Kamagra gibt es auch als Kautabletten, die sich schneller auflösen als normale Pillen. Manche Patienten empfinden das als angenehmer. Wer sich informieren will, findet Hinweise unter kamagra kautabletten.
Pedspainmedicine.org
SPA Pain Meeting syllabus 2014
Developmental Pharmacokinetics/Pharmacodynamics of Parenteral Opiates and NSAIDS in Infants: What are the Problems?
The development of microassay techniques for drug concentrations in the late 1970s and 1980s allowed investigations of the metabolism of drugs in pediatric populations. The study of pharmacokinetics (drug distribution and handling in the body-PK) in children and infants and of pharmacodynamics (the effects of drugs on the body – PD) grew as small blood/serum samples could be analyzed for drug concentrations. Computer-assisted analysis of concentration vs. time graphs facilitated computation of pharmacokinetic parameters, such as clearance, volume of distribution and elimination half-life. This information showed differences between adult drug handling and that found in children and infants, helping to explain the different effects or durations of effect seen. Applying these analyses to opiate analgesics involved many investigators including this speaker. Pharmacodynamic effects may be more complex since this involves not only pharmacokinetic factors, but factors such as access to sites of action, different receptor avidity or number which may differ in different ages, races, ethnicities or with different genetic variants linked to opiate action.
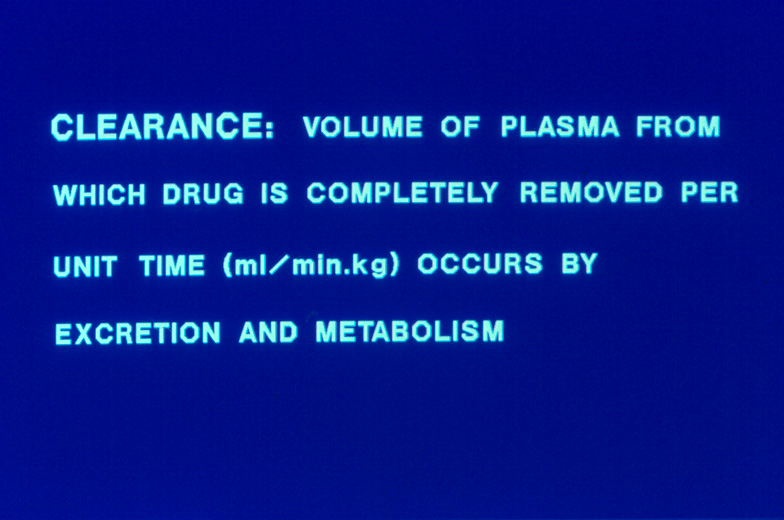
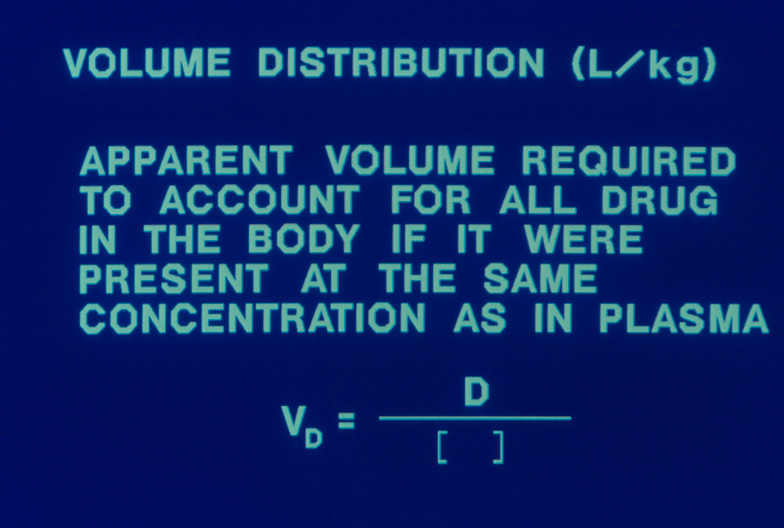
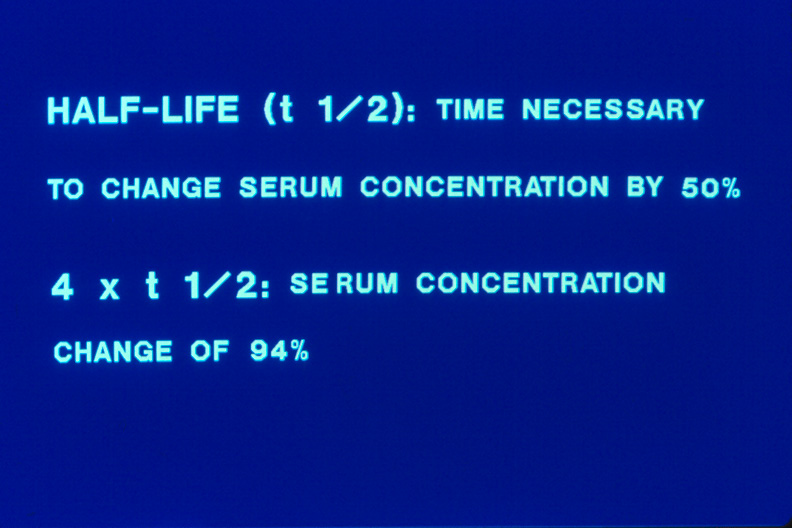
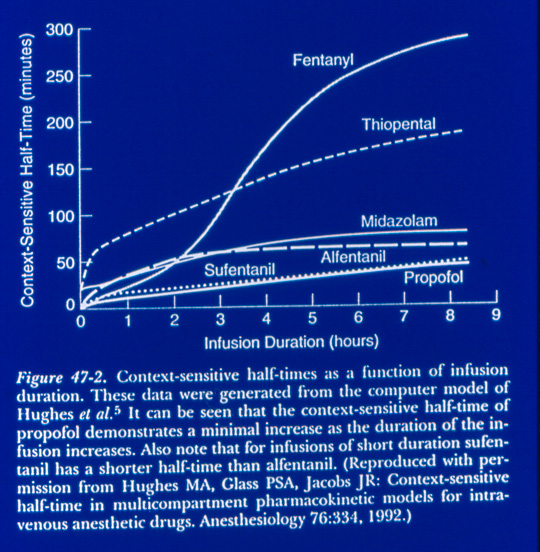
To begin, I want to define some PK terms reported in most PK studies- clearance, volume of distribution and half-life. Clearance is defined as the volume (usually of blood or serum) from which drug is removed in a unit of time (L/hr, mL/min), often corrected for weight to allow comparison across pediatric groups (L/hr/kg, mL/min/kg). Volume of distribution represents the volume necessary to account for the measured concentration after a drug dose, Vd= dose/concentration. This may or may not be equal to any real volume (such as blood volume or extracellular fluid volume) but shows how widely distributed a drug is in the body or how wel a blood concentration reflects how much drug is present in the body. Small Vd is seen in drugs that don't cross cell membranes easily due to large size, ionization or extensive binding to serum proteins. Half-life is a time term (min, hr) which represents the time needed to change drug concentration by 50%. Elimination half-life, t ½, occurs due to metabolism – renal, hepatic or other pathways and excretion of unchanged drug.
This talk will focus on 2 opiates used widely in pediatric anesthesia and critical care, morphine and fentanyl. Many investigators have reported studies with these agents; I have been involved in the study of morphine in infants. In 1984, we reported a group of 44 children treated with morphine infusions following cardiac surgery (1). Children were able to wean from mechanical ventilation with normal PaCO2 (during morphine infusions of 10-30 mcg/kg/hr) with [Mo]ss < 30 ng/mL. A subset of older children reported good verbal pain scores if [Mo]ss was over 12 ng/mL.
Pharmacokinetic evaluation of infants and children, most following cardiac surgery, showed a pattern seen with many drugs – initial low clearance which increased to reach adult values by 6 months, a slightly higher volume of distribution and an elimination half-life which is prolonged in infants reaching adult values at 6 months (2, 3). Subsequent studies in infants having non-cardiac surgery showed the same pattern but adult morphine clearance was reached more quickly, by 1-3 months of age (4). Several
of our studies focused on the respiratory effects of morphine infusions, showing those infants with [Mo]ss > 20 ng/mL had a high incidence of hypercarbia and depressed CO2 response curves slopes (5). Comparing morphine infusion to bolus dosing in postoperative infants showed acceptable analgesia in both groups with fewer scores showing pain in the infusion group (6). Four of 57 (7%) infants showed respiratory depression/hypercarbia, all in the infusion group. In all of these studies variability between infants was notable, often 3-fold. Other groups completed PK studies in similar postoperative populations and in premature infants, with similar patterns and the large inter-patient variability (7, 8, 9).
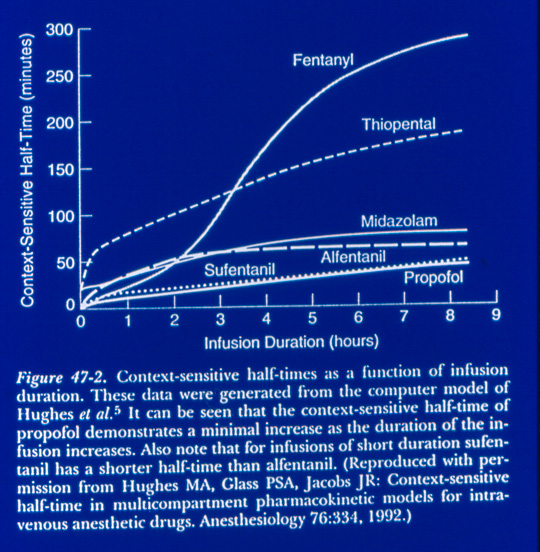
Pharmacokinetic studies of fentanyl, sufentanil, alfentanil, meperidine follow the same pattern, including the between patient variability (10, 11). Age and the closely-linked weight showed an important correlation with pharmacokinetic values, with a 2-3 fold inter-patient variability in drug concentrations. The choice of morphine or fentanyl for postoperative use seems a choice made by institutional tradition rather than by major differences in effects (12).
Several research groups (Knibbe, Krekels, Tibboel, Encinas, Anderson – 13-15) have done sophisticated modeling of morphine and fentanyl to improve prediction of drug dosing. These are elegant studies but a level of uncertainty remains for the clinician treating an individual infant. Current investigators, including Jimenez, Galinkin, Cohen and others who are studying the ethnic, racial, and genetic factors affecting opiate handling will help to inform this arena.
In the meantime, my clinical approach is to titrate opiate doses, particularly in infants breathing spontaneously:
for morphine – 0.05 mg/kg load and infusions at 5-10 mcg/kg/hr in newborns and 10-20 mcg/kg/hr in infants(lower dose in cardiac surgical babies);
for fentanyl – 0.5 mcg/kg load and infusions at 1 mcg/kg/hr.
This assumes one may have an infant with low clearance but does not preclude adding more if clinical signs show an inadequate response. A recent report from Taylor suggests that morphine infusion dosing does not follow clearance maturation with infusion rates plateauing at 22 mcg/kg/hr by age 5y. (16) They also note increasing variability in dosing with increasing age, suggesting other factors are at play.
Many clinical studies support the use of non-opiate analgesics to augment pain relief at lower opiate doses( 17, 18). In the US, ketorolac is the only parenteral NSAID available. Ketorolac is a racemic mixture of R- and S-isomers. The S-isomer is the more potent analgesic and anti-inflammatory compound. While several groups have reported ketorolac kinetic parameters, many report composite values for the racemate (19, 20). Hamunen and Kauffman showed that these 2 isomers have different kinetics in children and adults (21, 22). We studied the stereospecific pharmacokinetics of ketorolac in infants and toddlers (23). In 6-18 month old postoperative infants and children, the S-isomer showed rapid clearance. The same pattern was seen in infants 2-6 months given a single dose following surgery (24). No changes in renal or hepatic function occurred nor was there difference in surgical drain amounts. Modeling of the PK parameters show the S-isomer is cleared with repeat dosing q 6h while the R-isomer
accumulates. Unknown is whether this bears any relation to the toxicity seen with longer-term use of ketorolac. Multiple dose studies are needed.
In broadening the definition of multimodal therapies, non-pharmacologic therapies have a definite but incompletely-explored role to play. The use of swaddling, non-nutritive sucking, sucrose have shown positive effects in comfort in some studies. Another modality that needs systematic study is acupuncture. A retrospective review of our experience in infants (25) showed it to be of benefit in a small number of infants without limiting side effects but much more needs to be done to establish its place in care of postoperative infants or in those requiring critical care.
1. Lynn AM, Opheim KE, Tyler DC. Morphine infusions fol owing pediatric cardiac surgery. Crit Care
Med 1984; 12:863-866
2. Lynn AM, Slattery JT. Morphine pharmacokinetics in early infancy. Anesthesiol 1987; 66:136-139 3. McRorie TI, Lynn AM, Nespeca MK, Opheim KE, Slattery JT. Maturation of morphine disposition.
Am J Dis Child. 1992; 146:972-976
4. Lynn AM, Nespeca MK, Bratton SL, Strauss SG, Shen DD. Clearance of morphine in postoperative
infants during intravenous infusions: Influence of age and surgery. Anesth Analg 1998; 86:958-963
5. Lynn AM, Nespeca MK, Opheim KE, Slattery JT. Respiratory effects of intravenous morphine
infusions in neonates, infants and children following cardiac surgery. Anesth Analg 1993; 77:695-701
6. Lynn AM, Nespeca MK, Bratton SL, Shen DD. Intravenous morphine in postoperative infants:
intermittent bolus dosing versus targeted continuous infusions. Pain 2000; 88:89-95
7. Bouwmeester NJ, Anderson BJ, Tibboel D, Holford NHG. Developmental pharmacokinetics of
morphine and its metabolites in neonates, infants and young children. Br J Anaesth 2004; 92: 208-217
8. Pokela ML, Olkkola KT, Seppala T, Koivisto M. Age-related morphine kinetics in infants. Dev
Pharmacol Ther 1993; 20:26-34
9. Anand KJS, Anderson BJ, Holford NHG et al. Morphine pharmacokinetics and pharmacodynamics
in preterm and term infants: secondary results from the NEOPAIN trial. Br J Anaesth 2008; 101: 680-689
10. Koehntop DE, Rodman JH, Brundage DM et al. Pharmacokinetics of fentanyl in neonates. Anesth
Analg 1986; 65:227-232
11. Collins C, Koren G, Crean P et al. Fentanyl pharmacokinetics and hemodynamics in preterm
infants during ligation of patent ductus arteriosus Anesth Analg 1985; 64:1078-1080
12. Saarenmaa E, Huttunen P, Leppaluoto J et al. Advantages of fentanyl over morphine in analgesia
for ventilated newborn infants after birth: a randomized trial. J Pediatr 1999; 134:144-150
13. Krekels EHJ, DeJongh J, van Lingen RA et al. Predictive performance od a recently developed
population pharmacokinetic model for morphine and its metabolites in new datasets of (preterm) neonates, infants and children. Clin Pharmacokinet 2011; 50:51-63
14. Krekels EHJ, vanHasselt GC, Tibboel D, Danhof M, Knibbe CAJ. Systematic evaluation of the
descriptive and predictive performance of pediatric morphine population models. Pharm Res 2011; 28:797-811
15. Encinas E, Calvo R, Lukas JC et al. A predictive pharmacokinetic/pharmacodynamic model of
fentanyl for analgesia/sedation in neonates based on a semi-physiologic approach. Pediatr Drugs 2013; 15:247-257
16. Taylor J, Liley A, Anderson BJ. The relationship between age and morphine infusion rate in
children. Ped Anesth 2013; 23:40-44
17. Splinter WM, Reid CW, Roberts DJ et al. Reducing pain after inguinal hernia repair in children:
caudal anesthesia versus ketorolac tromethamine. Anesthesiol 1997; 87:542-546
18. Munro HM, Walton SR, Malviya S et al. Low-dose ketorolac improves analgesia and reduces
morphine requirements following posterior spinal fusion in adolescents. Can J Anaesth2002; 49:461-466
19. Olkkola KT, Maunuksela EL. The pharmacokinetics of postoperative intravenous ketorolac
tromethamine in children. Br J Clin Pharmacol 1991; 31:182-184
20. Dsida RM, Wheeler M, Birmingham PK et al. Age-stratified pharmacokinetics of ketorolac
tromethamine in pediatric surgical patients. Anesth Analg 2002; 94:266-270
21. Hamunen K, Maunuksela EL, Sarvela J et al. Stereoselective pharmacokinetics of ketorolac in
children, adolescents and adults. Acta Anesthesiol Scand 1999; 43:1041-1046
22. Kauffman RE, Lieh-Lai MW, Uy HG et al. Enantiomer-selective pharmacokinetics and metabolism
of ketorolac in children. Clin Pharmacol Ther 1999; 65:382-388
23. Lynn AM, Bradford H, Kantor ED et al. Postoperative ketorolac tromethamine use in infants
aaged 6-18 months: the effect on morphinr usage, safety assessments and stereo-specific pharmacokinetics. Anesth Analg 2007; 104:1040-1051
24. Lynn AM, Bradford H, Kantor E et al. Ketorolac tromethamine: stereo-specific pharmacokinetics
and single dose use in postoperative infants aged 2-6 months. Ped Anesth 2011; 21:325-334
25. Gentry KR, McGinn KL, Kundu A, Lynn AM. Acupuncture therapy for infants:a preliminary report
on reasons for consultation, feasibility and tolerability. Ped Anesth 2011; 22 690-695
DEVELOPMENTAL
KINETICS/DYNAMICS OF
PARENTERAL OPIOIDS AND NSAIDS
IN INFANTS
Anne M. Lynn MD Professor, Anesthesiology and Pediatrics University of Washington Seattle Children's Hospital
CONFLICT OF INTEREST
None Most drugs do not have labeling for use in infants
Review with focus on infants pharmacokinetic terms
Clearance, volume of distribution, half-life
Kinetics of morphine and fentanyl Kinetic modeling approaches Kinetics of ketorolac Suggested clinical approach


Children's Hospital and
Children's
Regional Medical
Hospital

Morphine Pharmacokinetics in Infants, 1987
10 term infants ≤ 10 weeks
Age (days)
Clearance
Half-life
(mL/kg/min) distribution
Morphine Metabolism in Infants and Toddlers, 1992
49 children, 1 day-2.5 years, post-cardiac surgery
Clearance
Volume of
Half-life
(mL/kg/min)
Respiratory Effects of Morphine Infusions After Cardiac Surgery, 1993
30 neonates, infants, and children
PaCO >
CO Response
Slope <
No difference in respiratory depression by age at
Morphine in Post-Operative Infants: Infusion vs. Bolus Dose, 2000 N=83, infn 57, bolus 26
• Analgesia better with infusion
(pain in 13% vs. 32%)
• Oximetry < 90% (RA) same
(2.3% vs. 2.5% of POD1)
• Ventilation effects in infusion group
(4/57 = 7%) Increased PvCO in 2, desat. in 1, both in 1
• PO intake 16hrs post-op in both groups
Morphine Metabolism: Effect of Age and Surgery, 1998
29 infants, clearance during infusions
Age (days)
Non-Cardiac
Cardiac Surgery
Interpatient variability 2-3 fold
Morphine Clearance
Morphine Study Noncardiac Surgery
Rate for [Mo] ss =
Morphine vs. Fentanyl Neonate/Infant Analgesia
Saarenmaa, J Pediatr 1999; 134:144-50
Randomized, double-blind trial ventilated newborns N=163 Fentanyl – 10.5 mcg/k load, infuse 1.5 mcg/k/h Morphine – 140 mcg/k load, infuse 20
No difference in HR, BP, pressor use, length ventilation,
opiate bolus doses, behavioral scores during suction
[Epi] and [Norepi] decreases Difference in [beta-endorphin] – lower in fentanyl fewer with decreased GI motility in fentanyl
Pharmacokinetic Modeling
Population PK models use factors influencing
PK variables related to age, weight as regular covariates with other covariate factors, assessing improvement of model
Weight-based allometric models incorporate
weight using exponential factors(0.75 for Clearance, 1 for Volume) augmented by age-based functions, eg bili or creat.
Both models have been used for morphine
and fentanyl in neonates
Fentanyl Kinetics in neonates Model vs. values in literature
Parameter
Model Calculated Literature Value
Value
Encinas E. Predictive PK/PD model fentanyl in neonates Pediatric drugs
2013; 15:247-57
Fentanyl modeling
Opiate Dosing in Infants
Two to three-fold variability in opiate
clearance and models makes individual infant dosing hard
This supports ongoing studies of ethnic,
racial and genetic factors important to help individualize care
My approach is to titrate to minimize the risk
to the slow metabolizing infant
Morphine 0.05 mg/kg load, then infusion 5-10
mcg/kg/hr in neonate to 10-20 mcg/kg/hr in infants
Fentanyl 0.5 mcg/kg, then infusion at 1 mcg/kg/hr
Nonsteroidal anti-inflammatory drug (NSAID) Inhibits prostaglandin synthesis Analgesia not opiate-receptor related Drug effects on renal, gastric mucosa,
platelet function
No drug effects on respiration,
Only parenteral NSAID released in U.S.
Ketorolac: Pharmacokinetics
Cyclic propionic-acid derivative Racemic mixture, S-isomer active analgesic,anti-
Tromethamine salt to increase solubility Adult plasma level after 30 mg:
Therapeutic range: 0.3-5 mcg/ml
Ketorolac in Infants Why?
Morphine infusions give good analgesia
but respiratory depression in 7% of infants.
Can using ketorolac decrease this to 0%? Does ketorolac have an acceptable safety
profile in infants?
Ketorolac in Postop. Infants
Intra- or postoperative use in children decreases opiate usage Splinter WM Anesthesiol. 87:542-6; 1997 Munro HM Can J Anesth. 49:461-6; 2002 Use of NSAIDs in infants: 11% in neonates (1-30 d) to 59% in infants (3-12
deLima J BMJ. 313:787; 1996 But how to dose to maximize effect/minimize
Ketorolac in Postop. Infants
Randomized, blinded, placebo-control study of
ketorolac pharmacokinetics, safety and efficacy
Infants 6-18 months admitted following surgery IRB approval/ Informed parental consent Exclusions:
History of gi bleeding or coagulopathy (infant or family)
Hepatic/renal impairment
Ketorolac Kinetics in Infants
Why stereo-specific kinetics? Kauffman and Hamunen reported differences
in isomer kinetics in children
Animal studies suggest the S- isomer more
potent analgesic
Isomer relation to toxicity – renal, GI,
hematologic unknown
Ketorolac in 6-18 mon infants
Ketorolac in Postop. Infants 6-18 m
Ketorolac Kinetics in Infants 2-6 mo R-isomer on left, S- on right side
Ketorolac in Postop. Infants
S (-) ketorolac cleared rapidly like in children Plasma concentration below "therapeutic" by
No respiratory , renal or hepatic problems
Surprising finding of no change in morphine
Pharmacokinetic – S-isomer gone quickly Other reasons – nursing care change?
Care Dilemma: Another Non-Pharmacologic Option
• Acupuncture – a complimentary modality
Enhances circulation of life energy (Qi) One mechanism involves endorphin system No drug interaction issues
• Anecdotal use in 6-10 infants over past
year aided in weaning ventilation and excessive sedative/opiate medications
Needs systematic study
Multimodal therapy may be a good option to
minimize undesired side effects
Opiate – use low doses and titrate Ketorolac – single dose did not cause problems,
but many unknowns still for repeated doses; would S-isomer be best since clearance is rapid even in infants?
Nonpharmacologic adjuncts
Sucrose if applicable Non-nutritive sucking/swaddling Acupuncture
Source: http://pedspainmedicine.org/wp-content/uploads/meetings/2014/syllabus/submissions/Developmental%20Pharmacokinetics_ALynn.pdf
Health Care for Women International, 23:98–118, 2002Copyright © 2002 Taylor & Francis0739-9332 /02 $12.00 + .00 CHILDBIRTH CARE-SEEKING BEHAVIOR IN CHIAPAS Linda M. Hunt, PhD Department of Anthropology and Julian Samora Research Institute, Michigan State University, East Lansing, Michigan, USA Namino Melissa Glantz, BA
Methodology articleA recombinase system facilitates cloning of expression cassettes in the ciliate Tetrahymena thermophilaThomas Weide*1, Ulrike Bockau2,3, Angelika Rave2, Lutz Herrmann2,4 and Marcus WW Hartmann*2 Address: 1Universitaetskliniken Muenster (UKM), Abteilung für Molekulare Nephrologie, Domagkstr. 3a, D-48149 Muenster, Germany, 2Cilian AG, Johann-Krane-Weg 42, D-48149 Muenster, Germany, 3Institut für allgemeine Zoologie und Genetik, Universitaet Muenster, Schloßplatz 5, D-48149 Muenster, Germany and 4Provendis GmbH, Eppinghofer Str. 50, 48468 Muelheim an der Ruhr, Germany