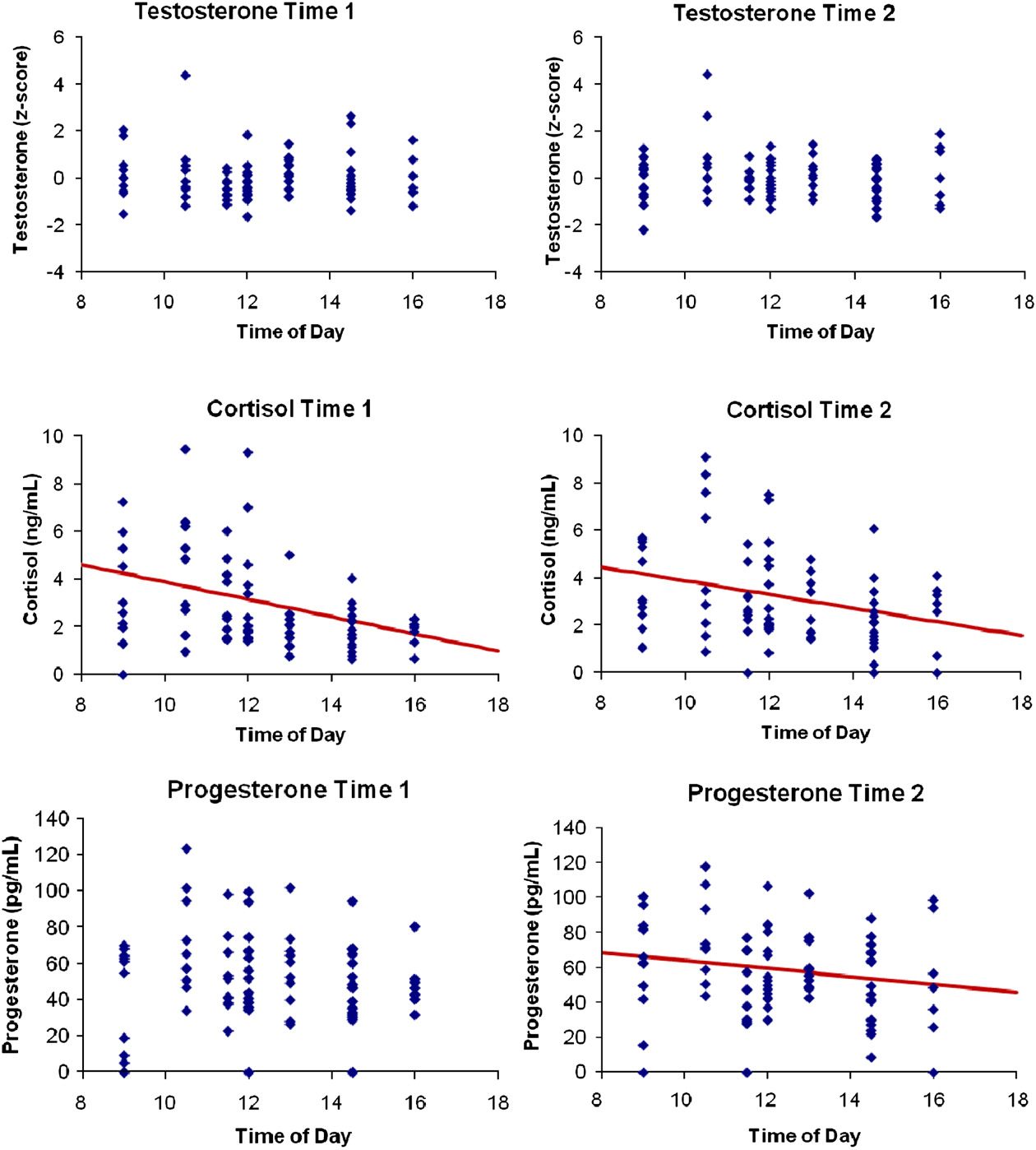
3.7. Effects of time of day on salivary steroids
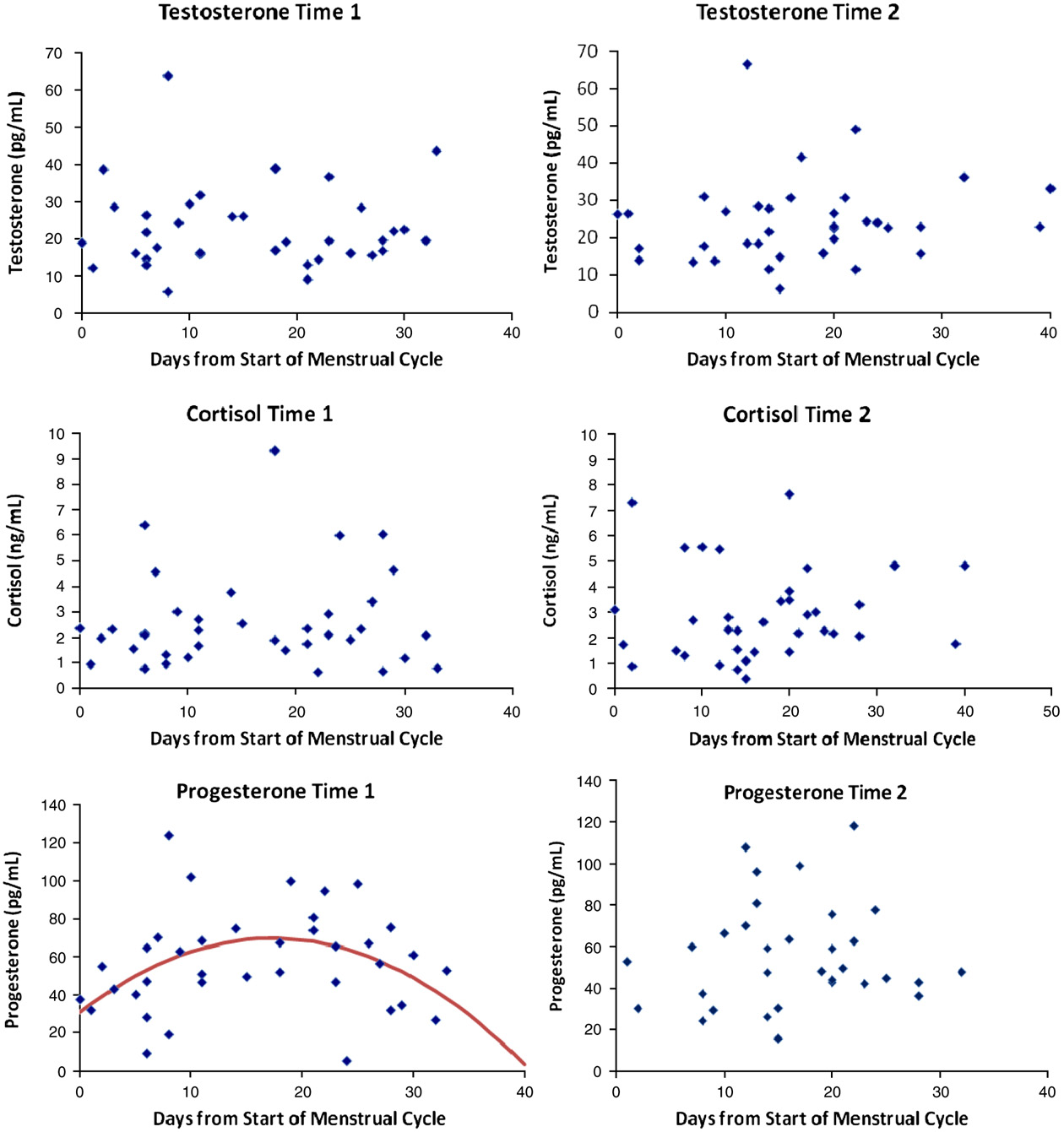
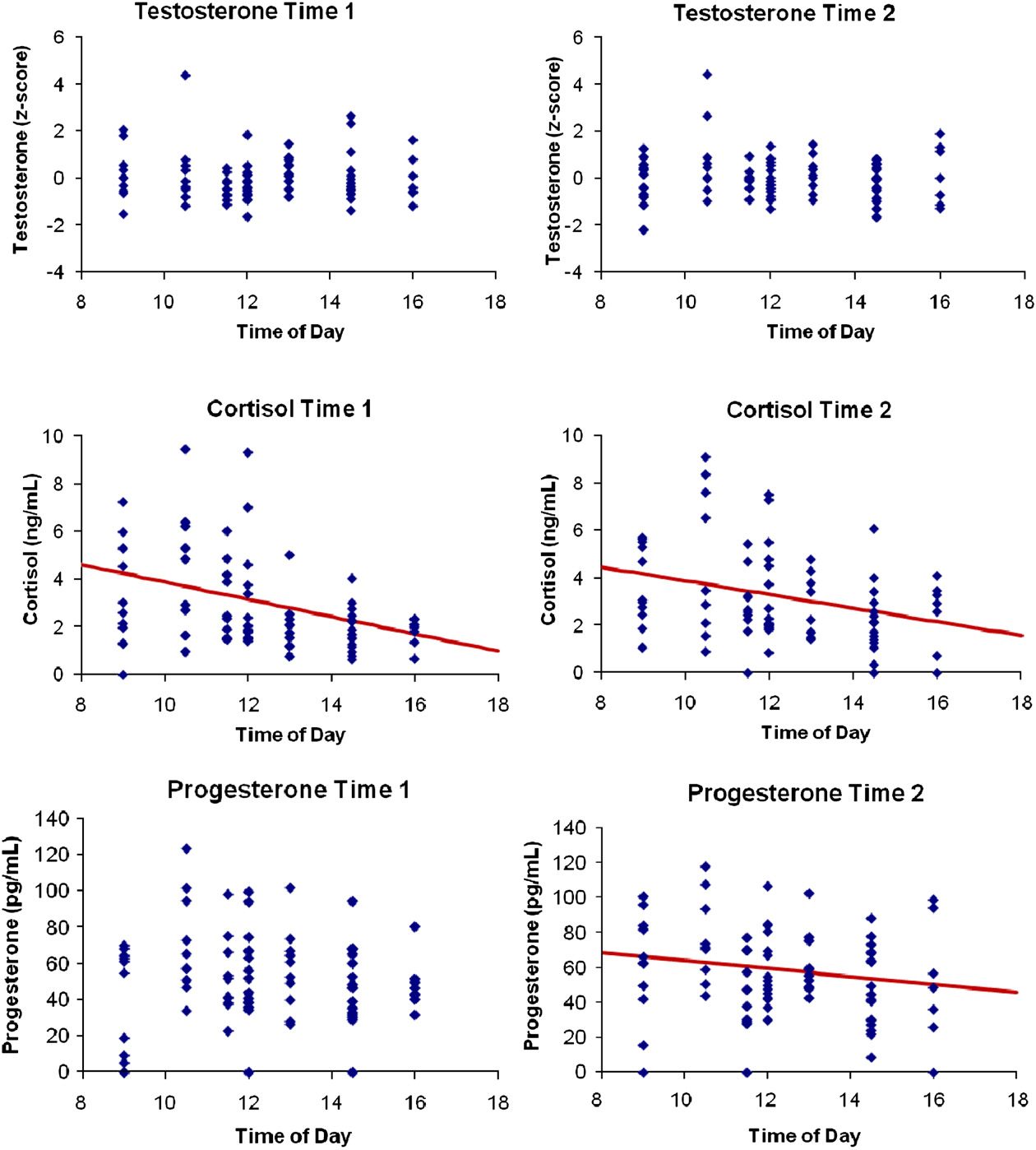
contains scatterplots of hormone levels against time of day of
assessment, as well as any significant regression models for effects oftime of day on hormone levels. There were no effects of time of day ontestosterone levels, either when analyzed separately by sex or whenstandardized and collapsed across sex. Since there was no significantdifference in cortisol levels between sexes at either time point (bothFs < 1.2), cortisol was collapsed across sex. A regression testing theeffects of time of day on cortisol revealed a significant relationship atTime 1 (R = −0.39, P<0.001), as well as Time 2 (R=−0.30, P=0.01),such that participants tested in the morning had higher cortisol levelsthan those tested later in the day. Because residuals were not normallydistributed, the analysis was rerun using log-transformed cortisol.
Assumptions were met and the effect remained significant at both Time1 (R = −0.41, P<0.001) and Time 2 (R=−0.29, P=0.01). Since thereis no significant difference in progesterone levels between the sexes ateither time point (both Fs < 1.0), progesterone was collapsed across sex.
There was no significant effect of time of day on progesterone at Time 1,but there was a significant effect at Time 2 (R=−0.22, P=0.06), suchthat those participants tested in the morning had higher progesteronelevels than those tested later in the day.
Time of day of assessment was added to the regression model to
test if stability changed as a function of when during the dayparticipants provided saliva samples. The effect of time of day onstability was nonsignificant for all three hormones for both sexes (allF-Changes < 2, Ps = ns).
3.8. Intercorrelations of hormones
shows the intercorrelations of all hormones for each sex at
both collection times. Progesterone and testosterone were signifi-cantly correlated at both time points for men but only at Time 2 forwomen. Progesterone and cortisol were significantly correlated atTime 1 but not Time 2 for men, and were significantly correlated atTime 2 but not Time 1 for women. Testosterone and cortisol werehighly correlated at Time 1 but uncorrelated at Time 2 for men, anduncorrelated at both time points for women.
The main focus of the present study was to test the stability of
salivary hormone measurements across a two-week period, as well asto examine the contributing role of other factors such as oralcontraceptive use, menstrual cycle phase, and time of day ofassessment. All hormones, with the exception of progesterone inmen, were found to be stable across a two-week period, withcorrelation coefficients ranging from R = 0.32 (progesterone in
Fig. 2. Reliability between collection day 1 and day 2 for women's testosterone (pg/mL),
women) to as high as R = 0.93 (cortisol in men). Testosterone and
cortisol (ng/mL), and progesterone (pg/mL).
cortisol, in particular, were found to be highly stable in both men andwomen, with all correlation coefficients greater than 0.65 (seeTo put this into perspective, reliability coefficients for
series of regression models testing the effect of menstrual cycle on levels
various forms of the Stroop task, a non-declarative measure of
of testosterone and cortisol among normally-cycling women were all
executive function, have been found to range from R = 0.77 to
nonsignificant at both time points (all ts≤1.5, all Ps>0.14).
R = 0.80 for a one week interval and from R = 0.46 to R = 0.93 for a
depicts endogenous levels of each hormone across days of the menstrual
two-week interval .
The presently-reported testosterone stability findings are in line
When adding day of menstrual cycle into the regression model to
with previous findings. Dabbs found the reliability of testosterone
test if stability changed as a function of menstrual cycle phase, the
to range from R = 0.64 over two days to R = 0.52 over seven to eight
effect of menstrual cycle on stability was nonsignificant for testos-
weeks, with a two-week reliability of R = 0.71, after standardizing
S.H. Liening et al. / Physiology & Behavior 99 (2010) 8–16
Fig. 3. Salivary hormone concentrations over the course of the menstrual cycle in normally-cycling women. Regression lines for significant models are included.
and collapsing across sex. Sellers et al. found the average
coefficient of similar magnitude. It is worth noting that the mean
intraclass correlations for daily measurements of testosterone over
progesterone levels in the present data are noticeably higher than
the course of five days to be R = 0.94 for men and R = 0.81 for women.
have been found in some other studies (e.g. but are in line
They also found the reliability of testosterone over a 48 h period to be
with some recent findings as well
R = 0.70 after standardizing and collapsing across sex. The current
There is the possibility that the stability coefficients may have been
findings of R=0.65 and R=0.78, for men and women respectively,
attenuated by extraneous factors, such as physical or sexual activity or
are thus comparable to previous studies.
stress. Information regarding these factors was not collected as part of
There is no previous research on the stability of salivary cortisol
the study, and previous research has found that these factors can have
and progesterone in a general adult population with which to
an impact on endogenous hormone levels
compare the present findings. Cortisol was found to be highly stable
The lack of a significant difference in progesterone levels between
in both men (R = 0.93) and women (R = 0.73). Progesterone, on the
the sexes is surprising and worth noting. Previous research has shown
other hand, was found to be considerably less stable. Progesterone
that normally-cycling women tend to have slightly higher progesterone
was significantly stable in women (R = 0.32), but nonsignificantly
levels than men generally, and significantly higher levels during the
stable in men (R = 0.32), though R values were equal. The lack of
surge in progesterone experienced by normally-cycling women in the
significance in men is due to the smaller sample size (21 men vs. 53
luteal phase It is possible that collapsing across normally-cycling
women). This is especially apparent when progesterone is collapsed
women and those using oral contraceptives washed out any effect
across sex, which yields an overall significant retest reliability
attributable to the luteal phase progesterone surge, lowering the mean
S.H. Liening et al. / Physiology & Behavior 99 (2010) 8–16
Fig. 4. Salivary hormone concentrations across collection times of day between participants for both collection time points. Regression lines for significant models are included.
progesterone levels among women to the point that they are similar to
their current menstrual cycle, and day of menstrual cycle was
those among men.
estimated by counting forward from that date to the date the saliva
The lower R values for progesterone, compared to testosterone
sample was provided. Day of menstrual cycle at Time 2 was estimated
and cortisol, could also be attributed to two additional factors. First,
by adding 14 days to the Time 1 estimation and using self-reported
progesterone in men is produced by the adrenal glands, but possibly
average cycle length to account for those participants who had started
as a byproduct of other adrenal functions, rather than a primary
a new cycle between collection dates. Given the variability of overall
function. Second, the low stability of progesterone in women could be
cycle lengths and specifically the lengths of both the follicular and the
attributed to the well-established individual changes in progesterone
luteal phase , this inexact estimation process should be kept in
levels over the menstrual cycle There was a significant effect of
mind when considering the reported effects of menstrual cycle on
menstrual cycle phase on progesterone levels in the present data (see
hormone levels.
), and the lower stability of progesterone among women is most
In Schultheiss et al.'s study on the impact of menstrual cycle
likely due to this effect.
phase and oral contraceptive use on steroid hormone levels in saliva,
It is worth noting that day of menstrual cycle was only an
testosterone levels were significantly lower in women using oral
estimation. Female participants self-reported the date of the onset of
contraceptives, matching other research that found the same effect
S.H. Liening et al. / Physiology & Behavior 99 (2010) 8–16
As with previous research, the present study found women
These findings are partially consistent with previous research that found
using oral contraceptives to have significantly lower testosterone
cortisol and progesterone to be correlated in men and women taking
compared to normally-cycling women. It is worth noting, though, that
oral contraceptives following an emotionally arousing manipulation
oral contraceptive use did not account for any significant differences
. One would expect cortisol and progesterone to be correlated
in levels of cortisol or progesterone. Given that oral contraceptives
among men, since the principal source of both cortisol and progesterone
reduce ovarian production of endogenous progesterone, we would
is the adrenal gland, whereas in naturally cycling women, the source of
expect normally-cycling women to have higher levels of progesterone
progesterone is both adrenal and ovarian From the present study, it
than those taking oral contraceptives, which the present data shows,
is clear that more work must be done to explore the relationship
though the difference was not statistically significant. The lack of a
between salivary progesterone and cortisol levels in both men and
statistically significant difference is most likely due to the between-
women. Testosterone and progesterone were found to be significantly
subjects design. A within-subjects design with repeated sampling
positively correlated at both time points for men, but only at Time 2 in
throughout the menstrual cycle is better suited to detect progesterone
women. Given progesterone's large fluctuations during the menstrual
increases during the luteal phase of the menstrual cycle (i.e. 22 to
cycle, one would expect the relationship between testosterone and
26 days after cycle onset) among normally-cycling women, an effect
progesterone to be more stable among men. This hypothesis is
that would be absent among women taking oral contraceptives.
supported by the present results.
Schultheiss et al. also found that testosterone levels did not
The dynamic relationship between hormones is one area in which
significantly differ across the menstrual cycle for both normally-cycling
more research is needed. For instance, with hormones being
women and women using oral contraceptives, and that normally-
significantly correlated at one time point but not the other (e.g.
cycling women experienced a significant increase in progesterone
testosterone–cortisol in men), the present results suggest that there is
during the luteal phase. The present study did not find a significant
a relationship between testosterone, progesterone, and cortisol, but
change in testosterone due to menstrual cycle phase, in accordance with
that these relationships are not as clear-cut as simple positive or
previous research . Also consistent with previous research, cortisol
negative correlations. As more research begins to incorporate the
levels were also found to be unaffected by phase of menstrual cycle (e.g.
study of multiple hormones into their designs (e.g. more
). The previously observed and well-established increase in
research into the dynamic relationships among steroid hormones
progesterone during the luteal phase was also found in the present data.
could provide valuable information for future researchers.
The expected quadratic relationship between menstrual cycle phase and
It bears mentioning that there is some disagreement in the literature
progesterone was observed at Time 1, but not at Time 2. We did not ask
regarding the validity and reliability of immunoassays for hormone
participants to provide information regarding the onset of their last
assessment Specifically, some researchers have called into question
menstrual cycle at Time 2; instead that information had to be
the validity of enzyme immunoassays which is why we chose to use
extrapolated from the information provided at Time 1. This process
radioimmunoassays to measure salivary hormone levels. The radioim-
yielded menstrual cycle phase estimates that are less precise at Time 2
munoassay procedure has been employed to measure a variety of
than at Time 1. A visual inspection of the data (see suggests that
steroid hormones in saliva (cortisol — testosterone — cortisol,
there was a midcycle increase in progesterone at Time 2, but that
testosterone, and progesterone — and has been found to be both a
statistical noise attributable to this extrapolation process is most likely
valid procedure for measuring salivary hormones and a more accurate
obscuring this effect. Again, we emphasize that day of menstrual cycle
measure than enzyme immunoassays .
and menstrual cycle phase at both time points are estimations derived
Some researchers have argued against essential usefulness of
from self-reported menstrual cycle information.
saliva samples for measuring levels of endogenous steroid hormones,
Time of day was a significant factor at both time points for cortisol
claiming that salivary assays "do not meet the criteria for routine
(see exemplifying the well-established circadian cortisol
diagnostic tests and their introduction into laboratory repertoire
response (e.g. ) with elevated levels in the morning hours and a
cannot be justified at present" , p. 193). Others have argued that
steep decline throughout the morning and into the afternoon. Time of
"saliva…has proven to be reliable and, in some cases, even superior to
day was also a significant factor for progesterone at Time 2, but not Time
other bodily fluids" , p. 1759) for measuring hormone levels. The
1. Time of day was not a significant factor for testosterone at either time
validity and reliability of salivary hormone assessments should be
point. The absence of this pattern in testosterone is surprising given
scrutinized, and the best way to address this disagreement is through
previous research that has shown circadian rhythms among androgens
continued research. The present study provides further support for
. The lack of this effect in testosterone at both time points and Time 1
the continued use of saliva as a noninvasive means for measuring
progesterone is most likely due to the between-subjects design of the
endogenous steroid hormones. While it is true that steroids can
present study. As with menstrual cycle effects, a within-subjects design
undergo "rapid fluctuations in salivary concentrations" (p. 186),
would be preferable for testing changes in endogenous hormone levels
the present study shows that basal steroid levels, in fact, remain
as a function of time of day. The fact that the cortisol response was still
relatively static over a two-week period.
detectable at both time points between-subjects speaks to therobustness of its circadian pattern.
Finally, the present study also examined the correlations between
each of the three hormones (see Testosterone and cortisol were
Parts of this research were supported by a National Science
uncorrelated at both time points in women. In men, testosterone was
Foundation grant (BCS-0444301).
significantly positively correlated with cortisol at Time 1, but uncorre-lated at Time 2. While previous work has suggested an antagonisticrelationship between testosterone and cortisol , that relationship is
driven in large part by the antagonism between the HPA and HPG axes.
[1] Brambilla DJ, Matsumoto AM, Araujo AB, McKinlay JB. The effect of diurnal
The present study did not involve activating either axis, thus one would
variation on clinical measurement of serum testosterone and other sex hormone
not necessarily expect negative correlations between testosterone and
levels in men. J Clin Endocrinol Metab 2009;94(3):907–13.
[2] Brown SL, Fredrickson BL, Wirth MM, Poulin MJ, Meier EA, Heaphy ED, et al. Social
cortisol. In fact, previous research has found basal testosterone and basal
closeness increases salivary progesterone in humans. Horm Behav 2009;56
cortisol to be moderately, positively correlated in both sexes (e.g.
), though this relationship was found only among men in
[3] Celec P, Ostatnikova D, Skoknova M, Hodosy J, Putz Z, Kudela M. Salivary sex
hormones during the menstrual cycle. Endocr J 2009;56(3):521–3.
the present data. Cortisol and progesterone were significantly positively
[4] Dabbs JM. Salivary testosterone measurements: reliability across hours, days, and
correlated among men only at Time 1 and among women only at Time 2.
weeks. Physiol Behav 1990;48:83–6.
S.H. Liening et al. / Physiology & Behavior 99 (2010) 8–16
[5] Dabbs JM, de La Rue D. Salivary testosterone measurements among women:
[25] Schultheiss OC, Dargel A, Rohde W. Implicit motives and gonadal steroid hormones:
relative magnitude of circardian and menstrual cycles. Horm Res 1991;35:182–4.
effects of menstrual cycle phase, oral contraceptive use, and relationship status.
[6] Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: a theoretical
Horm Behav 2003;43:293–301.
integration and synthesis of laboratory research. Psychol Bull 2004;130(3):355–91.
[26] Schultheiss OC, Liening S, Schad D. The reliability of a Picture Story Exercise
[7] Edwards S, Clow A, Evans P, Hucklebridge F. Exploration of the awakening cortisol
measure of implicit motives: estimates of internal consistency, retest reliability,
response in relation to diurnal cortisol secretory activity. Life Sci 2001;68:2093–103.
and ipsative stability. J Res Pers 2008;42:1560–71.
[8] Edwards DA, O'Neal JL. Oral contraceptives decrease saliva testosterone but do not
[27] Schultheiss OC, Stanton SJ. Assessment of salivary hormones. In: Harmon-Jones E,
affect the rise in testosterone associated with athletic competition. Horm Behav
Beer J, editors. Methods in social neuroscience. New York: Guilford; 2009. p. 17–44.
[28] Schultheiss OC, Wirth MM, Stanton SJ. Effects of affiliation and power motivation
[9] Eide P, Kemp A, Silberstein RB, Nathan PJ, Stough C. Test–Retest reliability of the
arousal on salivary progesterone and testosterone. Horm Behav 2004;46:592–9.
emotional Stroop task: examining the paradox of measurement change. J Psychol
[29] Sellers JG, Mehl M, Josephs RA. Hormones and personality: testosterone as a
marker of individual differences. J Res Pers 2007;41:126–38.
[10] Fehring RJ, Scheider M, Raviele K. Variability in the phases of the menstrual cycle.
[30] Silbergeld S, Brast N, Noble EP. The menstrual cycle: a double-blind study of
J Obstet Gynecol Neonatal Nurs 2006;35(3):376–84.
symptoms, mood and behavior, and biochemical variables using envoid and
[11] Gosling SD, Rentfrow PJ, Swann WB. A very brief measure of the Big-Five
placebo. Psychosom Med 1971;33(5):411–28.
personality domains. J Res Pers 2003;37:504–28.
[31] Soto CJ, John OP, Gosling SD, Potter J. The developmental psychometrics of Big Five
[12] Gray A, Jackson D, McKinlay J. The relation between dominance, anger, and
self-reports: acquiescence, factor structure, coherence, and differentiation from
hormones in normally aging men: results from the Massachusetts Male Aging
ages 10 to 20. J Pers Soc Psychol 2008;94(4):718–37.
Study. Psychosom Med 1991;53:375–85.
[32] Stanton SJ, Schultheiss OC. Basal and dynamic relationships between implicit
[13] Groschl M. Current status of salivary hormone analysis. Clin Chem 2008;54
power motivation and estradiol in women. Horm Behav 2007;52(5):571–80.
[33] van Anders SM, Watson NV. Menstrual cycle irregularities are associated with
[14] Groschl M, Rauh M, Dőrr HG. Circadian rhythm of salivary cortisol, 17α-
testosterone levels in healthy premenopausal women. Am J Hum Biol 2006;18:841–4.
hydroxyprogesterone, and progesterone in healthy children. Clin Chem 2003;49
[34] Viau V. Functional cross-talk between the hypothalamic–pituitary–gonadal and –
adrenal axes. J Neuroendocrinol 2002;14:506–13.
[15] Groschl M, Rauh M, Schmid P, Dőrr HG. Relationship between salivary
[35] Viau V, Soriano L, Dallman MF. Androgens alter corticotropin releasing hormone
progesterone, 17-hydroprogesterone, and cortisol levels throughout the normal
and arginine vasopressin mRNA within forebrain sites known to regulate activity
menstrual cycle of healthy postmenarcheal girls. Fertil Steril 2001;76(3):615–7.
in the hypothalamic–pituitary–adrenal axis. J Neuroendocrinol 2001;13:442–52.
[16] Groschl M, Wagner R, Rauh M, Dorr HG. Stability of salivary steroids: the influence
[36] Vicennati V, Ceroni L, Genghini S, Patton L, Pagotto U, Pasquali R. Sex difference in
of storage, food, and dental care. Steroids 2001;66:737–41.
the relationship between the hypothalamic–pituitary–adrenal axis and sex
[17] Hansen AM, Garde AH, Persson R. Sources of biological and methodological
hormones in obesity. Obesity 2006;14:235–43.
variation in salivary cortisol and their impact on measurement among healthy
[37] Wirth MM, Meier EA, Fredrickson BL, Schultheiss OC. Relationship between
adults: a review. Scand J Clin Lab Invest 2008;68(6):448–58.
salivary cortisol and progesterone levels in humans. Biol Psychol 2007;74:104–7.
[18] Herold DA, Fitzgerald RL. Immunoassays for testosterone in women: better than a
[38] Wirth MM, Schultheiss OC. Basal testosterone moderates responses to anger faces
guess? Clin Chem 2003;49(8):2003.
in humans. Physiol Behav 2007;90:496–505.
[19] Kirschbaum C, Steyer R, Eid M, Patalla U, Schwenkmezger P, Hellhammer D.
[39] Wood P. Salivary steroid assays — research or routine? Ann Clin Biochem
Cortisol and behavior: 2. Application of a latent state-trait model to salivary
[40] Wüst S, Wolf J, Hellhammer DH, Federenko I, Schommer N, Kirschbaum C. The
[20] Kirschbaum C, Kudielka BM, Gaab J, Schommer NC, Hellhammer DH. Impact of
cortisol awakening response — normal values and confounds. Noise Health
gender, menstrual cycle phase, and oral contraceptives on the activity of the
hypothalamic–pituitary–adrenal axis. Psychosom Med 1999;61:154–62.
[41] Oskis A, Loveday C, Hucklebridge F, Thorn L, Clow A. Diurnal patterns of salivary
[21] Lemay S, Bédard MA, Rouleau I, Tremblay PLG. Practice effect and test–retest
cortisol across the adolescent period in healthy females. Psychoneuroendocrinol-
reliability of attentional and executive tests in middle-aged to elderly subjects.
Clin Neuropsychol 2004;18(2):284–302.
[42] Dabbs JM. Salivary Testosterone Measurements: Collecting, Storing, and Mailing
[22] Mehta PH, Jones AC, Josephs RA. The social endocrinology of dominance: basal
Saliva Samples. Physiol Behav 1991;49:815–7.
testosterone predicts cortisol changes and behavior following victory and defeat.
[43] Raff H, Homar PJ, Burns EA. Comparison of Two Methods for Measuring Salivary
J Pers Soc Psychol 2008;94:1078–93.
Cortisol. Clin Chem 2002;48(1):207–8.
[23] Popma A, Vermeiren R, Geluk CAML, Rinne T, van den Brink W, Knol DL, et al.
[44] Campbell KL, Schultheiss OC. A Necessary adjustment of protocol for use of DPC
Cortisol moderates the relationship between testosterone and aggression in
coat-a-count total testosterone assay with saliva. Clin Biochem 1999;32(1):83–5.
delinquent male adolescents. Biol Psychiatry 2007;61:405–11.
[24] Pruessner JC, Wolf OT, Hellhammer DH, Buske-Kirschbaum A, von Auer K, Jobst S,
et al. Free cortisol levels after awakening: a reliable biological marker for theassessment of adrenocortical activity. Life Sci 1997;61(26):2539–49.
Source: http://www.scottliening.com/research/publications/Lieningetal_2010.pdf
Actividad docente y riesgo de estrés. Acerca de la relación entre el trabajo en escuelas de los niveles educativos obligatorios y su impacto sobre la salud física y psicológica de los docentes. Olga Cristina Colatarci. El presente trabajo se propone analizar como afecta a los docentes, a cargo de un grupo de alumnos, realizar la totalidad de la tarea que su rol implica. ¿Cuáles son los límites o
The Open Clinical Chemistry Journal, 2009, 2, 7-11 7 Open Access Improvement of Phencyclidine-Induced Cognitive Deficits in Mice by Subsequent Subchronic Administration of Fluvoxamine, but not Sertraline Tamaki Ishima1, Yuko Fujita1, Mami Kohno1, Shinsui Kunitachi1, Mao Horio1, Yuto Takatsu1, Takahiko Minase1, Yuko Tanibuchi1,2, Hiroko Hagiwara1,2, Masaomi Iyo2 and Kenji Hashimoto1,*