Kamagra gibt es auch als Kautabletten, die sich schneller auflösen als normale Pillen. Manche Patienten empfinden das als angenehmer. Wer sich informieren will, findet Hinweise unter kamagra kautabletten.
Head lice: evidence-based guidelines based on the stafford report

HEAD LICE: EVIDENCE-BASED
GUIDELINES BASED ON THE
STAFFORD REPORT
2012 UPDATE
Produced by
Public Health Medicine Environmental
Background and Acknowledgements
1.1. The Original 1998 Stafford Report , 2002 and 2012 Updates
There is a need for a consistent, integrated, rational approach to the prevention and control of head louse infection in the UK. Myths and misinformation abound and there has been insufficient high quality scientific research for the production of authoritative, evidence-based policies. The national professional organisation for Consultants in Communicable Disease Control (CCDC) in Great Britain and Ireland is the Public Health Medicine Environmental Group (PHMEG). In 1997 the PHMEG commissioned three members to produce guidance on head louse control. These members reviewed the available evidence, discussed the issues with a multiprofessional working group and consulted widely amongst colleagues around the country to gain as balanced a view as possible on what might constitute a rational base for a national approach to the problem. Supported by the Deputy Director of the Cambridge Medical Entomology Centre, the three members produced a document that became known as the "Stafford Report" 1, since the authors met in Stafford. Referencing was deliberately omitted, since it was intended to be a "best practice" guidance document and there was insufficient evidence of high quality to produce a comprehensive authoritative scientific statement. The Stafford Report was distributed for wide consultation and in its final version was formally accepted by the PHMEG in June 1998. Since then, modified according to local needs, it has been widely adopted and has been found to be a rational and logical approach for devising local policies and providing useful informational materials for professionals and public alike. This was complemented by a video produced by PHMEG. The 1998 Stafford Report1 was written by the "Stafford Group": Dr Robert Aston CCDC, Bolton Health Authority Dr Harsh Duggal, CCDC, South Staffordshire Health Authority Dr John Simpson, CCDC, West Surrey Health Authority Advised by:
Ian Burgess, Deputy Director, Medical Entomology Centre Cambridge
While a consensus document such as the Stafford Report is valuable, it is useful to identify
which statements are supported by research and which rely on consensus. This enables
readers to identify those areas of care where there is perhaps more clinical freedom. In
addition, this approach explicitly identifies the strength of evidence behind each
recommendation. Therefore, in 2002 the Centre for Evidence-Based Medicine at the University
of Oxford was asked to review the Stafford Report, with an updated Stafford Report published in
the Journal of Family Health Care 2. The evidence-based assessment in the 2002 update of the
report was provided by Martin Dawes at the Oxford Centre for Evidence-Based Medicine.
Evidence for statements was sought and appraised. Grades of recommendation (A to D, where
A is the strongest recommendation) were allocated to each of the main claims within the
Report, giving an indication of the strength of the evidence supporting each one. These were
given in bold within parentheses alongside the appropriate statement. Key references were
also added.
1.2. The 2008 Evidence Based Update
This further update of the report builds on the 2002 version, and includes more recent evidence
and recommendations in relation to chemical treatments, including the availability of new
products and evidence around non-chemical alternative approaches. Much of the information
and guidance provided in both the original 1998 Stafford Report, and the 2002 update, still
stands and has not been altered.
The 2008 Update was produced by a working group:
Dr Alison Teale
Public Health Specialist Trainee, West Midlands Deanery
Director, West Midlands North Health Protection Unit
Dr Wendy Phillips
Director, South Yorkshire Health Protection Unit
Mrs Mandy Beaumont Health Protection Nurse, West Midlands North Health Protection Unit Mrs Audrey Pepperman Health Protection Nurse Specialist, Cambridgeshire and Peterborough
Health Protection Unit
Communicable Disease Control Nurse, Leeds Primary Care Trust
Ian Burgess, Director, Medical Entomology Centre, Cambridge
With thanks to:
Mrs Veronica Baker
Mrs Wendy Jeffcott
Mrs Vicki Tilston
The 2012 Update was the result of a review prior to reloading on the PHMEG website
undertaken by Martin Schweiger with thanks to Sally Millership for her contribution. The
principal changes in the 2012 update were the removal of information on carbaryl based
products because they are no longer available in England, the updating of relevant web links
and a reference to the change in legislation relating to the exclusion of children from school.
This report is produced for members of the Public Health Medicine Environmental Group
and is available on its website: www.phmeg.org.uk
1.3. Using this Update
As with previous versions, this report should be read in conjunction with the Appendices, which contain notes and guidance for involved professional groups and suggest key messages for public information. The latter are written in everyday non-technical language so as to be readily developed for distribution to the public, but should also be of value for training professional groups and for the development of protocols for them. In addition, Appendix 1 consists of a glossary and recommendations concerning terminology. There has been limited research into the epidemiology of head louse infection on which to base our understanding of many aspects of the management of this problem. This Report is based on the best available evidence. The term "infection" is used throughout these documents in order to be consistent with the view that the term "infestation" has pejorative, stigmatic overtones and should be avoided in public information leaflets. The Report is lengthy because it is intended to be an explanatory document and to serve as the basis for the development of local policies and protocols. Because readers may selectively read only the sections applicable specifically to themselves, there has inevitably had to be some repetition in the document as a whole. Recommendations have not been separated from the main text since the authors believe it is important that readers understand the reasoning behind them.
1.4. Assessment of the strength of evidence
Evidence for this and the 2002 Update of the Stafford Report 2 has been classified according to
the robustness and quality of the sources available. Evidence statements are categorised as
grade A to D, where A is the strongest recommendation. Further information about the
assessment of evidence is provided in Appendix 9.
Levels of evidence and grades of recommendation
Grade of
Type of study
Systematic review of randomised control trials
Individual good-quality randomised control trial
Systematic review of cohort studies
Individual cohort study or low-quality randomised control trial (e.g. <80% follow-up)
"Outcomes" research; ecological studies
Systematic review of case-control studies
Individual case-control study
Case series (and poor-quality cohort and case-control studies)
Expert opinion without explicit critical appraisal, or based on physiology, bench research or "first principles"
General points
1.5. Prevalence and risk factors
Although head louse infection is an infectious disease, many of the problems associated with it
are due to society's reaction to the infection rather than the organism itself. There is limited
research matter on true prevalence of infection, but is probably much lower than the public and
professional perception.
There is evidence that head lice are increasing in prevalence3 (B). Prevalence estimates
vary between countries and reflect, at least in part, differences in how estimates are derived. In
Israel, it is estimated that in the past 25 years, 15% to 20% of all 4-13 year old children were
infected with headlice annually 4. An Australian study found the prevalence to be much higher at
21% 5.
Information on which to base UK estimates is limited, with recent data coming from two Welsh
studies. In one therapeutic trial 4,037 children were screened and a prevalence of 4.1% was
found 6. In a study of resistance patterns in Welsh schools, 2793 primary school children were
screened for headlice and the prevalence found to be 8.3% 7.
Observational studies suggest that infections occur most often in school-aged children, although there is no evidence of a link with school attendance 8 9. Head lice are commoner in girls than boys 5 3. The peak age for infestation is 7-8 years 3. A cross-sectional study in Belgium found that head lice were significantly more common in families of low socio-economic status, in children with more siblings, and in children with long hair 10 A recent review found no evidence to support the theory that head lice prefer clean hair to dirty hair. 8
1.6. Health implications
Head lice are not a serious health problem in this country. They rarely cause physical
symptoms other than itching of the scalp (B) 11. Sensitisation reactions to louse saliva and
faeces may result in localised irritation and erythema. Skin may become infected as a result of
scratching. Lice have been identified as primary mechanical vectors of scalp pyoderma caused
by streptococci and staphylococci usually found on the skin 12.
Adverse health effects mainly derive not from lice themselves, but from the human perception of
them. Excessive public and professional reactions lead to an inflated perception of prevalence,
to unnecessary, inappropriate or ineffective action, and to a great deal of unwarranted anxiety
and distress. These actions and reactions in themselves cause problems, especially from the
misuse and overuse of treatments.
1.7. A problem of society
Head louse infection is more a societal than an infectious disease problem.
1.8. Responsibility for the control of head lice
1.8.1. Parents
The primary responsibility for the identification, treatment and prevention of head lice in a family has to lie with the parents, if only for reasons of practicality. Parents, however, cannot be expected to diagnose current infection, or to distinguish it from successfully treated previous infection or other conditions, if they are not adequately instructed and supported by the following professionals. Notes on the detection and treatment of head lice for families are given in Appendices 2, 3 and 4.
1.8.2. Primary care team
The primary professional responsibility for the diagnosis, management and treatment of any individual for any disease lies with the general practitioner with whom the patient is registered; they are also responsible for advice and support on disease prevention. Historically, because of a misplaced emphasis on head louse infections in schools, the former system of head inspections, and the (now discontinued) distribution of large quantities of chemical lotions from community based clinics, primary care teams did not traditionally involve themselves to any major degree. Nowadays, for primary care workers to refuse all responsibility for the management of head lice in individuals and families registered with them is as illogical as it would be to do so for measles, impetigo, threadworms or immunisation. General practitioners (or another member of the primary care staff) should, therefore, be knowledgeable and competent in the control of head lice, be able to teach parents the technique of detection combing and be prepared to advise on appropriate treatment. Treatment should never be advised unless the responsible officer is convinced by physical evidence that living lice are present. It should be noted that none of treatments currently available for headlice, require a prescription. Carbaryl-based products are no longer available in the UK as a result of anxieties over their carcinogenicity. Notes and guidance for the primary care team are provided in Appendix 5.
1.8.3. Pharmacists
Local pharmacists should inform themselves of local policies and protocols and should adhere to them. Every opportunity should be taken to give accurate information to the public. Customers should be dissuaded from the inappropriate, repeated or unnecessary use of chemical preparations. Pharmacists (or another member of their staff) should, therefore, be knowledgeable and competent in the control of head lice, be able to teach parents the technique of detection combing and be prepared to advise on appropriate treatment. Treatment should never be advised unless the responsible officer is convinced by physical evidence that living lice are present. Notes and guidance for community pharmacists are provided in Appendix 6.
1.8.4. School Health Services
School nurses (or equivalent) have responsibility for providing professional advice to staff, parents and children and for carrying out local policies, which should be agreed with the consultant in communicable disease control. They should provide clear, accurate, up-to-date information about head lice. This should be done on a regular basis and not only when parents' or teachers' concern is already raised or there is an "outbreak" in the school. It should generally be integrated with the management of other school health problems rather than dealt with as a special separate topic. School nurses should be prepared to teach detection combing to individuals, families (at their homes if appropriate) and groups of parents, children and staff as required, and give advice on treatment and prevention. They should not undertake head inspections as a routine screening procedure. Notes and guidance for school nurses are provided in Appendix 7. Advice on Headlice is included in the Guidance on Infection Control in Schools and other Child Care Settings information sheets which are published by the HPA and which were updated in December 20061.
1.8.5. Health Visitors
Every family in the UK with children under five has a named health visitor whose role is to offer support and advice through the early years from pregnancy and birth to primary school. Health Visitors work closely with GPs and cover the geographical area of the GP practice. Health
Visitors should be prepared to offer advice on the detection and treatment of headlice. The notes and guidance in Appendix 7 for School Nurses are also relevant to Health Visitors. Health Visitors should pay particular note to the following advice on chemical treatments and very young children (see section 6.5):
Preparations with an alcohol base should not be used in very young children (under 5 years of age) 13.
Chemical anti-headlice treatments should only be used in children under 6 months with medical supervision 13.
1.8.6. Head teachers
The head teacher should work with the school nurse and the health protection team to produce a local protocol and adhere to it. The "alert letters" system should be discontinued. Notes and guidance for head teachers are provided in Appendix 8. Advice on Headlice is included in the Guidance on Infection Control in Schools and other Child Care Settings information sheets which are published by the HPA and which were updated in December 2006 14.
1.8.7. The health protection team
The health protection team consists of the consultant in communicable disease control (CCDC) together with their health protection nurse and support staff colleagues. The CCDC is responsible for advising on the control of head lice in the population as a whole. Adequate guidelines and protocols should be produced for all involved professionals, including school nurses, school doctors, nursery nurses, general practitioners, health visitors, practice nurses, community paediatricians, infection control teams, pharmacists and head teachers (see Appendices). It is particularly important that school nurses and other community nurses are given adequate support by the CCDC, including regular training sessions and advice about specific problems.
Diagnosis
1.9. Only one sure way
A diagnosis of head louse infection cannot be made with certainty (no matter how many nits are present, how many reported cases there are in school, how bad the itch is or however dirty the pillows are) unless a living, moving louse is found.
Detection combing
The only reliable method of diagnosing current, active infection with head lice is by
detection combing (B). A study, published in 2008, found that detection combing was 3.84
times more effective than visual inspection for finding live lice15. The technique should be
carefully described in protocols for the public and professionals4;16. There may be other clues to
the presence of live lice, such as pillows being dirtier than usual in the morning. If detection
combing is not used as the diagnostic criterion, a misdiagnosis may be made, commonly due to
the factors listed below in the section of "Imaginary lice".
Many combs sold as louse detection and removal combs are unsuitable for the purpose. Only
those with flat-faced, parallel-sided teeth less than 0.3mm apart are appropriate 17. Amongst the
best known of these are the combs included in the "BugBuster" pack, which are designed for
wet-combing with conditioner.
Appendix 2 provides advice on how to perform detection combing.
Self diagnosis
Detection combing should be done by parents or family members following advice from leaflets and support from the school nurse, general practitioner, etc. Professionals should not necessarily rely on such diagnoses without asking to see the evidence, for example, a louse stuck on paper with clear adhesive tape.
Imaginary lice
Many "cases" of head louse infection are not current infections but are due to the
following (D):
itching scalp due to other causes such as eczema (which in itself may be caused by repeated treatment with chemicals)
other conditions such as seborrhoea, "dandruff" and hair muffs
extinct/treated infection but with nits still being found
extinct/treated infection but with itch persisting
parents of school children having a grievance that is not primarily to do with head lice
psychogenic itch and revulsion on hearing of other cases in the school, usually via the head teacher's "alert letter and resultant "louse phobia"
When talks are arranged in schools there is often a low turnout of parents and typically the "outbreak" is greatly reduced at least for a time thereafter. What has actually been reduced is the outbreak of public concern, not of head lice, usually because there was in fact no true outbreak of infection.
PREVENTION
Information, advice and general approach
1.13.1. Campaigns
The word "campaign" suggests intense activity to combat a major problem of the moment.
Since for head lice there is more likely to be the situation of fairly steady background
prevalence, "campaigns" might in fact fuel the fires of public concern and misapprehension (D).
It might be more sensible to concentrate efforts on providing a regular supply of reliable
information about the control of head lice, integrated with other health information. If, however,
a specific educational programme is felt to be necessary, it should:
be regular rather than driven by public alarm
provide accurate information, advice and support
strongly discourage multiple applications of chemical treatment; individual assessment of "problem cases" and "repeated reinfections" should be made
avoid the trap of "being seen to do something"
1.13.2. Leaflets and public information sources
The Department of Health has an online version of the leaflet "The prevention and treatment of
head lice" 18 which provides brief advice on headlice infection, detection and treatment. Copies
can be downloaded from the Department of Health website:
There is currently no nationally available leaflet that fully reflects the opinions and advice given
in this Report. It would be helpful if national leaflets and information based on the
recommendations contained in this Report were made available and updated regularly. Locally
produced leaflets based on this Report may be the best option for the time being and can
offer a useful resource for schools and parents (D).
There are many online sources of information about head lice that may be helpful.
In particular the information contained on the NHS Choices web site is a useful resource for
schools and parents.
Advice on Headlice is included in the Guidance on Infection Control in Schools and other Child
Care Settings information sheets which are published by the HPA and which were updated in
December 2006.
http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/SchoolsGuidanceOnInfectionControl/
Prevention methods
1.14.1. Grooming
Good hair care would seem to be sensible in terms of personal and social education and
hygiene, and grooming should be encouraged (D). Thorough, regular grooming using a
fine-toothed pocket comb has often been recommended as a means of preventing, reducing the
prevalence of, and even treating head lice, but there is little evidence supporting the efficacy of
this practice, although there has in fact been little reliable scientific assessment made. Caution
must, therefore, be exercised if claims are to be made that it is an effective method of
preventing or treating head louse infection.
1.14.2. Repellents
Proprietary products that are claimed to repel lice are not recommended. Even if they were effective in protecting the individual from infection, they do not deal with the control of lice in the population and do not treat existing infections.
CHEMICAL TREATMENT
Effectiveness of chemical treatments
Chemical treatment has been shown to be effective by a number of recent reviews (A) 19
20. A summary of recent clinical effectiveness information for the main chemical agents is provided in Appendix 11. Chemical treatment should be used when current infection is definite, since this is the only method that has been scientifically demonstrated to be effective.
Cardinal rule before chemical treatment
Chemical preparations for head louse infection should never be recommended or used unless a living, moving louse has been found on the head of at least one household member. Ideally, if one member of the household has a current infection, detection combing of all members should be undertaken, and only those found to be infected should be treated.
Chemical treatment options
Research into treatments worldwide is limited and of variable quality, the evidence presented here is from published literature in peer reviewed journals. Two main groups of chemicals (pyrethroids, and malathion) remain available and are effective 6
21 22 23 19 24 even though there is some degree of resistance to each group reported around the country that may require a change in therapy after an initial confirmed failure of treatment. The effectiveness of these chemicals probably compares favourably with that of, for example, broad-spectrum antibiotics commonly used for other infections. More recently, products based on Dimeticone have become available. Dimeticone creates a physical barrier around the louse that eventually kills it, but does not act on the insect nervous system and is thus unlikely to be affected by resistance to other chemicals25. A recent Randomised Controlled Trial 26 comparing 4% Dimeticone with 0.5% Malathion concluded that, although malathion is still effective in some people, dimeticone lotion offers a significantly more effective treatment for most people. In general, a course of treatment for head lice should always be 2 applications of product at least 7 days apart to prevent lice emerging from any eggs that survive the first application.
Currently available preparations
The table overleaf lists the preparations available in the UK based on the British National
Formulary 54 (September 07)27. All the products listed are available without prescription. All the
products listed can be prescribed. GPs are advised to seek evidence of true infection before
prescription. In addition to the products listed in the table, there are a number of products on the
market not listed in the BNF and there is currently no evidence base to support their use.
It should be noted that some formulations, in particular shampoos and crème rinses,
either contain an insufficient concentration of the active ingredient or provide too short a
contact time to be effective, and are not recommended. These include Lyclear Crème
Rinse, Prioderm Cream shampoo, Quellada Crème shampoo and Full Marks mousse.
Licensed Medical Products
Comments
Dimeticone
Lotion, dimeticone 4%
Malathion
Derbac-M®
Liquid, malathion 0.5% in an aqueous base
Lotion, malathion 0.5%, in an alcoholic base
(Also available is Cream shampoo containing 1% Malathion which is not recommended as product too diluted in use and insufficient contact time)
Liquid, malathion 0.5% in an aqueous base (Also available is Cream Shampoo - 1% Malathion which is not recommended as product is too diluted in use and insufficient contact time)
Phenothrin
Liquid, phenothrin 0.5% in an aqueous basis Lotion, phenothrin 0.2% in basis containing isopropyl alcohol (Also available is Mousse containing phenothrin 0.5% in an alcoholic basis which is not recommended for headlice due to insufficient contact time)
Permethrin is active against head lice but the formulation and licensed methods of application of the current UK products make them unsuitable for the treatment of headlice27
Safety of chemical treatment and contraindications
1.19.1. Adverse events
The main chemical agents currently used have a good track record for safety over many
years (D). Information on suspected adverse reactions are reported by clinicians, and since
2005, members of the public, to the Medicines and Healthcare Products Regulatory Agency
which is responsible for ensuring that medicine and medical devices work, and are safe.
Adverse drug reaction data can be downloaded from their website There is anecdotal evidence that mild adverse effects are under reported.
The table shows that the number of adverse drug reactions reported for anti-headlice chemicals
is very small given the high volume of their usage. In all the agents, skin reactions make up a
sizeable proportion of the reported reactions.
Earliest
Total adverse
Total adverse
reported
skin reactions
adverse event
reported
No adverse reactions for products containing Dimeticone have yet been reported to Medicines and Healthcare Products Regulatory Agency. Some of the published evidence of effectiveness includes information on adverse events indicating that the incidence of adverse reactions under trial conditions is very low. One study
comparing 0.5% phenothrin (aqueous liquid) with 4% dimeticone found that 9% of subjects treated with phenothrin experienced scalp irritation compared to 3% of those treated with dimeticone 25. Several studies which used malathion as one of the treatment options reported no adverse events amongst those treated with malathion 19. One randomised control trial comparing malathion with permethrin reported no adverse events associated with permethrin and a single case of scalp irritation amongst the 41 individuals treated with malathion which is likely to have been due to the terpenoid vehicle used 28.
1.19.2. Contraindications
Chemical anti-headlice treatments should only be used in children under 6 months with medical supervision 13. Preparations with an alcohol base should not be used in very young children (under 5 years of age) 13. Preparations with an alcohol base are contraindicated for people with scalp dermatitis or asthma. Care must, however, be taken that they are used in well-ventilated spaces, preferably in the open air, well away from sources of flame and heat such as fires, stoves, cigarettes and hair driers. Care should also be taken to prevent lotion from running over the face and into the eyes. Pyrethroid based preparations (permethrin and phenothrin) are contra-indicated in persons with an allergy to chrysanthemum flowers, as these flowers contain a natural pyrethroid 13.
"Reinfection" or "treatment failure"
Although true resistance does occur, other causes of apparent "resistance" may be more
likely to be due to ovicidal failure, misdiagnosis, faulty treatment technique or possibly
failure to eradicate imaginary lice (D). The often arduous process of determining whether
there was a true active infection and whether "treatment failure" was due to misdiagnosis or
inappropriate/inadequate treatment is, therefore, necessary.
Many cases of "reinfection" are due to one of the fol owing:
inadequate or inappropriate treatment
misdiagnosis, for example itch or nits still present after successful eradication of living lice
the finding of young lice that have not been killed whilst in the egg after the first and before the second application of lotion.
True reinfection is usually from a close contact in the community rather than specifically from a school contact. Where some carriers of lice are likely not to be aware that they are infected, others may have struggled for some time despite treatment.
Cardinal rule after chemical treatment
Inappropriate use of chemical treatments can lead to a failure to bring a headlice infection to an end, and may increase the risk of resistant lice. In general the following points should be borne in mind to avoid inappropriate use, particularly when considering a possible treatment failure. Chemical preparations should not be used for more than one complete treatment (i.e. two applications, seven days apart) unless a careful assessment has been made, including:
Was there in fact a true infection before application?
Is there in fact a current active infection now?
Are the detected lice simply those that have hatched after a first application? This is more likely to be the case if the lice found following the suspected treatment failure are predominant young or baby lice
Did the first treatment (two applications) fail?
If it did, why? (Enough lotion? Properly applied? All infected contacts treated? etc)
Is it more probable that the first infection was cleared, but reinfection has occurred? This is more likely to be the case if the lice found following the suspected treatment failure are predominantly adult.
Management of true reinfections/treatment failure
If it is certain that chemical treatment has failed for an individual or a particular family, then the following actions should be considered:
retreatment with the same preparation but ensuring that it is undertaken adequately and for all contacts simultaneously
retreatment using a different preparation
supervision and assistance, such as a domiciliary visit to the family by the school nurse or practice nurse
further thorough attempts to define if there may be a source of recurring infection, for example, a "best friend", and attempts to reduce the likelihood of reinfection of the case/family
if the problem remains, consider teaching the process of continued physical removal of lice
Resistance to chemical agents
Over the years different chemical agents have been used in the UK to tackle headlice. There is now strong evidence that the headlice population continues to develop resistance to the point where some chemicals have become obsolete 29. Resistance to a number of chemical agents, particularly permethrin, has been reported in the UK30 7. Resistance patterns vary between countries and between regions within a country. Ideally the choice of treatment will depend on local resistance patterns, but usually information about resistance is unavailable. Rotation of chemical agents in some areas was standard practice for many years as a means to reducing the impact of resistance to chemical agents. There are, however, several objections to this. It was a reasonable hope in the former days of distribution of lotions from health authority clinics that limitation to one preparation could be achieved. This is no longer the case, and under present health service arrangements a mosaic of treatments is inevitable. There are doubts about the scientific grounds underlying the concept of attempting to limit treatment to one chemical agent for a period of three years. If it is agreed that chemical treatments are inappropriately and grossly overused, with inadequate application, then it could be argued (from parallels with antibiotic therapy such as their use against tuberculosis in the Third World) that the limitation of therapy to one agent is more likely to encourage the proliferation of resistant lice than would a mosaic system. It is impossible to limit the distribution of headlice treatments because they are available over the counter. effectively.
Unnecessary and excessive use will occur, such as those parents who apply chemical treatments regularly to their children's heads "just in case". The policy of rotating chemical agents on a district-wide basis is now considered outmoded 27. To overcome the development of resistance, a mosaic strategy is required whereby, if a course of treatment fails to cure, a different insecticide is used for the next course.
ALTERNATIVE APPROACHES TO TREATMENT
General points
Parental concerns over use of chemical preparations to treat headlice are common and a number of products based on alternative approaches are currently on the market. In addition, chemical preparations are most often purchased without a prescription and the cost of repeatedly purchasing such items may be prohibitive, particularly for low income families. Parents may be drawn to less costly approaches for financial reasons, perhaps being unaware that their GP can prescribe headlice treatments. Unfortunately many of the alternative products available lack an evidence base on which to assess effectiveness. In addition, the safety of some alternative methods is unknown and there is, therefore, the risk that safety problems could arise.
Mechanical removal of headlice ("Bug Busting")
1.25.1. Evidence of effectiveness
In recent years, mechanical removal of lice by wet combing with the use of conditioner has been
put forward as a method of treatment and control, often termed "bug-busting". "Bug Buster" kits
are available to buy and contain special narrow-toothed combs, to be used with conditioner and
instructions on appropriate use. There is some evidence that, if performed rigorously and
according to the instructions provided with Bug Busting kits, wet combing can be effective in a
proportion of cases, but the level of effectiveness is generally much lower than that seen with
chemical preparations 6 although one study reported that the Bug Busting kit could achieve a
cure rate as high as 57% 31. However, a number of methodological issues have been raised in
relation to this study which may have biased the results in favour of BugBusting 32. Thus
mechanical removal of lice is less effective at treating infection than chemical treatment
(A). Nonetheless, wet combing may be a preferred option for some parents, and where this is
the case it is essential that the technique is carried out appropriately. Wet combing is an option
for diagnosing current infection.
For mechanical removal of lice to be a helpful element in controlling headlice, it needs to be
carried out thoroughly, at appropriate intervals and include all relevant family members. Wet-
combing of hair is often time-consuming and children may find it uncomfortable particularly if
they have long or curly hair. It is likely that the degree to which mechanical removal is carried
out to a sufficient standard varies enormously, and for this reason it cannot be relied upon as a
means of controlling lice at a community level.
1.25.2. BugBusting as a treatment option
There are some circumstances in which BugBusting may be an appropriate option for families. When a health adviser is quite sure that appropriate and thorough conventional treatment of a definitely diagnosed case of active current infection has failed, mechanical removal might be tried for individual cases and their families. It may also be considered when patients refuse to accept conventional treatment with chemical treatments because of concern about their safety. Appendix 2 provides more information on how to perform wet combing.
1.25.3. Other means of mechanical removal
A number of devices are available which claim to electronically aid the removal and/or killing of
lice including electronic combs and dry air devices. Evidence of effectiveness of these devices
is generally absent.
In general electronic devices are expensive and their incorrect usage may present a
safety risk. The current recommendation is that these devices are not suitable for general
use (D).
Herbal and essential oils
A number of products containing essential oils such as tea tree and eucalyptus oil are marketed as "natural" remedies for headlice. There is little evidence available on which to assess the effectiveness or safety of such products. Different products contain different concentrations and combinations of essential oil and it is hard to generalise the findings from the little evidence that is available. Many formulations, particularly shampoos and mousses, contain low concentrations of active ingredients, or provide an insufficient contact time and thus even if the active agent has the potential to eradicate lice, it is unlikely to do so. One study compared eradication rates between a herbal product containing coconut, anise and ylang ylang and a product containing a combination of insecticides (permethrin and malathion, synergised with piperonyl butoxide), and found no difference between eradication rates 4. Some ingredients in herbal or essential oil-based products are usually harmless, such as dilute vinegar, whereas some may be dangerous. Essential oils such as tea tree and lavender oil can be quite toxic, especially as concentrates. One new product on the UK market is Lice AttackTM (PM consumer Products AG) is based on coconut oil; however there is as yet a lack of evidence on which to base any assessment of effectiveness.
Other medical devices and alternative cures
A number of fluid preparations are marketed as medical devices for the eradication of headlice. Products which claim to have a physical action on headlice are coming onto the UK market, including Full Marks SolutionTM , Lyclear Spray AwayTM, and Nice 'n ClearTM head lice lotion. There is as yet insufficient evidence available on which to assess the effectiveness of these new products. A recent assessment of a number of home remedies, including vinegar, isopropyl alcohol, olive oil, mayonnaise, melted butter and petroleum jelly concluded that none of the substances assessed were an effective means of eradicating headlice 33.Other "remedies" and "preventives" such as children wearing baseball caps over their heads throughout the day in school are not supported by any evidence, may be damaging and should be discouraged.
WHICH TREATMENT TO CHOOSE?
Given that a true infection is diagnosed, when advising a parent or carer on which treatment is best for their child/children, or (less commonly) advising on treatment for adult infection, there are a number of aspects which require consideration:-
(if relevant) the age of the child concerned, as treatments are not licensed for those under 6 months
any contraindications including asthma, skin conditions, allergies
previous recent use of chemical treatment
existing patterns of resistance
wish to avoid creating resistance
- individual parent/carer preference
On the basis of the currently available evidence, which is summarised in Appendix 11,
any one of the following three treatment options are recommended:
NB: With all chemical treatments for headlice it is vitally important that products are
selected to be a formulation that contains sufficient active agent, and provides a
sufficient contact time to allow the active agent to work. Section 6.4 outlines the
currently available formulations and which of those are recommended by the British
National Formulary27. In general, formulations such as mousses and shampoos are not
recommended for use. Chemical treatments must be used in accordance with the
manufacturers instructions, with particular regard to the need to administer a 2nd
application at an interval (usually 7 days) after the 1st. It is likely that many apparent
treatment failures or reinfections are really a result of a failure to use chemical
treatments properly.
1.Dimeticone
The current evidence suggests that Dimeticone is an effective agent, with lice eradication rates
in the order of 70% 25 26. The evidence to support the effectiveness of this relatively new agent
is limited and there is a need for longer-term assessment to be carried out. Nonetheless it would
appear that Dimeticone provides a promising treatment option as it's mode of action is one that
is likely to avoid the appearance of resistant lice. A recent overview published in the Drugs and
Therapeutics Bulletin17 concluded that on current evidence Dimeticone should be seen as a
useful alternative to products containing conventional insecticides (malathion and phenothrin).
2.Phenothrin
Products containing Phenothrin have been used for a number of years and it has a favourable
safety record. The available evidence shows variable levels of effectiveness 34 35 with one high
quality study reporting an eradication rate of 75% 25. Levels of lice resistant to Phenothrin may
be rising which would suggest that this agent could become less effective.
3.Malathion
Products containing Malathion have been used for a number of years and it has a favourable
safety record. The available evidence demonstrates high levels of effectiveness for this agent
with eradication rates of between 78% and 95% reported 34 28 6. However, as with Phenothrin,
there is evidence that levels of resistance to this agent are rising22. One recent UK study26
found that Malathion eradicated lice in only 33% of those treated with it.
Chemical agents not recommended for use
Although clinical effectiveness data suggest that Permethrin can be effective in treating headlice
it has been excluded from this list as none of the currently available Permethrin preparations are
recommended by the British National Formulary27 for the treatment of headlice 27.
General approach to chemical treatment
The need to avoid populations of resistant lice building up has, in the past, been reflected in
treatment advice recommending single agents and advocating a mosaic approach.
Unfortunately, mosaic treatment protocols are often complicated and may not be well adhered
to. Although it would be helpful to be able to base the choice of treatment on information about
local resistance patterns, this data is generally not available. However, the mode of action of
Dimeticone is such that it is unlikely to provoke the appearance of lice resistant to this agent.
Particularly in areas were resistance appears to be an issue Dimeticone would appear to be the
most favourable chemical treatment option.
Non-chemical approaches
Some parents may wish to avoid chemical treatments, and others may try the available
chemical treatments but find them ineffective or experience an adverse reaction. In these
instances parents may wish to use a non-chemical approach, the most well established of which
is BugBusting. There is evidence of limited effectiveness if the BugBusting regime is well
adhered to, with eradication rates of between 38% and 52% reported 6 35 31. The BugBusting
technique is labour intensive and requires a high level of commitment in the part of the parent or
carer. It is recommended that, where parents wish to use this technique, the correct equipment,
particularly the fine-tooth BugBusting combs, are used.
A SPECIAL WORD ON SCHOOLS
"It's the school's fault!"
Head lice are not primarily a problem of schools but of the community. Stigma and tradition, however, combine with inadequate public and professional knowledge to continue to hold schools responsible.
The "Nit Nurse"
Routine head inspections, usually performed by the school nurse, are without value as a screening measure and should not be done, though examination of an individual (not necessarily in school) may be indicated to establish the presence of infection in a specific population group. Before the effective control of head lice became possible with chemical lotions, severe cases of infection occurred and head inspections served to detect the very worst and, therefore, most obvious of them. Nowadays, such gross infections rarely occur. Most active infections are of only a few lice and routine head inspections are ineffectual at identifying these.
"Alert letters"
One of the principal causes of unnecessary public alarm is the "alert letter" sent out by head teachers, typically warning parents that "we have head lice in the school". This is an il ogical and unnecessary reaction: Most schools will always have some pupils with head lice at any one time. An "alert letter" could be sent out every day of the school year. It often converts the usual background level of infection in the school into a pseudo-outbreak in which the parents' perception is that the school is riddled with lice. Many parents become convinced they and their children have head lice when they in fact do not (psychogenic itch), or decide to use chemical lotions as inappropriate prophylaxis "just in case".
Exclusion from school
There is provision in the Health Protection (Local Authority Powers) Regulations 2010, SI no 2010/657 for the Local Authority to exclude children from schools and nurseries. The use of these powers requires careful consideration by all parties involved. Exclusion should not be used because: It cannot ensure the elimination of infection from the family of a child. It is an unproductive and undesirable overreaction to a problem that is not a public health threat. It is inappropriate, being in fact simply an admission of the failure to deal with infection by the community and its professional advisers, but does not contribute to a solution. It is not used for other conditions with low transmissibility such as verrucas or herpes simplex infections. Families with continuing or recurring infection with head lice should be assisted and supported, as they would be with any other infection, by the concerted support and help of the community (including the school) and health professionals (including, for example, visits by the school nurse to the family home).
AREAS FOR FURTHER RESEARCH
There has been limited support for population research, possibly because head louse infection has not been perceived by health professionals as a serious problem. There is an urgent need for proper peer-reviewed studies using standardised techniques to be undertaken. Areas for research include:
validation of the detection method
the size of the problem and the prevalence of infection
general epidemiology
intervention studies of treatments
modelling of transmission dynamics
patterns of resistance
reported adverse reactions
optimal delay between first and second treatment
APPENDIX 1: GLOSSARY AND TERMINOLOGY
Glossary
Detection comb
A special plastic comb which should have rigid teeth no further than 0.3 mm apart, each tooth
preferably having at least one flat surface. Metal combs are too harsh and may pull out hair.
Hair muffs
Rings of debris from the hair follicle that surround the hair shaft and grow out with it. They may
be mistaken for nits but, unlike nits, they can be easily slid along the hair shaft.
Head louse
An insect parasite, Pediculus capitis, which can only survive on the human scalp and has a
needle-like mouthpart with which it pierces the scalp to feed on blood.
Incidence
The proportion of people who develop new infection in a given group over a period of time,
usually one year (compare "prevalence").
Nit
The empty eggshell of the head louse left stuck to a hair shaft after the insect has hatched.
Prevalence (point prevalence)
The proportion of people with active infection in a given group at a given time (compare
"incidence").
Terminology
The following terms are recommended for use in policies and leaflets:
Head louse (singular)/head lice (plural)
The form headlouse/headlice is non-standard.
Infection
"Infestation", though correct, has unpleasant overtones and tends to reinforce social stigma.
"Infection" is generally a more helpful term when dealing with head lice.
Lotion
For simplicity, the term lotion used in this document includes all types of licensed products,
except shampoos (which are ineffective). However, commercial products for treatment of
headlice are normally described as lotion (alcohol base) and liquid (aqueous base).
APPENDIX 2: NOTES FOR FAMILIES – HAVE YOU GOT HEAD LICE?
Detection combing – how to do it
You need:
Plastic detection comb (from the pharmacist)
Good lighting
Ordinary comb
Wash the hair well and then dry it with a towel. The hair should be damp.
Make sure there is good light. Daylight is best.
Comb the hair with an ordinary comb.
Start with the teeth of the detection comb touching the skin of the scalp at the top of the head.
Keeping in contact with the scalp as long as possible, draw the comb carefully towards the edge
of the hair.
Look carefully at the teeth of the comb in good light.
Do this over and over again from the top of the head to the edge of the hair in all directions,
working round the head.
Do this for several minutes. It takes 10 to 15 minutes to do it properly for each head.
If there are head lice, you will find one or more lice on the teeth of the comb.
Head lice are little insects with moving legs. They are often not much bigger than a pin head,
but may be as big as a sesame seed (the seeds on burger buns).
Clean the comb under the tap. A nail brush helps to do this.
If you find something and aren't sure what it is, stick it on a piece of paper with clear sticky tape
and show it to your school nurse or family doctor. There can be other things in the hair that are
not lice.
Notes
You can buy a plastic detection comb from the pharmacist. Many combs sold as louse detection
and removal combs are unsuitable for the purpose. Only those with flat-faced, parallel-sided
teeth less than 0.3mm apart are appropriate 17. Amongst the best known of these are the combs
included in the "BugBuster" pack, which are designed for wet-combing with conditioner.
If you need help and advice, ask your local pharmacist, health visitor, school nurse or family
doctor.
Don't treat unless you are sure that you have found a living, moving louse.
APPENDIX 3: NOTES FOR FAMILIES – HOW TO TREAT HEAD LICE
Notes
Please read NOTES FOR FAMILIES – HAVE YOU GOT HEAD LICE?
Don't treat unless you are sure you have found a living, moving louse.
Never use head louse lotions on your family "just in case". It's never a good idea to use
chemicals if they aren't really needed.
If you are sure you have found a living louse:
Check the heads of all the people in your home.
Only treat those who have living, moving lice.
Treat them all at the same time with a headlice lotion (not shampoo).
Ask your local pharmacist, school nurse, health visitor or family doctor which lotion to use and
how long to leave it on.
Always follow manufacturers instructions when applying a lotion.
Put the lotion on to dry hair.
Use the lotion in a well-ventilated room or in the open air.
Part the hair near the top of the head, put a few drops on to the scalp and rub it in. Part the hair
a bit further down the scalp and do the same again. Do this over and over again until the whole
scalp is wet.
With long hair you don't need to apply lotion down any further than where you would put a
ponytail band (except when applying Dimeticone which should fully cover hair).
Use enough lotion – at least one small bottle for each head and more if the hair is thick. Use all
the lotion up.
Keep the lotion out of the eyes and off the face. One way is to hold a cloth over the face.
Let the lotion dry on the hair. Some lotions can catch fire, so keep well away from flames,
cigarettes, stoves and other sources of heat. Don't use a hair dryer.
Repeat the treatment in seven days' time for all of those receiving the first treatment.
Check all the heads a day or two after the second treatment. If you still find living, moving lice,
ask your local pharmacist, health visitor, school nurse or family doctor for advice.
APPENDIX 4: NOTES FOR FAMILIES – HEAD LICE: THE TRUTH AND THE MYTHS
The lice
Head lice are small insects with six legs. They are often said to be "as large as a match head";
in fact, they are often not much bigger than a pin head and rarely bigger than a sesame seed
(the seeds on burger buns).
They live on, or very close to the scalp and don't wander far down the hair shafts for very long.
The louse's mouth is like a very small needle. It sticks this into the scalp and drinks the blood.
They can only live on human beings; you can't catch them from animals.
Nits are not the same thing as lice. Lice are the insects that move around the head. Nits are
egg cases laid by lice, which are glued onto hair shafts; they are smaller than a pin head and
are pearly white.
If you have nits it doesn't always mean that you have head lice. When you have got rid of all
the lice, the nits will stay stuck to the hair until it grows out.
You only have head lice if you can find a living, moving louse (not a nit) on the scalp.
Who and where?
Anybody can get head lice, but they are much rarer in adults.
Head louse infection is a problem of the whole community, not just the schools.
Infection is common during school holidays as well as during term time. Parents start to worry
more about lice when children go back to school because they think the lice are being caught
there.
A lot of head louse infections are caught from close family and friends in the home and
community, not from the school.
It's not just children who have head lice; adults get them too.
It's often said that head lice prefer clean, short hair. In fact, they probably don't much care
whether hair is dirty or clean, short or long.
How you get them
Head lice can walk from one head to another when the heads are touching for some time.
You are very unlikely to pick up head lice from brief contact with other people. The longer you
have head-to-head contact with someone who has lice, the more likely it is you will get them
too.
They can't swim, fly, hop or jump. The idea that they can jump may have come from the fact
that, when dry hair is combed, a head louse caught on the teeth of the comb is sometimes
flicked off by static electricity (this is one reason why detection combing should be done with the
hair damp).
You don't get them from objects such as chair backs. Although it's just possible that a louse
might get from one head to another if a hat is shared, this is very unlikely. It's not the way
infection is usually caught.
What happens next
If you catch two or more lice, they may breed and increase slowly in number. At this stage,
most people don't have any symptoms and won't know they have lice unless they look very
carefully for them.
For the first two or three months, there is usually no itch, but then the scalp may start to itch
badly. This is due to an allergy, not to the louse bites themselves.
Most people only realise they have head lice when this itch starts. By then they've had lice on
their head for two or three months without knowing it.
In most infections, there aren't more than a dozen or so lice on the scalp at any one time.
Some people never get the itch, including adults. They may have a few lice on their heads for
years without knowing it and can pass them to other people.
Louse droppings may fall on to the pillow during the night. Pillows may then get dirty more
quickly than usual.
Prevention – can you stop them?
Combing is an important part of good personal care but head lice are not easily damaged by it.
Good hair care may help to spot lice early and so help to control them. There is no evidence
that the old slogans "break its legs, so it can't lay eggs" or "a legless louse is an eggless louse"
have any truth in them.
The best way to stop infection is for families to learn how to check their own heads. This way
they can find any lice before they have a chance to breed. They can then treat them and stop
them going round the family.
The way to check heads is called "detection combing". It can be done as often as families want
to. The way to do it is described in NOTES FOR FAMILIES – HAVE YOU GOT HEAD LICE?
If a living, moving louse is found on one of the family's heads, the others should be checked
carefully. Then any of them who have living lice should be treated at the same time.
How to treat head lice
You should only ever treat someone for head lice if you have found a living, moving louse.
The best treatment is to use lotion (not shampoo) from the pharmacist or your local doctor's
surgery.
The way to use the lotion is given in NOTES FOR FAMILIES – HOW TO TREAT HEAD LICE.
If you are sure you have found living lice after proper treatment, don't keep putting more lotion
on; ask advice from the local pharmacist, the health visitor, your family doctor or the school
nurse.
If the problem won't go away
The problem may not be head lice at al . Often we think there are lice when there aren't really
any there. We all start to itch as soon as head lice are mentioned.
There are other causes for itching of the scalp. Using head louse lotion can make these worse.
Using lotion over and over again can cause skin irritation, which itself makes the head itch.
When living, moving lice are found, they can almost always be cleared by using the right lotion.
This will only work if enough of it is used, if it is put on in the right way, and if any other family
members or close friends who have lice are properly treated at the same time.
A day or two after using the lotion, you sometimes find little lice still there. These have hatched
out of the eggs since you put the lotion on and will be killed if you put the lotion on again after
seven days.
When you have got rid of the lice, you may still itch for two or three weeks. This doesn't mean
you stil have lice. Check the head carefully. Remember, you don't have head lice if you can't
find a living, moving louse.
When you have got rid of all the lice, the nits (empty egg cases stuck on the hairs) will still be
there. This doesn't mean you still have lice and you shouldn't treat again no matter how many
nits there are if you can't find a living louse.
People who think their children keep on getting head lice may have made the mistakes listed
above and may keep be "treating" lice that have long since been cleared, or were never even
there in the first place.
If children do really keep on having living lice, this is most likely to be due to not doing the
treatment properly and not treating all those close contacts who have also been found to have
lice. Remember, if infection really does keep on happening, it is almost always from a member
of the family or a close friend. It is rarely from other children in the classroom, except from a
"best friend".
If you still have problems, ask your family doctor, health visitor, local pharmacist or health visitor
if a wet-combing method to remove the head lice might help.
What the schools can do
Schools must remember that most lice are caught in the family and the local community, not in
the classroom.
"Alert" letters should not be sent out. These can cause an "outbreak" of imaginary lice.
Children who may have lice should not be excluded from school; if they do have lice, they will
probably have been there for weeks already. The school nurse can help the parents to know
how to detect whether there really are lice there and how to get rid of them if they are.
The school should give information on lice for parents and staff, including the importance of
regular detection combing and how to do it. Provision of information should be on a regular
basis, not just when there is thought to be an "outbreak" and should be done in conjunction with
the school nurse.
Talks for parents by the school nurse can be helpful.
What families can do
Make sure that all family members know about good hair care, including regular, thorough
combing.
The only way to control head lice that works is for the family to check their own heads.
Check all the family's heads every now and then with a special plastic detection comb from the
pharmacist's shop. Read NOTES FOR FAMILIES – HAVE YOU GOT HEAD LICE?
All the family means everyone (adults as well as children) in the same household.
Only if you are sure you have found living, moving head lice in your family or household,
tell your relatives and close friends so that they can check their own heads. Treat any of your
household you are sure have lice at the same time. Ask your local pharmacist, school nurse,
health visitor or family doctor which lotion you should use.
Remember, never use lotion unless you are sure you have found a living, moving head louse
(not nits).
Try not to worry too much about head lice. They are unpleasant, but they rarely do any
harm other than causing an itchy scalp.
APPENDIX 5: HEAD LICE: NOTES AND GUIDANCE FOR THE PRIMARY CARE TEAM
General
Please read the attached Report carefully.
Head louse infection is not primarily a problem of schools but of the wider community.
As for any other infectious conditions that occur in their patients, primary care teams should be
knowledgeable and competent in the control of head lice. They should be able to teach patients
the technique of detection combing and be prepared to advise appropriate treatment when there
is confirmed infection.
Health professionals should make sure that they are able to identify a louse at all stages of its
development. It helps to have a magnifying glass to hand.
Patients should be made aware that head lice are only transmitted by direct, prolonged, head-
to-head contact.
Specific
DO.
Do consider nominating a member of staff to be responsible for advising patients on head louse
problems. This may be a practice nurse or health visitor, but other non-clinical staff may be
appropriate as a first contact. If examination is thought necessary, referral can then be made.
Do liaise, as appropriate, with local pharmacists, school nurses, health visitors, head teachers,
infection control nurses and the consultant in communicable disease control. Only a concerted
approach can be effective.
Do adhere to the following principles of control:
Definite diagnosis, i.e. a living, moving louse found by detection combing
Listing and examination of contacts
Simultaneous thorough and adequate treatment of all confirmed cases with one of the standard chemical lotions
Repeat the treatment after seven days
Do make sure that the patients are provided with information, advice and support. At a first consultation, it may be sufficient to ensure that they know how to undertake detection combing and what to do if there are head lice present. See NOTES FOR FAMILIES – HAVE YOU GOT HEAD LICE?; HOW TO TREAT HEAD LICE; and HEAD LICE: THE TRUTH AND THE MYTHS. Do be aware that patients are often mistaken when they believe they have lice. Recurrent scalp problems may be missed if it is simply assumed without evidence that lice are the cause. Do make every effort to discourage unnecessary or inappropriate treatment with chemical treatments. Do make sure that patients know that the correct use of chemical lotions is the scientifically confirmed way to treat head louse infections. Do follow the British National Formulary's recommendation of two applications of lotion (not shampoo) seven days apart. Do resist the temptation to agree with parents' suggestions that a first course of treatment has failed, that "it must be a resistant strain", and that a further course of treatment should be given. There is no substitute for a proper professional assessment.
Do seek the advice of the local health protection team on appropriate chemical lotions.
Do bear in mind that different formulations of the same active ingredient may have different
efficacies. When a first treatment has definitely failed, it may be useful to try the same agent in
a different formulation.
DON'T…
Don't routinely refer patients to the school nurse.
Don't confirm a diagnosis of head louse infection unless you yourself have seen a living, moving
louse, or you have physical evidence from the patients; ask them to stick one of the lice on a
piece of paper with clear sticky tape and bring it in.
Don't recommend treatment unless a louse has been clearly identified (as described above). If
you do recommend treatment, ensure that it is performed adequately both in the patient and in
infected contacts.
Don't assume that "reinfections" or "treatment failures" are truly infections. Make sure that a
louse is found or produced.
Don't recommend retreatment without first of all establishing that living, moving lice are still
present after two applications of lotion seven days apart and after a full professional
assessment as to the ways in which the family may not have complied carefully with the first
attempt.
Don't recommend or support any mass action.
Don't support the use of electronic combs, repellent sprays or chemical agents not specifically
licensed for the treatment of head louse infections.
APPENDIX 6: HEAD LICE: NOTES AND GUIDANCE FOR COMMUNITY PHARMACISTS
General
Please read the attached Report carefully.
Head louse infection is not primarily a problem of schools but of the wider community.
Pharmacists are an important source of advice on the management of head louse infection.
They should be knowledgeable and competent on the subject, be able to teach patients the
technique of detection combing and be prepared to advise appropriate treatment.
Pharmacists have an especially important role in limiting chemical treatment to true cases of
infection, reducing unnecessary and inappropriate treatment and, thereby, reducing the risk of
further development of resistant strains of lice.
Health professionals should make sure that they are able to identify a louse at all stages of its
development. It helps to have a magnifying glass to hand.
Patients should be made aware that head lice are only transmitted by direct, prolonged, head-
to-head contact.
Specific
DO.
Do consider nominating a member of staff to be responsible for advising patients on head louse
problems.
Do liaise, as appropriate, with your local family practices, school nurses, health visitors, head
teachers, infection control nurses and the local health protection team. Only a concerted
approach can be effective.
Do adhere to the following principles of control:
Definite diagnosis, i.e. a living, moving louse found by detection combing
Listing and examination of contacts
Simultaneous thorough and adequate treatment of all confirmed cases with one of the standard
chemical lotions
Repeat the treatment after seven days
Do make sure that the patients are provided with information, advice and support. At a first
consultation, it may be sufficient to ensure that they know how to undertake detection combing
and what to do if there are head lice present. See NOTES FOR FAMILIES – HAVE YOU GOT
HEAD LICE?; HOW TO TREAT HEAD LICE; and HEAD LICE: THE TRUTH AND THE
MYTHS.
Do be aware that patients are often mistaken when they believe they have lice. Recurrent scalp
problems may be missed if it is simply assumed without evidence that lice are the cause.
Do make every effort to discourage unnecessary or inappropriate treatment with chemical
treatments.
Do follow the British National Formulary's recommendation of two applications of lotion (not
shampoo) seven days apart.
Do make sure that patients know that the correct use of chemical lotions is the scientifically
confirmed way to treat head louse infections.
Do resist the temptation to agree with parents' suggestions that a first course of treatment has
failed, that "it must be a resistant strain", and that a further course of treatment should be given.
There is no substitute for a proper professional assessment.
Do seek the advice of the local consultant in communicable disease control on appropriate
chemical lotions. Generally, dimethicone is now considered as first-line chemical treatment and
malathion or one of the pyrethroids as second-line treatment
Do bear in mind that different formulations of the same active ingredient may have different
efficacies. When a first treatment has definitely failed, it may be useful to try the same agent in
a different formulation.
Do ensure that you provide patients with an effective detection comb. This will have rigid,
plastic teeth set not more than 0.3 mm apart.
DON'T…
Don't routinely refer patients to the school nurse.
Don't assume a patient has head lice unless you yourself have seen a living, moving louse, or
you have physical evidence from the patients; ask them to stick one of the lice on a piece of
paper with clear sticky tape and bring it in.
Don't recommend treatment unless a louse has been clearly identified (as described above). If
you do recommend treatment, ensure that it is performed adequately both in the patient and in
infected contacts.
Don't assume that "reinfections" or "treatment failures" are truly infections. Make sure that a
louse is found or produced.
Don't recommend retreatment without first of all establishing that living, moving lice are still
present after two applications of lotion seven days apart and after a full professional
assessment as to the ways in which the family may not have complied carefully with the first
attempt.
Don't support the use of electronic combs, repellent sprays or chemical agents not specifically
licensed for the treatment of head louse infections.
APPENDIX 7: HEAD LICE: NOTES AND GUIDANCE FOR SCHOOL NURSES (OR OTHER
RESPONSIBLE SCHOOL HEALTH OFFICERS)
General
Please read the attached Report carefully. It is your professional duty to ensure that you are
fully informed and up-to-date with current scientific knowledge and practice.
Health professionals should make sure that they are able to identify a louse at all stages of its
development. It helps to have a magnifying glass to hand.
Parents and staff should be made aware that head lice are only transmitted by direct,
prolonged, head-to-head contact.
Specific
DO…
Do adhere to the following principles of control (see NOTES FOR FAMILIES – HAVE YOU GOT
HEAD LICE?; HOW TO TREAT HEAD LICE; and HEAD LICE: THE TRUTH AND THE
MYTHS):
Definite diagnosis, i.e. a living, moving louse found by detection combing
Listing and examination of contacts by the family
Simultaneous thorough and adequate treatment of all confirmed cases with one of the standard chemical lotions
Repeat the treatment after seven days
Do make a professional assessment of reported cases of head louse infection of any child in the
school. If the report is from the child's parent, make sure that the parents are provided with
information, advice and support. If the report is from a teacher, for example, that the child is
scratching continuously or that a moving louse has been seen on the head, it may be necessary
to examine the child to establish a diagnosis. If your knowledge of the parents is good, it may
be sufficient to make contact with them to ensure that they know how to undertake detection
combing and what to do if there are head lice present.
Do understand yourself and teach your families and school staff that the correct use of chemical
lotions is the scientifically confirmed way to treat head louse infections.
Do make every effort to discourage unnecessary or inappropriate treatment with chemical
treatments.
Do resist the temptation to agree with parents' suggestions that a first course of treatment has
failed, that "it must be a resistant strain", and that a further course of treatment should be given.
This may be an easier approach in a busy schedule, but is not in the best interests of the family.
There is no substitute for a proper professional assessment.
Do be prepared to do a domiciliary visit if that is the most tactful and effective way of dealing
with a case of head louse infection, especial y for a "problem family". You have the professional
skills and training to educate, persuade, inform, guide and support them.
Do play an active part in providing regular, accurate information about head lice to parents and
staff. This should be done in conjunction with your local consultant in communicable disease
control and the head teacher, and should preferably be integrated into a package along with
information on other health issues.
DON'T…
Don't undertake routine head inspections as a screening procedure. Detection combing should be done by parents, but it is important that they are given proper information, advice and support by you. This should be in accordance with the attached Report. Don't diagnose head louse infection unless you yourself have found a living, moving louse, or you have physical evidence from the parents; ask them to stick one of the lice on a piece of paper with clear sticky tape and bring it in to you or one of their other health advisers. Don't recommend the head teacher to send out "alert letters" to other parents. In fact, encouragement should be given not to do so. Don't recommend treatment unless a louse has been clearly identified (as described above). If you do recommend treatment, ensure that it is performed adequately both in the patient and in infected contacts. Don't assume that "reinfections" or "treatment failures" are truly infections. Make sure that a louse is found or produced. Don't recommend retreatment without first of all establishing that living, moving lice are still present after two applications of lotion seven days apart and after a full professional assessment as to the ways in which the family may not have complied carefully with the first attempt. Don't recommend or support any mass action. Don't support the use of electronic combs, repellent sprays or chemical agents not specifically licensed for the treatment of head louse infections. Don't wait until there is a perceived major outbreak and corresponding agitation in the school. A regular educational programme rather than a reactive "campaign" is more sensible.
APPENDIX 8: HEAD LICE: NOTES AND GUIDANCE FOR HEAD TEACHERS
General
Please read the attached Report carefully. Successful management of headlice relies on
school staff being well informed.
Head louse infection is not primarily a problem of schools but of the wider community. It cannot
be solved by the school, but the school can help the local community to deal with it.
Head lice are only transmitted by direct, prolonged, head-to-head contact.
Transmission of lice within the classroom is relatively rare. When it does occur, it is usually
from a "best friend".
Head lice will not be eradicated in the foreseeable future, but a sensible, informed approach,
based on fact not mythology, will help to limit the problem.
The perception by parents and staff, however, is often that there is a serious "outbreak", with
many of the children infected. This is hardly ever the case.
The "outbreak" is often an outbreak of agitation and alarm, not of louse infection: a societal
problem rather than a public health problem.
Specific
DO…
Do have a written protocol on the management of head louse infections, based on this Report
and this Appendix. If possible, agree a protocol for your area in consultation with the Local
Education Authority, the local consultant in communicable disease control, infection control
nurses, school nurses and, if appropriate, your colleagues in other schools.
Do make sure that your school nurse is informed in confidence of cases of head louse infection.
The school nurse will assess the individual report and may decide to make confidential contact
with the parents to offer information, advice and support.
Do keep individual reports confidential and encourage your staff to do likewise.
Do collaborate with your school nurse in providing educational information to your parents and
children about head lice, but do not wait until there is a perceived "outbreak". Send out
information on a regular basis, preferably as part of a package dealing with other issues.
Do consider asking your school nurse to arrange a talk to parents at the school if they are very
concerned. Be present yourself and encourage your staff to attend; they are just as likely to be
misinformed about head lice as the parents. You may prefer to arrange a separate talk for the
staff.
Do ensure, with the school nurse, that your parents are given regular, reliable information,
including instructions on proper diagnosis by detection combing, the avoidance of unnecessary
or inappropriate treatments, and the thorough and adequate treatment of definitely confirmed
infections and their contacts using a chemical lotion.
Do advise concerned parents to seek the professional advice of the school nurse, the family
practice or the local pharmacist.
DON'T…
Don't send out an "alert letter" to other parents. Don't exclude children who have, or are thought to have, head lice. Don't recommend or support any mass action, including wet combing campaigns. Don't agree with angry parents that routine head inspections should be reintroduced. They were never effective. Don't refer parents directly to the health protection team. The appropriate clinical advisers are the school nurse, the local pharmacist, the health visitor and the general practitioner. Don't take, or support, actions simply "to be seen to be doing something" (such as send out "alert letters").



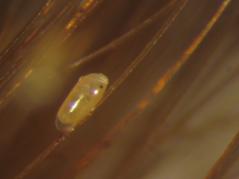

APPENDIX 9: LIFE CYCLE OF THE HEAD LOUSE
Life cycle/pictures produced with kind permission of Ian Burgess, Director Medical Entomology
Centre, Cambridge, UK and text reproduced from Head Lice Bulletin (Bulletin 893-01) produced
by Ohio State University
The head-louse life cycle (egg to adult) requires about 21 - 27 days on the human host. Each
adult female deposits anywhere from 50 -150 eggs (nits) during her lifetime. Nits hatch in 5 - 9
days. Nymphs (immatures) moult three times before becoming sexually mature adults. Young
and adult head lice feed on blood several times a day. The adult stage can live approximately
one month (30 - 40 days). The head-louse life cycle (egg to adult) requires about 21 - 27 days
on the human host. Each adult female deposits anywhere from 50 - 150 eggs (nits) during her
lifetime. Nits hatch in 5 - 9 days. Nymphs (immatures) moult three times before becoming
sexually mature adults. Young and adult head lice feed on blood several times a day. The adult
stage can live approximately one month (30 - 40 days).
Head lice are completely dependent on their human host for nourishment and warmth. In fact,
head lice cannot complete their life cycle if they become separated from their host. Adults and
nymphs can survive off their host for only 2 - 3 days, whereas nits can live for up to 14 days.
Life Cycle
APPENDIX 10: APPRAISAL OF EVIDENCE
For each type of research question there is an appropriate research method. Thus a question
about the prevalence of head lice should be considered by looking at cohort studies, while a
question about therapy would be answered by a randomised controlled trial. Systematic
reviews of all the randomised control trials about a particular therapy or all the cohort studies
describing prevalence have the advantage of putting the evidence into context. Thus the results
of systematic reviews carry a great deal of weight. Does this matter? The answer is yes –
different methodologies give different answers. The exact way the trial is carried out can affect
the result by as much as 30%; therefore if the benefit of the treatment was 20% but the trial was
not designed effectively, then the real truth may be that the treatment is causing harm! This is
why we should not only look for trials with a high (believable) level of evidence but also appraise
the quality of those trials.
In order to assess the evidence for the statements made in the Report, the statements were first
classified into the four categories shown in Table 1. This table also shows the types of research
likely to provide information on the different categories.
Table 1: Appropriate research methods for the different statement categories
Statement category
Systematic review, Cohort study' Cross-sectional study
Aetiology and risk factors
Systematic review, Cohort study, Case control study
Systematic review' Cross-sectional study
Systematic review, Randomised control trial Cohort study, Case control study
Searches in the literature were then undertaken for all articles with the terms "head lice", "head
louse", "lice", "louse" or "pediculus" in the text. The medical subject heading (MESH) "lice" was
also used. EMBASE, Cochrane and Medline (1966 onwards) were searched. No limits were
placed on the searches.
Articles were selected and independently appraised by two authors, using the format approved
by the Journal of the American Medical Association.36 37. The appraisal process used in-house
software for the generation of result data. Some trials were not included in the appraisals if a
more recent study had been performed. On the basis of these appraisals, studies were
classified according to the level of evidence they provide (see Table 2), and on this basis
grades of recommendation were allocated to each of the main claims within the Report.
Statements were categorised as grade A to D, where A is the strongest recommendation.
Table 2: Levels of evidence and grades of recommendation
Grade
of Level of Type of study
Systematic review of randomised control trials
Individual good-quality randomised control trial
Systematic review of cohort studies
Individual cohort study or low-quality randomised control trial (eg <80% follow-up)
"Outcomes" research; ecological studies
Systematic review of case-control studies
Individual case-control study
Case series (and poor-quality cohort and case-control studies)
Expert opinion without explicit critical appraisal, or based on physiology, bench research or "first principles"
APPENDIX 11: CLINICAL EFFECTIVENESS SUMMARY FOR CHEMICAL HEADLICE
TREATMENTS AND BUGBUSTING
The information in this brief summary has been drawn from the Clinical Evidence review by Ian
Burgess in 200620. It is intended to provide an indication of the current evidence for
effectiveness across a range of products that are currently available. 95% Confidence Intervals
(CIs), where not available, have been calculated using the original study data to provide an
indication of the reliability of the success rate reported. Wide confidence intervals indicate that
a result lacks reliability often due to small study size.
Recent evidence of effectiveness: Dimeticone
Dimeticone
Outcome of
formulation
comparison
interest
2 applications 7
2 applications 7
applications 7 days apart
Recent evidence of effectiveness: Malathion
Malathion
Outcome of
formulation
comparison
interest
(Malathion)
Lice eradication
8 hours overnight
mins, twice at 7
0.5% alcoholic /
hours/overnight/ 7
applications 7 days
Recent evidence of effectiveness: Permethrin
Outcome of
Permethrin
comparison
interest
formulation
Meinking et
cream rinse applied
al, 200428
Hill et al,
treated with single
tx of 1% permethrin
cream rinse applied
some with single
treatment of 0.5%
aqueous malathion
Recent evidence of effectiveness: Phenothrin
Phenothrin
Outcome of
formulation
comparison
interest
0.3% d-phenothrin
Lice eradication at
Lice free at 7 days
Phenothrin lotion,
Lice eradication at
Plastow et
al, 200135
applications 7 days
Burgess et
headlice after 2nd
al, 200525
reinfestation after
Recent evidence of effectiveness: Bugbusting
Method
Outcome of
comparison
interest
0.5% alcoholic /
Roberts et
al, 20006
malathion lotion
applied twice 8 hours/overnight/ 7 days apart
Phenothrin lotion,
Lice eradication at
Plastow et
al, 200135
Some treated with
Lice free at 5 days
Hill et al,
permethrin cream
group) or 15 days
rinse applied for
10 minutes, some
with single tx of 0.5% aqueous malathion
Comment 1: The RCT was conducted in an area where resistance to pyrethroids is widespread
35. There were differences in the use of combs and conditioners between the Phenothrin and BugBusting groups and differences in follow strategies that may have introduced bias and confounding 20. Comment 2: A single application of pediculocide is not considered to be best practice. Most of those in the pediculocide group who did not have successful eradication were found to have pyrethroid-resistant lice 20.
REFERENCES
1. The Stafford Group. Head Lice: a report for Consultants in Communicable Disease
Control (CCDCs) The Stafford Document. on behalf of the Public Health Medicine Environment Group. 1998. Ref Type: Generic
2. The Stafford Group. Head lice: evidence-based guidelines based on the Stafford Report.
J Fam Health Care. 12(5 Suppl), 1-21. 2002.
3. Downs AM, Harvey I, Kennedy CT, Downs AM, The epidemiology of head lice and
scabies in the UK. Epidemiology & Infection 1999;122:471-7.
4. Mumcuoglu KY. Prevention and treatment of head lice in children. Paediatric Drugs 1 (3),
5. Speare R, Buettner PG. Head lice in pupils of a primary school in Australia and
implications for control. International Journal of Dermatology 1999;38:285-90.
6. Roberts RJ, Casey D, Morgan DA, Petrovic M. Comparison of wet combing with
malathion for treatment of head lice in the UK: a pragmatic randomised controlled
trial.[see comment]. Lancet 2000;356:540-4.
7. Thomas DR, McCarroll L, Roberts R, Karunaratne P, Roberts C, Casey D, Morgan S,
Touhig K, Morgan J, Collins F, Hemingway J. Surveillance of insecticide resistance in
head lice using biochemical and molecular methods. Archives of Disease in Childhood
2006;91:777-8.
8. Burgess IF. Human lice and their management. [Review] [410 refs]. Advances in
Parasitology 1995;36:271-342.
9. Gratz NG. Human Lice: their prevalence, control and resistance to Insecticides. 1997.
Geneva, World Health Organisation.
10. Willems S, Lapeere H, Haedens N, Pasteels I, Naeyaert JM, De Maeseneer J et al. The
importance of socio-economic status and individual characteristics on the prevalence of
head lice in schoolchildren. European Journal of Dermatology 2005;15:387-92.
11. Mumcuoglu KY, Klaus S Kafka D Teiler M Miller J. Clinical observations related to head
lice infestation. Journal of the American Academy of Dermatology 25 (2 Pt 1), 248-251. 1991.
12. Taplin D, Meinking DL. Infestations. Pediatric dermatology, pp 1465-93. New York:
Churchill Livingstone, 1988.
13. North West Health Protection Unit. Headlice Guidance. 2006.
14. Health Protection Agency. Infection Control in Schools and other Child Care Settings.
15. Balcioglu C, Burgess IF, Limoncu ME, Sahin MT, Ozbel Y, Bilac C, Kurt O, Larsen KS.
Plastic detection comb better than visual inspection for diagnosis of head louse infection. Epidemiology and Infection 2008. (Published online by Cambridge University Press 04 Jan 2008).
16. Stallbaumer M, Ibarra J. Clinical efficacy of treatment for head lice. Counting head lice by
visual inspection flaws trials' results.[comment]. BMJ 1995;311:1369-70.
17. Does Dimeticone clear headlice? Drugs and Therapeutics Bulletin 2007;45:52-5.
18. Department of Health. The prevention and treatment of head lice. 2007. Pamphlet
19. Dodd CS. Interventions for treating headlice.[update in Cochrane Database Syst Rev.
2001;(2):CD001165; PMID: 11405977]. [Review] [3 refs]. Cochrane Database of Systematic Reviews 2000;CD001165.
20. Burgess I. Head lice.[update of Clin Evid. 2004 Jun;(11):2168-73; PMID: 15652106].
[Review] [25 refs]. Clinical Evidence 2005;2044-9.
21. Vander Stichele RH, Dezeure EM, Bogaert MG. Systematic review of clinical efficacy of
topical treatments for head lice.[see comment]. BMJ 1995;311:604-8.
22. Downs AM, Stafford KA, Harvey I, Coles GC. Evidence for double resistance to
permethrin and malathion in head lice.[see comment]. British Journal of Dermatology
1999;141:508-11.
23. Pollack RJ, Kiszewski A, Armstrong P, Hahn C, Wolfe N, Rahman HA, Laserson K,
Telford III SR, Spielman A. Differential permethrin susceptibility of head lice sampled in
the United States and Borneo. Archives of Pediatrics & Adolescent Medicine 1999;153
:969-73.
24. Bainbridge CV, Klein GL, Norbert SI, Hassman H, Ellis K, Manring D, Goodyear R,
Newman J, Micik S, Hoehler F, Walicke P. Comparative study of the clinical effectiveness
of a pyrethrum-based pediculocide with combing versus a permethrin-based pediculocide
with combing.[see comment][erratum appears in Clin Pediatr (Phila) 1998 Apr;37(4):276].
Clinical Pediatrics 1998;37:17-22.
25. Burgess IF, Brown CM, Lee PN. Treatment of head louse infestation with 4% dimeticone
lotion: randomised controlled equivalence trial. BMJ 2005;330:1423.
26. Burgess IF, Lee PN, Matlock G. Randomised, Controlled, Assessor Blind Trial Comparing
4% Dimeticone Lotion with 0.5% Malathion Liquid for Head Louse Infestation. PLosONE
2007;2.
27. British Medical Association and the Royal Pharmaceutical Society of Great Britain. British
National Formulary 54. 2007.
28. Meinking TL, Vicaria M, Eyerdam DH, Villar ME, Reyna S, Suarez G. Efficacy of a
reduced application time of Ovide lotion (0.5% malathion) compared to Nix creme rinse
(1% permethrin) for the treatment of head lice. Pediatric Dermatology 2004;21:670-4.
29. Downs AM. Managing Head Lice in an Era of Increasing Resistance to Insecticides. Am J
Clin Dermatol 2004;5 (3):169-77.
30. Burgess IF, Brown CM, Peock S, Kaufman J. Head lice resistant to pyrethroid insecticides
in Britain. BMJ 1995;311:752.
31. Hill N, Moor G, Cameron MM, Butlin A, Preston S, Williamson MS, Bass C. Single blind,
randomised, comparative study of the Bug Buster kit and over the counter pediculocide
treatments against head lice in the United Kingdom.[see comment]. BMJ 2005;331:384-7.
32. Dawes M. Combing and combating head lice.[comment]. BMJ 2005;331:362-3.
33. Takano-Lee M, Edman JD, Mullens BA, Clark JM. Home remedies to control head lice:
assessment of home remedies to control the human head louse, Pediculus humanus
capitis (Anoplura: Pediculidae). Journal of Pediatric Nursing 2004;19:393-8.
34. Chosidow O, Chastang C, Brue C, Bouvet E, Izri M, Monteny N, Bastuji-Garin S, Rousset
JJ, Revuz J. Controlled study of malathion and d-phenothrin lotions for Pediculus
humanus var capitis-infested schoolchildren.[see comment]. Lancet 1994;344:1724-7.
35. Plastow L, Luthra M, Powell R, Wright J, Russell D, Marshall MN. Head lice infestation:
bug busting vs. traditional treatment. Journal of Clinical Nursing 2001;10:775-83.
36. Guyatt GH, Sackett DL, Cook DJ. Users' guides to the medical literature. II. How to use
an article about therapy or prevention. B. What were the results and will they help me in
caring for my patients? Evidence-Based Medicine Working Group. JAMA 1994; 271:59-
63.
37. Guyatt GH, SD, Cook DJ. Users' guides to the medical literature. II. How to use an
article about therapy or prevention. A. Are the results of the study valid? Evidence-
Based Medicine Working Group. JAMA 1993;270:2598-601.
Source: http://www.phmeg.org.uk/files/1013/2920/7269/Stafford_Headlice_Doc_revise_2012_version.pdf
DONALD I. ABRAMS AND MANUEL GUZMAN Key Concepts ■ Cannabis has been used in medicine for thousands of years prior to achieving its current status as an illicit substance ■ Cannabinoids, the active components of Cannabis sativa, mimic the effects of the endogenous cannabinoids (the so-called endocannabinoids), activating specific cannabinoid receptors,particularly CB1 found predominantly in the central nervous system and CB2 found in cellsinvolved with immune function.
1 According to the author of the module, the compulsory readings do not infringe known copyright. COMPULSORY READINGS Readings #1 and #2 List of relevant readings :FromTextbook Revolution-Taking the Bite out of Books http://textbookrevolution.org/chemistry/ 1. Virtual Textbook of Organic ChemistryOrganic Chemistry by Wil iam Reusch 2. Organic Chemistry by Richard and Sal y Daley 3.Organic Chemistry Practice Problems by Wil iam Reusch