Kamagra gibt es auch als Kautabletten, die sich schneller auflösen als normale Pillen. Manche Patienten empfinden das als angenehmer. Wer sich informieren will, findet Hinweise unter kamagra kautabletten.
Powerpoint presentation
Review and its Relevance
to Hospice and Palliative Medicine
Hospice and Palliative Medicine Fellow
Grand Rapids Medical Education Partners
John Mulder, M.D.
Hospice and Palliative Medicine Fellowship Program Director
Grand Rapids Medical Education Partners
• A retrospective review and study (n=4,252) to determine the
most commonly prescribed medications in a population of
hospice patients.
•
Top ten of the 100 most frequently prescribed medications in
hospice patients:
1. Acetaminophen
2. Lorazepam
3. Morphines
4. Atropine
5. Haloperidol
6. Prochlorperazine
7. Albuterol
8. Docusate
9. Bisacodyl
10. Scopalamine
Sera L, et al. Commonly Prescribed Medications in a Population of Hospice
Patients.
AM J Hosp Pal iat Care. 2013.
• European Study/Survey (n=90), whose aim was to
identify a consensus of appropriate treatment for
common symptoms in the end of life care for
patients with cancer (based on consensus opinion).
• Four essential drugs were identified:
o Morphine o Midazolam o Haloperidol o Antimuscarinic
Lindqvist O, et al. Four Essential Drugs Needed for Quality Care of the Dying: A
Delphi-Study Based International Expert Consensus Opinion.
J Pal iat Med. 2013.
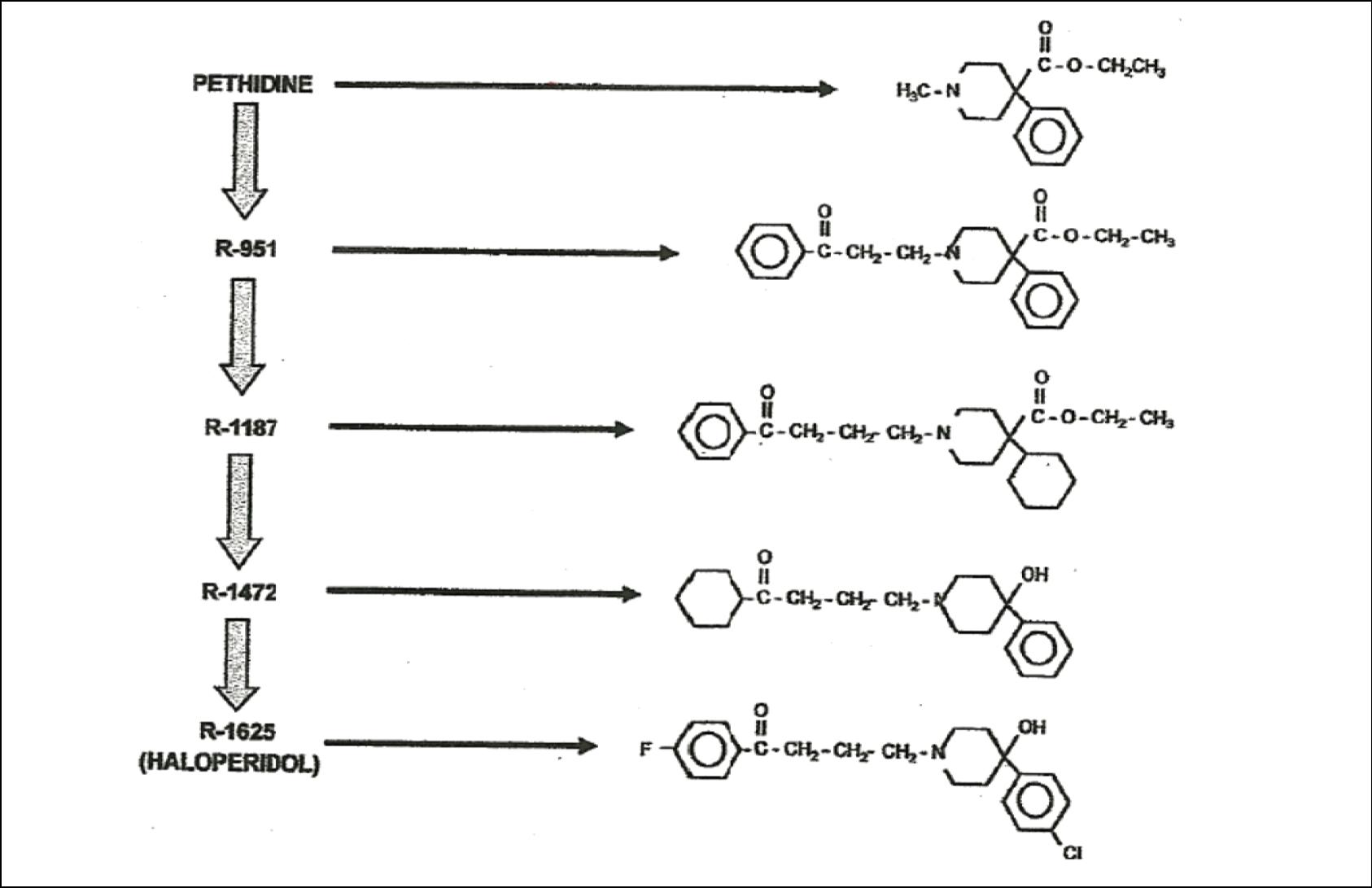
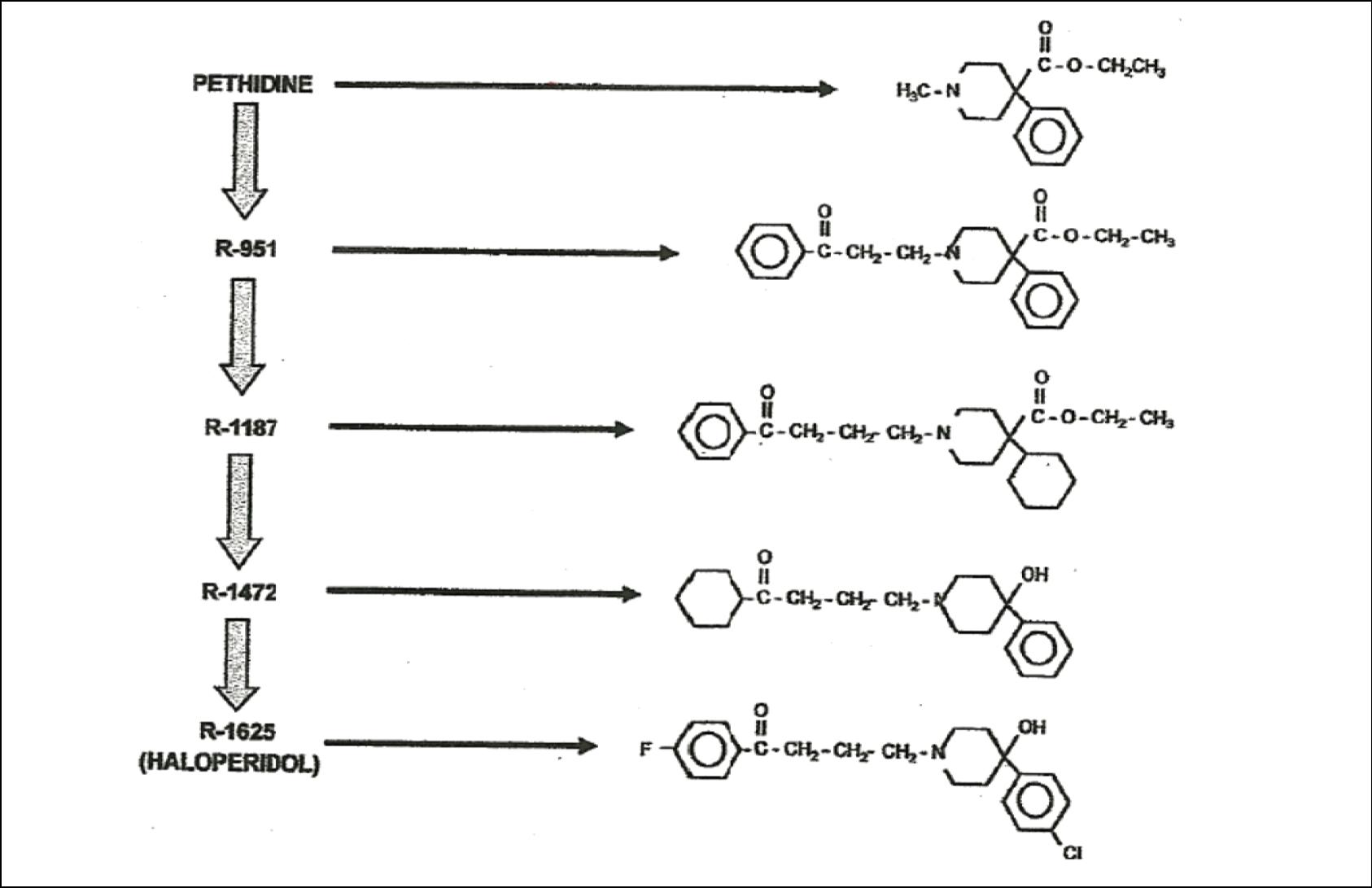
• Haloperidol has its origin in the research process of
central analgesic molecules derived from pethidine
(meperidine) and methadone, carried out by the
Belgian company Janssen Pharmaceutica in an
attempt to discover a new analgesic.
• Early animal studies revealed a potent tranquilizer
which exhibited antipsychotic activity as well as
analgesic qualities. In addition, it was found this
molecule produced Parkinsonism.
Landmarks in the history of Haloperidol:
•
1939 Otto Eisleb synthesized pethidine, a fundamental molecule in
the history of the discovery of Haloperidol
1953 Paul Janssen begins to carry out research
1958 Synthesis of R-1625 (Haloperidol) by Bert Hermans
1961 Johnson & Johnson acquires Janssen Pharmaceutica
1963 Arvid Carlsson demonstrates Haloperidol-induced changes to
dopamine levels in the brain; the "dopaminergic hypothesis of
schizophrenia" is born
1967 Synthesis of long-acting injectable Haloperidol (Haloperidol
1969 Haloperidol patent granted in the United States
1976 Solomon Snyder confirms that Haloperidol is a dopamine receptor
1982 Market launch of Haloperidol decanoate (Haldol®)
Cecilio LM. The consolidation of neuroleptic therapy: Janssen, the discovery of
Haloperidol and its introduction into clinical practice.
Brain Res Bull. 2009.
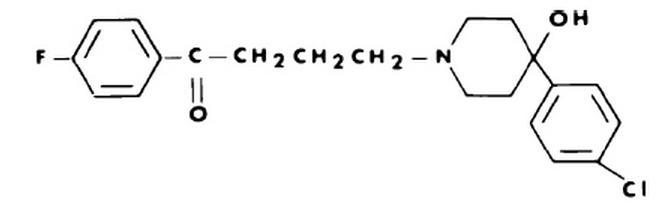
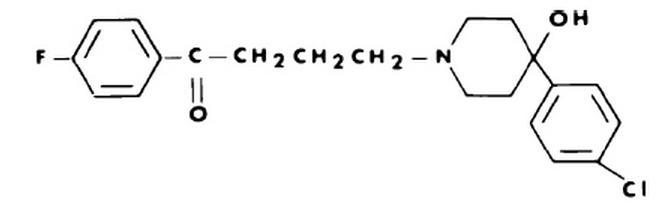
Haloperidol (Haldol®)
• A butyrophenone chain which appears to be
essential for D2 receptor binding
• Contains a piperdine ring and a ketone group
• The presence of the hydroxyl group enhances the
binding of Haloperidol to the D2 receptor
Haloperidol Pharmacology:
Pharmacodynamics
Pharmacokinetics
Pharmacodynamics may be simply defined as
what the drug does to the body, as opposed to
pharmacokinetics, which may be defined as
what the body does to the drug.
Haloperidol Pharmacodynamics
• Potent dopamine antagonist with a strong affinity
for the D2 dopamine receptor
• Weaker affinity to serotonin
• NMDA receptors, opioid (kappa, sigma, delta),
muscarinic, histamine, alpha-1 adrenergic,
substance P, and sodium channels
Haloperidol Pharmacodynamics
Stahl SM, et al. The psychopharmacology of ziprasidone: receptor-binding
properties and real-world psychiatric practice. J Clin Psychiatry. 2003.
Schotte A, et al. Risperidone compared with new and reference antipsychotic
drugs: in vitro and in vivo receptor binding. Psychopharmacology. 1996. Whittemore ER, et al. Antagonism of N-methyl-D-aspartate receptors by sigma site
ligands: potency, subtype-selectivity and mechanisms of inhibition. J Pharmacol
Exp Ther. 1997. Debonnel G, et al. Modulation of NMDA and dopaminergic neurotransmissions by
sigma ligands: possible implications for the treatment of psychiatric disorders. Life
Sci. 1996.
Haloperidol Pharmacokinetics
ABORPTION
METABOLISM
ELIMINATION
Onset of action:
Extensive protein
extensively in the
free fraction in the liver by CYP3A4
-Oral – first pass
Metabolites: -Reduced Haloperidol -Haloperidol glucuronide -inactive -Pyridium: toxicity
Haloperidol Pharmacokinetics
• SQ, Topical, PR – no pharmacokinetic data
• Duration of Action: (1-6 h) relative to route of
administration, dose [peak concentration (T-max)],
severity of clinical situation, and is a function of
distribution, metabolism, and elimination.
• Half life (t½): Oral t½ - 26h, IM t½ - 21h, IV t½ - 20h
Haloperidol Pharmacokinetics -
Kudo S, et al. Pharmacokinetics of Haloperidol: an update. Clin
Pharmacokinet. 1999. Holley FO, et al. Haloperidol kinetics after oral and intravenous doses. Clin
Pharmacol Ther. 1983. Schaffer CB, et al. Bioavailability of intramuscular versus oral Haloperidol in
schizophrenic patients. J Clin Psychopharmacol. 1982. Fang J, et al. Involvement of CYP3A4 and CYP2D6 in the metabolism of
Haloperidol. Cell Mol Neurobiol. 1997. Subramanyam B, et al. Identification of potentially neurotoxic pyridinium
metabolite in the urine of schizophrenic patients treated with Haloperidol.
Biochem Biophys Res Commun. 1991. Forsman A, et al. On the pharmacokinetics of Haloperidol. Nord J Psychiatr. 1974.
• Haloperidol is subject to hepatic blood flow,
protein binding, and intrinsic enzyme activity.
• It is thus potentially affected by liver disease and
dose modification may be necessary.
Gupta SK, et al. Effect of alosetron (a new 5-HT3 receptor antagonist) on the
pharmacokinetics of haloperidol in schizophrenic patients. J Clin Pharmacol.
Blaschke TF. Protein binding and kinetics of drugs in liver diseases. Clin
Pharmacokinet. 1997.
• No need for alteration of drug dosing in
renal insufficiency.
Prommer E. Role of Haloperidol in Paliative Medicine: An Update. AM J
Hosp Pal iat Care. 2011.
Hanks G, et al. Oxford Textbook of Paliative Medicine. 2010.
Drug Interactions
• Decreased levels of Haloperidol
o Carbamazepine o Phenobarbital o Phenytoin
• Increased levels of Haloperidol
o Fluoxetine (Prozac®) o Venlafaxine (Effexor®) o Nefazodone (Serzone-®) o Fluvoxamine (Luvox®) o Alprazolam (Xanax®)
Prommer E. Role of Haloperidol in Palliative Medicine: An Update. AM J Hosp
Pal iat Care. 2011.
• Extrapyramidal Side Effects
• QT Interval Prolongation and Torsades de
• Neuroleptic Malignant Syndrome
Extrapyramidal Side Effects (E.S.E.)
• Symptom complex resulting from a dopaminergic-
cholinergic imbalance at the level of the basal
• The high affinity of Haloperidol for the D2 receptor
results in a relative increase in interneuronal
o Acute dystonia – spasm of muscles – tongue, face, neck or back o Parkinsonism o Neuroleptic malignant syndrome o Akathisia o Tardive dyskinesia
E.S.E. (Cont'd.)
• Double-blind randomized trial (n=244)
• Haloperidol, chlorpromazine and lorazepam
• Low-dose Haloperidol is effective in treatment of
delirium with an extremely low prevalence of
extrapyramidal side effects.
• Not clinically significant Breitbart W, et al. A double-blind trial of Haloperidol, chlorpromazine,
and lorazepam in the treatment of delirium in hospitalized AIDS patients.
Focus. 2005.
E.S.E. (Cont'd.)
• Prospective blinded study (n=10)
• Patient receiving IV Haloperidol experienced
significantly less intense extrapyramidal symptoms
• Delirious patients have relatively lower levels of
acetylcholine, which may lessen the severity of
Menza M, et al. Decreased Extrapyramidal Symptoms With Intravenous
Haloperidol. J Clin Psychiatry. 1987.
E.S.E. (Cont'd.)
• Extrapyramidal Syndrome Presenting as Dysphagia:
• Usually responds to diphenhydramine
Gonzalez F. Extrapyramidal Syndrome Presenting as Dysphagia: A Case Report.
AM J Hosp Pal iat Care. 2008.
QT Interval Prolongation and
Torsades de Pointes (TdP)
• 1997-2008 • 70 cases of QT prolongation and/or TdP • 54 cases TdP with 80% preceded by QT prolongation • 3 patients experienced sudden cardiac arrest • Increased Risk:
o IV o ↑ Doses o High risk medical y complex situations o Pre-existing heart disease o Electrolyte imbalance o Antiarrhythmic agents
Prommer E. Role of Haloperidol in Pal iative Medicine: An Update. AM J Hosp
Pal iat Care. 2011.
QT Interval Prolongation and TdP
Huffman J, et al. QTc Prolongation and the Use of Antipsychotics: A Case
Discussion. Primary Care Companion J Clin Psychiatry. 2003. Hatta K, et al. The association between intravenous Haloperidol and prolonged
QT interval. J Clin Psychopharmacol. 2001. Hunt N, et al. The Association Between Intravenous Haloperidol and Torsades de
Pointes. Psychosomatics. 1995. Metzger E, et al. Prolongation of the Corrected QT and Torsades de Pointes
Cardiac Arrhythmia Associated with Intravenous Haloperidol in the Medical y Il . J
Clin Psychopharmacology. 1993.
Neuroleptic Malignant Syndrome
• A neurologic emergency associated with neuroleptics
• FEVER – Fever, Encephalopathy, Vitals unstable, Elevated
enzymes (Increased CPK), Rigidity of muscle
• Hyperkalemia, Hypercapnia, Acidosis, DIC, Leukocytosis,
• Incidence .07-2.2%
• Risks: IV, ↑ dose (rapid), Agitation, Cachexia, Dehydration Benzer T. Neuroleptic malignant syndrome. 2002. Bel amy CJ, et al. Neuroleptic malignant syndrome in traumatic brain injury patients treated
with Haloperidol. J Trauma. 2009. Jackson N, et al. Neuropsychiatric complications of commonly use palliative care drugs.
Postgrad Med. 2008.
• Lowers seizure threshold
• Among the first generation antipsychotics, it is
the phenothiazine class (chlorpromazine) that
carries the greatest risk (1.2%)
Pisani F, et al. Effects of psychotropic drugs on seizure threshold. Drug Saf.
2002. Hedges D, et al. Antipsychotic medication and seizures: a review. Drugs
Today. 2003. Remick RA, et al. Antipsychotic drugs and seizures. J Clin Psychiatry. 1979.
Adverse Effects by System
Cardiovascular: hypotension, hypertension, tachcardia,
dysrhythmia(s), QTc prolongation-torsades de pointes, sudden death
CNS: restlessness, anxiety, extrapyramidal reactions, dsytonic
reactions, pseudoparkinsonian signs and symptoms, tardive
dyskinesia, neuroleptic malignant syndrome, altered central
temperature regulation, akathisia, insomnia, euphoria, agitation,
drowsiness, depression, lethargy, headache, confusion, vertigo,
Dermatologic: hyperpigmentation, pruritus, rash, contact dermatitis,
alopecia, photosensitivity (rare)
Gastrointestinal: nausea, vomiting, anorexia, constipation, diarrhea,
hypersalivation, dyspepsia, cholestatic jaundice, obstructive
Genitourinary: urinary retention
Hematologic: leukopenia
Ocular: blurred vision
Respiratory: laryngospasm, bronchospasm
Spectrum Health Drug Quick Reference - Haloperidol (Haldol®)
Clinical Indications
• Nausea and vomiting
• Bowel Obstruction
• Palliative Sedation
• There is a legitimate evidence base for the
treatment of delirium with Haloperidol and it is
advocated for this use by most experts
• Hyperactive, hypoactive, mixed
Delirium (Cont'd)
• Prospective randomized trial (n=73)
• Tertiary care university hospital in Montreal, affiliated ICU
• Olanzapine vs. Haloperidol
• Clinical efficacy was similar in both treatment arms
• ↑ E.P.S. with Haloperidol (n=6) (↓ severity)
• Similar ↓ need for benzodiazepines
Skrobik YK, et al. Olanzapine vs Haloperidol: treating delirium in a critical care setting.
Intensive Care Med. 2004.
Delirium (Cont'd)
• Randomized double-blind trial (n=28)
• Korea University Medical Center
• Delirium significantly reduced in both groups
• E.P.S. (n=1), mild in Haloperidol group Han CS, et al. A double-blind trial of Risperidone and Haloperidol for the
treatment of delirium. Psychosomatics. 2004.
Delirium (Cont'd)
• Randomized, double-blind, placebo-controlled trial
• Large university hospital, Netherlands
• Low dose Haloperidol (1.5mg/d) administered
prophylactically for elderly hip surgery patients
• No efficacy demonstrated in reducing post-op delirium
• Reduced severity and duration of delirium
• Reduced hospital stay (↓ cost)
Kalisvaart K. Haloperidol prophylaxis for elderly hip-surgery patients at risk for delirium: a
randomized placebo-control ed study. J Am Geriatr Soc. 2005.
Delirium (Cont'd)
Breitbart W. Diagnosis and management of delirium in the terminal y il .
Topics in Palliative Care. 2001. Breitbart W, et al. A double-blind trial of Haloperidol, chlorpromazine,
and lorazepam in the treatment of delirium in hospitalized AIDS patients.
Am Jour of Psychiatry. 1996.
Treatment of Delirium
• Mild agitation – 2mg PO, IV, IM
• Moderate agitation – 5mg
• Severe agitation – 7.5-10mg
• Decrease dose by 1/3 for elderly patients
• May repeat q 30 min – patient calm yet arousable to voice
• If serious agitation persists, double dose in 30 min – may repeat
• When symptom control is achieved, 24hr dose QD, BID
Goldstein, Morrison. Evidence-Based Practice of Pal iative Medicine. 2013.
Nausea and Vomiting
Glare P, et al. Treating nausea and vomiting in pal iative care: a review. Clin
Interv Aging. 2011.
Nausea and Vomiting (Cont'd)
• A review of the literature which identified 3 studies which
provided enough information on base line symptoms,
interventions, outcome measures, and evaluation tools
• Haloperidol may be effective in patients experiencing
nausea and vomiting
• No randomized controlled trials evaluating Haloperidol
for nausea and vomiting
• The clinical use of Haloperidol for nausea and vomiting
must be guided by clinical experience, judgment, case
reports, and expert opinion
Critchley P, et al. Efficacy of Haloperidol in the treatment of nausea and vomiting
in the pal iative patient: a systematic review. J Pain Symptom Manage. 2001.
Nausea and Vomiting (Cont'd)
• 0.5mg – 1.5mg q 6-12h, up to 5mg q 12h IV/SQ
• SQ/IV = ½ PO
Tucker R, et al. Managing Nonpain Symptoms. UNIPAC 4: A Resource for Hospice
and Pal iative Care Professionals. 2012.
Nausea and Vomiting (Cont'd)
• Retrospective study
• Trial 1 (n=23), 74% reported the use of LDH ↓ their
• Trial 2 (n=10), 70% reported relief Bleicher J, et al. Lorazepam, Diphenhydramine, and Haloperidol Transdermal Gel
for Rescue From Chemotherapy-Induced Nausea/Vomiting: Results of Two Pilot
Trials. J Support Oncol. 2008.
ABHR Gel in the Treatment
of Nausea and Vomiting in
the Hospice Patient
Moon, R. Inter J of Pharma Compounding. 2006.
Nausea and Vomiting (Cont'd)
Haloperidol "has been extremely effective
in doses from 5-20mg/d and remains
our antiemetic of choice in most situations."
Storey P, et al. Subcutaneous Infusions for Control of Cancer Symptoms. J Pain
and Symp Mgmt. 1990.
Bowel Obstruction
• May be useful as an antiemetic in the treatment of
malignant bowel obstruction
• However, has not been compared with other
antiemetics in a randomized controlled trial.
Ventafridda V, et al. The management of inoperable gastrointestinal obstruction
in terminal cancer patients. Tumori. 1990. Ripamonti C, et al. Clinical-practice recommendations for the management of
bowel obstruction in patients with end-stage cancer. Support Care Cancer. 2001.
Intractable Hiccups (IH)
• Retrospective chart review (n=240)
• 3 subjects with IH were identified
• Haloperidol (n=1), Chlorpromazine, Baclofen, and
Carbamazepine proved effective
Kumar A, et al. Intractable hiccups during stroke rehabilitation. Arch Phys Med
Rehabil. 1998.
• 2 case studies in which IM Haloperidol (2mg)
followed by a PO regimen (2d) was effective in
treatment of IH without recurrence
• Mention of 7 additional cases Ives TJ, et al. Treatment of intractable hiccups with intramuscular Haloperidol. Am
J Psychiatry. 1985.
• Useful in treatment of anxiety when
benzodiazepines are not sufficient for symptom
• Psychotic symptoms accompany the anxiety
• Avoids excessive sedation Hanks G, et al. Oxford Textbook of Pal iative Medicine. 2010.
Palliative Sedation
• Palliative sedation is often used at end of life for
refractory symptoms such as delirium, nausea,
dyspnea, and pain
o 0.5mg – 5mg PO/SQ a 2-4h OR o 1-5mg IV/SQ then infusion 5-15mg/d SQ/IV
Rousseau P. Palliative sedation in the management of refractory symptoms. J
Support Oncol. 2004.
Palliative Sedation (Cont'd)
• National Taiwan University Hospital (n=251)
• 70 patients received palliative sedation
• 35 patients received Haloperidol
• Did not influence survival time
• Surveys of staff and families indicated Haloperidol
was an effective agent for palliative sedation
Chiu TY, et al. Sedation for refractory symptoms of terminal cancer patients in
Taiwan. J Pain Symptom Manage. 2001.
Innovative Uses of
•Analgesic Adjunct •Pruritus
Analgesic Adjunct
• Anesthesia and psychiatric literature provide well
designed studies and case reports that
demonstrate the efficacy of Haloperidol as well as
other neuroleptics as an analgesic adjunct
• Mixed results
• Most studies appear to be in the favorable camp
• Mμ, NMDA, -1 adrenergic, substance P receptors
• Na╫ channels
• Isometric similarity to meperidine
Analgesic Adjunct References
Colclough G, et al. Epidural Haloperidol enhances epidural morphine
analgesia: three case reports. J Opioid Manage. 2008. Kotake Y, et al. Additional Droperidol, not Butorphanol, augments
epidural fentanyl analgesia following anorectal surgery. J Clin Anes.
2000. Maltbie A, et al. Analgesia and Haloperidol: a hypothesis. J Clin
Psychiatry. 1979. Judkins KC. Haloperidol as an adjunct analgesic in the management of
post operative pain. Anaesthesia. 1982. Hanks GW, et al. The Myth Of Haloperidol Potentiation. The Lancet. 1983.
Analgesic Adjunct (Cont'd)
• Well designed retrospective study
• Patients receiving short-acting opioids
• Low-dose methadone in conjunction with
adjuvent Haloperidol resulted in excellent pain
control without dose escalation or opioid-
induced hyperalgesia
Salpeter S, et al. The Use of Very-Low-Dose Methadone for Palliative Pain Control
and the Prevention of Opioid Hyperalgesia. J Pal iative Med. 2013.
Organic Causes of Pruritus:
"Psychologic" causes of
• Hepatic disease
pruritus and self-excoriation:
• Renal disease
• Anxiety disorder (primary
• Obsessive-compulsive
• Depressive disorder
(primary or secondary)
• Personality disorder
(especially borderline)
• Collagen vascular disease • Psychosis
When there is a psychological component, or
delusional ideation, or agitation is prominent, the
author recommends considering Haloperidol
Fried R. Evaluation and treatment of "psychogenic" pruritus and self-excoriation. J
Am Acad Dermatol. 1994.
• Effective and essential medication for symptom
management in Hospice and Palliative patients
due to its unique pharmacodynamic profile.
• Dose: start low and go slowly
• Adverse effects: increased in medically
complex patients with high risk clinical situations
Source: http://www.leadingagemi.org/resource/resmgr/2014_AC_Session_Handouts/Haloperidol_Revised_05_14.pdf
D-level Essay in Statistics 2009 How to Analyze Change from Baseline: Absolute or Percentage Change? Högskolan Dalarna Lars Rönnegård 781 88 Borlänge Tel vx 023-778000 Richard Stridbeck How to Analyze Change from Baseline: Absolute or Percentage Change? In medical studies, it is common to have measurements before and after some medical interventions. How to measure
ANTIOXIDANTS & REDOX SIGNALINGVolume 15, Number 7, 2011 FORUM REVIEW ARTICLE ª Mary Ann Liebert, Inc.DOI: 10.1089/ars.2010.3739 Oxidative Stress as Pathogenesis of Cardiovascular Risk Associated with Metabolic Syndrome Metabolic syndrome (MetS) is characterized by accumulation of visceral fat associated with the clustering ofmetabolic and pathophysiological cardiovascular risk factors: impaired glucose tolerance, dyslipidemia, andhypertension. Although the definition of MetS is different among countries, visceral obesity is an indispensablecomponent of MetS. A growing body of evidence suggests that increased oxidative stress to adipocytes is centralto the pathogenesis of cardiovascular disease in MetS. Increased oxidative stress to adipocytes causes dysre-gulated expression of inflammation-related adipocytokines in MetS, which contributes to obesity-associatedvasculopathy and cardiovascular risk primarily through endothelial dysfunction. The purpose of present reviewis to unravel the mechanistic link between oxidative stress and cardiovascular risk in MetS, focusing on insulinresistance, hypertension, and atherosclerosis. Then, therapeutic opportunities translated from the bench tobedside will be provided to develop novel strategies to cardiovascular risk factors in MetS. Antioxid. RedoxSignal. 15, 1911–1926.